Introduction
Primary small bowel adenocarcinoma (PSBA) is rare
and arises in the duodenum in more than a half of cases (1). Thus, adenocarcinoma in the jejunum is
extremely rare. It has been reported that PSBA accounts for ~2% of
gastrointestinal tumors and that PSBA originates in the duodenum in
272/523 (52.0%), jejunum in 98/523 (18.7%), ileum in 90/523
(17.2%), and unspecified sites in 63/523 (12.0%) of patients
(1). Clinical symptoms of PSBA
include abdominal pain, bleeding, vomiting, loss of appetite and
jaundice (2). For the treatment of
PSBA, resection of the tumor, chemotherapy and radiation are
performed alone or in combination (2). If it is in the early stage, endoscopic
mucosal resection is also performed. The prognosis for PSBA is
poor, predominantly due to the delay in detection. The present
study describes a case of advanced adenocarcinoma with adenoma in
the jejunum of an elderly male. The family of the patient provided
written informed consent. This study was approved by the Ethics
Committee of Toyooka Hospital (Toyooka, Japan).
Case report
Case presentation
A 70-year-old male presented at the Asago-Yanase
Medical Center, (Asago, Japan) due to upper abdominal discomfort
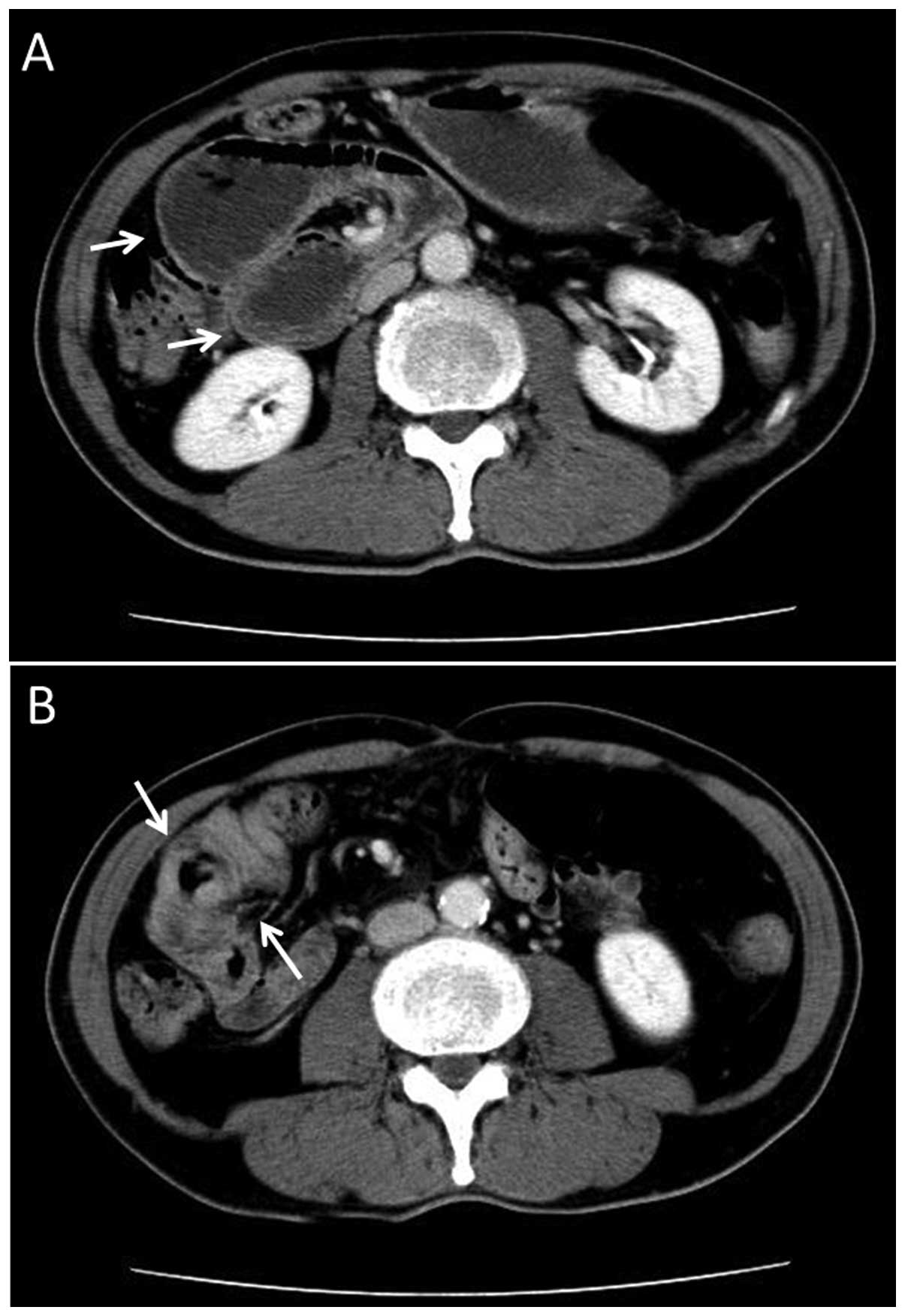
and dehydration lasting for three months. Contrast computed
tomography scans revealed severe dilatation of the stomach,
duodenum and upper section of the jejunum, and also revealed a
tumor in the jejunum (Fig. 1). The
tumor had induced wall thickening around almost the entire
circumference of the jejunum at about 50 mm towards the anus from
the ligament of treitz. Serologically, the carcinoembryonic antigen
and carbohydrate antigen 19-9 titers were found to be within the
normal limits.
Tumor resection
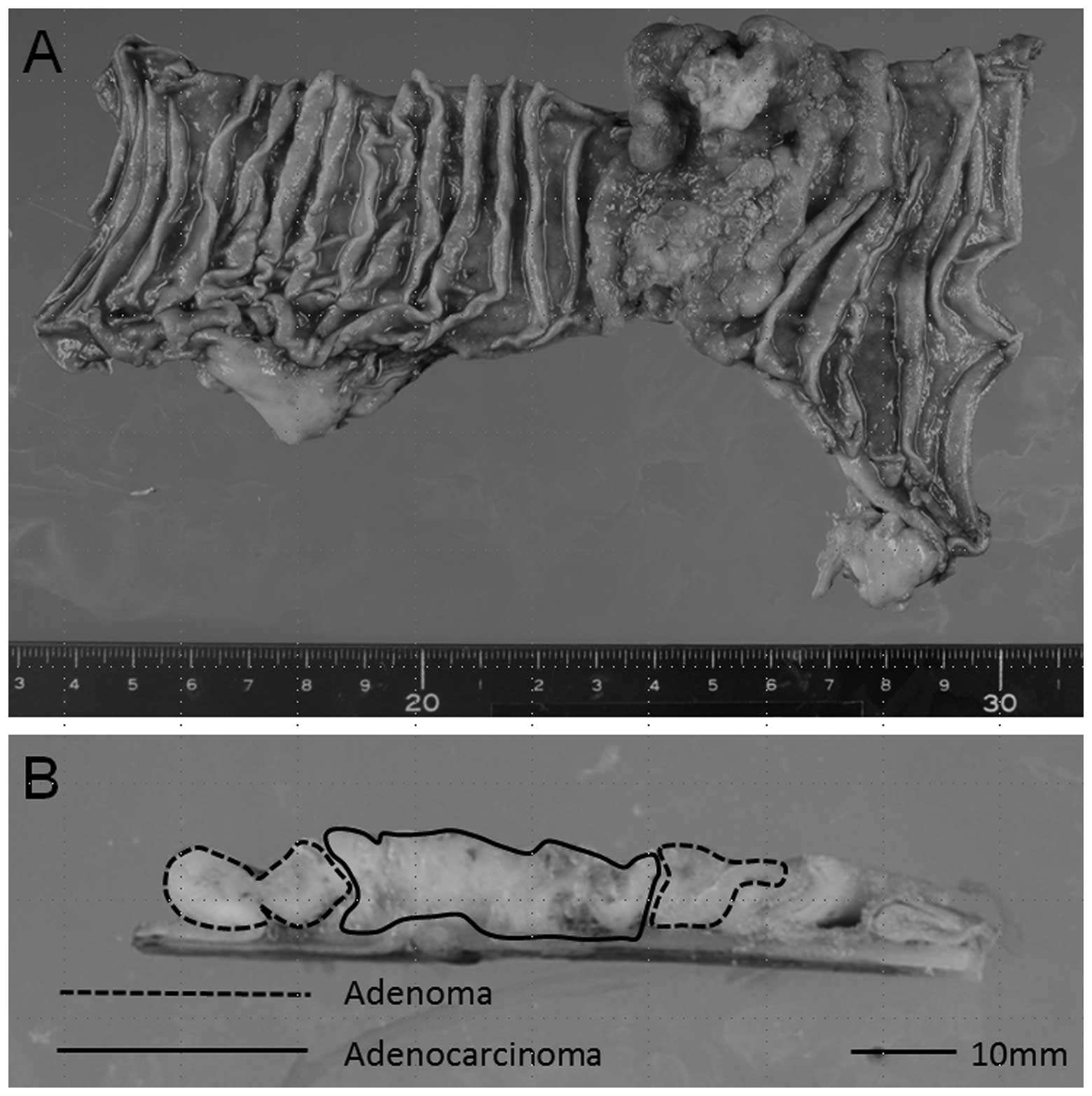
The tumor was resected and a pathological
examination of the tumor was performed. Macroscopically, the tumor
was 60×52 mm and was classified as Borrmann type 2 (Fig. 2A). Histologically, the tumor
contained areas of adenoma and adenocarcinoma tissue (Figs. 2B and 3). The adenocarcinoma was found to be in
the center of the tumor, while the adenoma was at the edge
(Fig. 2B). In the adenocarcinoma
area, the carcinoma showed various differentiating subtypes of
adenocarcinoma, including mucinous adenocarcinoma,
well-differentiated tubular adenocarcinoma, moderately
differentiated tubular adenocarcinoma and poorly differentiated
adenocarcinoma. Furthermore, the tumor had invaded the subserosa
and had metastasized into the regional lymph nodes.
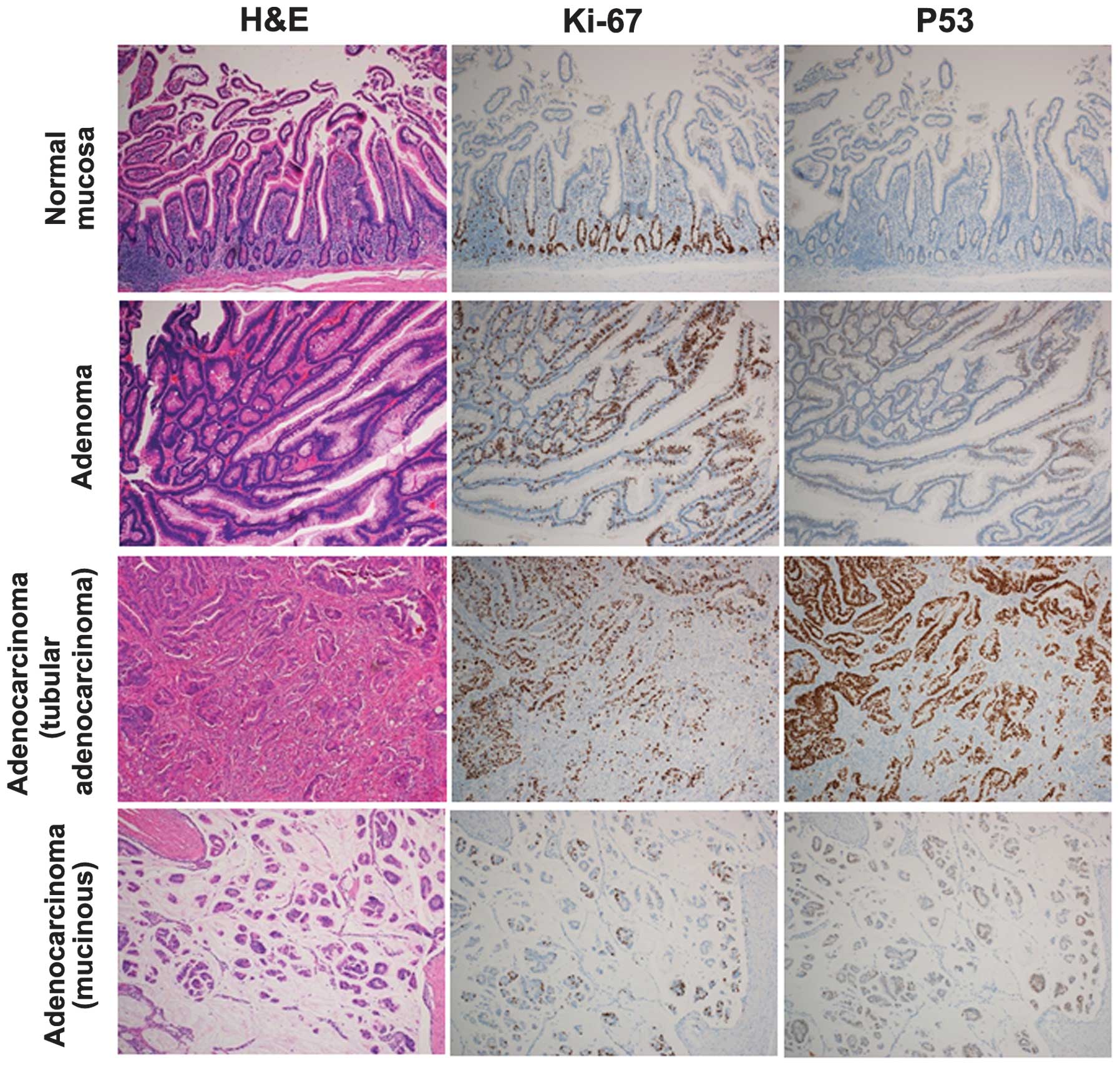
Immunohistological analysis
The tumor was immunohistologically analyzed for the
expression of P53 and Ki-67. As shown in Fig. 3, in the normal mucosa of the
jejunum, there were no P53-expressing epithelial cells and the
Ki-67-expressing epithelial cells primarily formed a regular
pattern at the base of the crypts. In the adenoma tissue, there was
a greater number of Ki-67-expressing epithelial cells compared with
the normal mucosa, and the cells were distributed in an irregular
pattern. Certain adenoma cells expressed a low level of P53. In the
adenocarcinoma tissue, there was a greater number of
Ki-67-expressing epithelial cells compared with the adenoma tissue,
and the adenocarcinoma tissue strongly expressed P53. Furthermore,
in the adenocarcinoma, there were a greater number of Ki-67- and
P53-expressing cells in the tubular adenocarcinoma area than in the
mucinous adenocarcinoma area.
Discussion
PSBA is a very rare condition. PSBA accounts for ~2%
of all cases of gastrointestinal cancer, while colorectal tumors
account for >52% of gastrointestinal carcinoma cases (3,4). Verma
and Stroehlein (1) analyzed 523
cases of SBA at the MD Anderson Cancer Center over a period of 60
years between 1944 and 2003 (1).
The mean age at the time of admission was 54 ± 13 years old (range,
21–87) and the male to female ratio was 58:42. With regard to the
location of the tumors, 272 were duodenal, 98 were jejunal, 90 were
ileal and 63 were not specified (1). Hong et al (2) investigated PSBA in 53 patients in
Korea. The mean age of the patients was 63 years (range, 26–84),
with 79.3% being >50 years old. The male to female ratio was
54.7:43.3 and 73.6% of the tumors were located in the duodenum,
13.2% in the jejunum and 13.2% in the ileum (2). Misawa et al (5) also analyzed 116 cases of PSBA in the
jejunum and ileum between 2005 and 2010 in Japan (5). The mean age of the patients was 60.8
years old, and the male to female ratio was 65:35. With regard to
the location of the tumor, 54% were located in the jejunum, while
46% were located in the ileum. These studies all showed a similar
pattern, with the duodenum being the main site of occurrence and
with more adenocarcinomas arising in the duodenum than in the
jejunum and ileum combined. Furthermore, the mean age of the
patients at the time of admission was 50–60s and the male to female
ratio was male dominant (1,2,5). In
the present case, the patient was in his 70s and male, which is
consistent with the previous reports.
Adenoma of the small bowel was also reported by
Perzin and Bridge (6), who analyzed
392,000 surgical pathology cases over a 62-year period. A total of
51 cases of small bowel tumor containing adenomatous epithelium
were found. Among the 51 patients, 18 had adenomas and 33 had
tumors that contained adenoma and carcinoma (6). These findings suggest that the
adenoma-adenocarcinoma sequence may occur in the small bowel as
well as in the colon and rectum. In 42 cases, the tumors arose in
the duodenum or consisted of multiple lesions, including duodenal
lesions, while six were in the jejunum and three were in the ileum.
Among the six jejunal cases, the adenocarcinoma existed with
adenoma in four of the cases and without adenoma in two of the
cases. In the four cases in which the carcinoma and adenoma
coexisted, one case exhibited ulcerative carcinoma with a zone of
adenoma at the edge, similar to that observed in the present
case.
Nishiyama et al (7) and Arai et al (8) reported that 40–50% of cases of PSBA
overexpress the p53 protein, suggesting that p53 may have a major
role in the progression of carcinoma of the small bowel (7,8). In
the present case, no p53-positive epithelial cells were found in
the normal mucosa; however, p53-expressing cells were observed in
the adenoma tissue and the level of p53 expression and the number
of p53-expressing cells was higher in the adenocarcinoma tissue,
consistent with previous findings (7,8).
Moreover, in the present case, the number of Ki-67 expressing cells
was observed to be higher in the adenoma tissue compared with the
normal mucosa, and higher in the adenocarcinoma tissue compared
with the adenoma tissue. This pattern of p53 and Ki-67 expression
suggests that p53 may have a crucial role in the progression from
normal mucosa to adenocarcinoma through to adenoma.
The prognosis for PSBA is poor predominantly due to
delay in the detection of the tumor. However, recent developments
have been made in capsule and double balloon endoscopy (9,10), and
the use of a combination of these tools and imaging examinations
(including computed tomography, magnetic resonance imaging and
positron-emission tomography) should make it possible to detect
PSBA in the early stage, allowing the tumor to be resected
endoscopically.
Acknowledgements
The authors would like to thank Ms. K. Ando
(Department of Stem Cell Disorders, Kansai Medical University,
Moriguchi, Japan), Mr. Y. Tanaka (Chugai Pharmaceutical Co. Ltd.,
Tokyo, Japan) and Mr. H. Eastwick-Field for their assistance with
the manuscript. The authors would also like to thank Mr. F.
Kawakami, Ms. H. Ogaki, Mr. K. Nagaoka, Ms. T. Kuge and Ms. S.
Eriguchi (Toyooka Hospital, Toyooka, Japan) for their technical
assistance.
References
|
1
|
Verma D and Stroehlein JR: Adenocarcinoma
of the small bowel: a 60-yr perspective derived from M. D. Anderson
Cancer Center Tumor Registry. Am J Gastroenterol. 101:1647–1654.
2006.
|
|
2
|
Hong SH, Koh YH, Rho SY, et al: Primary
adenocarcinoma of the small intestine: presentation, prognostic
factors and clinical outcome. Jpn J Clin Oncol. 39:54–61. 2009.
|
|
3
|
Jemal A, Murray T, Ward E, et al: Cancer
statistics, 2005. CA Cancer J Clin. 55:10–30. 2005.
|
|
4
|
Schottenfeld D, Beebe-Dimmer JL and
Vigneau FD: The epidemiology and pathogenesis of neoplasia in the
small intestine. Ann Epidemiol. 19:58–69. 2009.
|
|
5
|
Misawa S, Horie H, Kumano H, et al: A
clinicopathological study of 10 cases of primary small bowel
adenocarcinoma. Nihon Shokakibyo Gakkai Zasshi. 108:429–435.
2011.(In Japanese).
|
|
6
|
Perzin KH and Bridge MF: Adenomas of the
small intestine: a clinicopathologic review of 51 cases and a study
of their relationship to carcinoma. Cancer. 48:799–819. 1981.
|
|
7
|
Nishiyama K, Yao T, Yonemasu H, Yamaguchi
K, Tanaka M and Tsuneyoshi M: Overexpression of p53 protein and
point mutation of K-ras genes in primary carcinoma of the small
intestine. Oncol Rep. 9:293–300. 2002.
|
|
8
|
Arai M, Shimizu S, Imai Y, et al:
Mutations of the Ki-ras, p53 and APC genes in adenocarcinomas of
the human small intestine. Int J Cancer. 70:390–395. 1997.
|
|
9
|
Espín RG, Fuentes E, Espín MI, et al:
Small bowel adenocarcinoma diagnosed by double balloon enteroscopy
in a patient with nonpolyposis colorectal cancer. Rev Esp Enferm
Dig. 103:373–374. 2011.
|
|
10
|
Cobrin GM, Pittman RH and Lewis BS:
Increased diagnostic yield of small bowel tumors with capsule
endoscopy. Cancer. 107:22–27. 2006.
|