Introduction
Malignant mesothelioma is a rare type of tumour,
which is derived from mesothelial cells of the serosal surfaces of
body cavities. There is currently no effective standard treatment
for mesothelioma; its prognosis is poor with the majority of
patients succumbing 12–17 months following diagnosis (1). In addition, resistance to all
treatment modalities is a typical feature of mesothelioma (2).
The association of all forms of malignant
mesothelioma with asbestos exposure has been well documented
(3,4). This neoplasm is similar to a carcinoma
with regard to its mode of spread, with metastases occurring
predomimantly by direct invasion into adjacent tissue, however,
also via lymphatic and haematogenous routes. Distant metastasis are
most common with the sarcomatous variant (5) whereas, metastatic tumours of the oral
cavity are rare. Only four cases of an oral gingiva metastasis from
diffuse malignant pleural mesothelioma were identified in the
English language literature using a PubMed search (6–9). To
the best of our knowledge, this is the first report regarding the
metastasis of mesothelioma to the maxillary gingiva. Patient
provided written informed consent.
Case report
A 62-year-old male was referred to the physicians at
the Department of Dentistry and Maxillofacial Surgery at the Osaka
Red Cross Hospital (Osaka, Japan), in November 1996, with a
two-month history of progressive shortness of breath on exertion.
Clinical and radiographic examination revealed a left-sided pleural
effusion, which was drained successfully. A chest radiograph and
computed tomography demonstrated the presence of a mass in the left
lung field, and a rigid bronchoscopy and open pleural biopsy showed
the lesion to be a diffuse mesothelioma. At that time, the patient
commenced radiotherapy (total dose, 40 Gy). However, two months
after the initial presentation, the patient was referred to the
Department of Dentistry and Maxillofacial Surgery, Osaka Red Cross
Hospital(Osaka, Japan) with a large, painless mass on the maxillary
gingiva. This mass had been present and growing gradually for two
weeks. On examination a semi-hard, haemorrhagic lesion was found
surrounding the molar teeth, and extending to the buccal and
lingual aspects of the alveolar region (Fig. 1). The mobility of the affected teeth
was good and radiographic examination revealed loss of the crestal
bony architecture. An incisional biopsy was performed under local
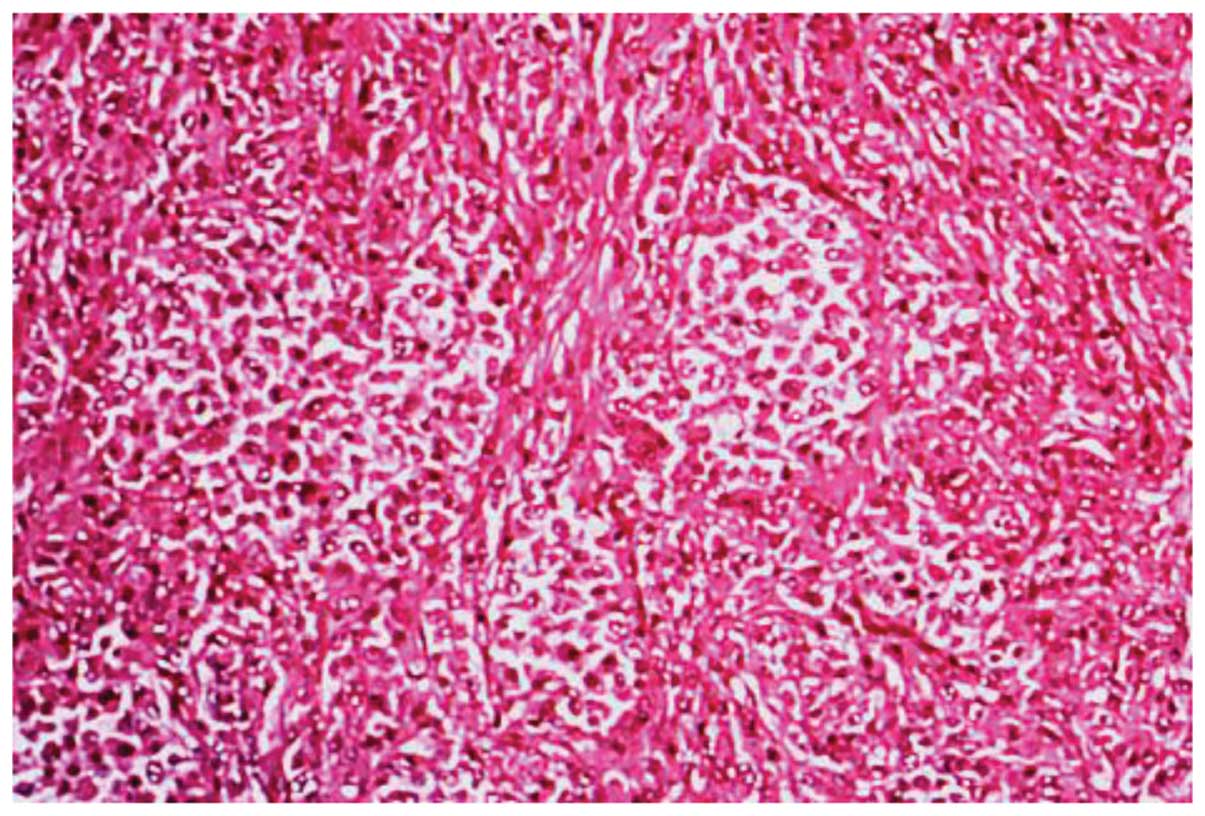
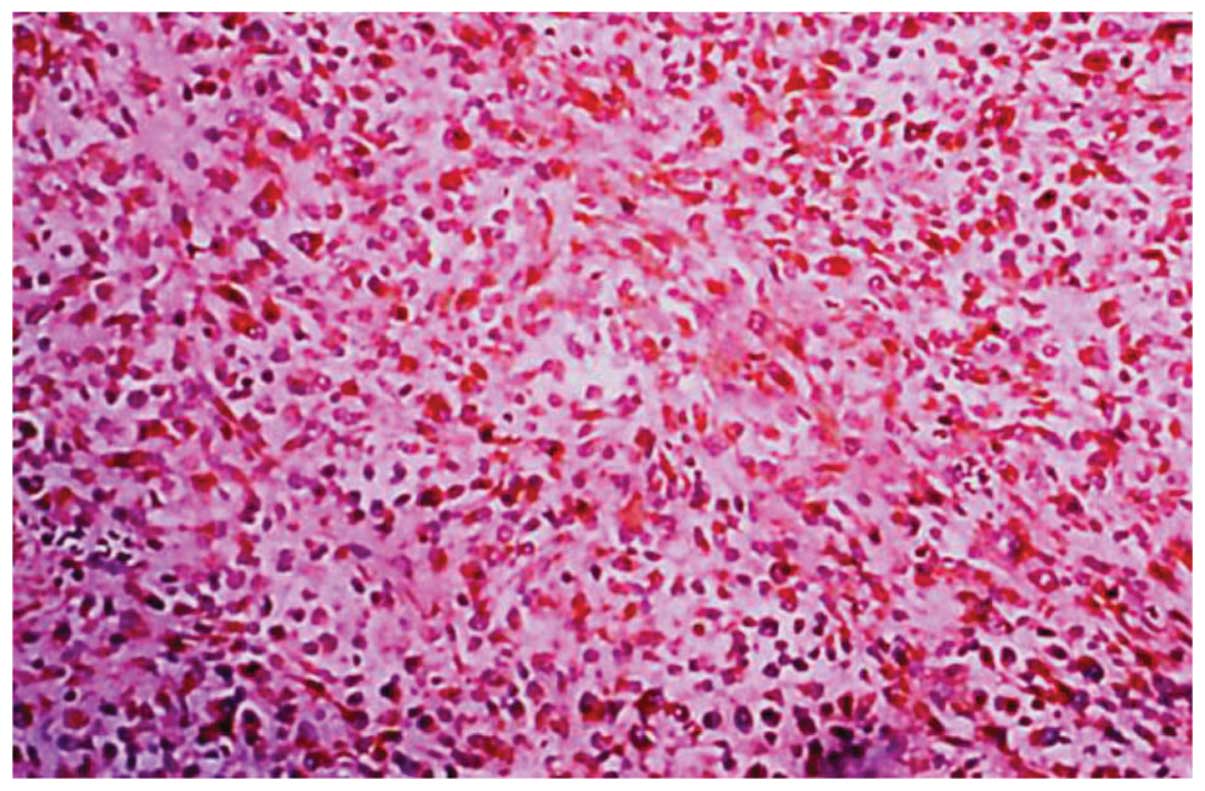
anaesthetic, and histology of the excised specimen showed a
mixed-type diffuse mesothelioma with poorly differentiated
epithelial and spindle cells (Fig.
2). The histological appearances of the biopsy specimen were
identical to those that were observed in the previous pleural
biopsy and immunocytochemistry indicated a sarcomatous, rather than
carcinomatous, pattern with strong positivity for vimentin
(Fig. 3). Focal positivity for
cytokeratin, and negative reactions for carcinoembryonic antigen
and epithelial membrane antigen were observed and an incisional
biopsy was subsequently conducted. The tumour increased rapidly and
the patient was unable to eat, thus, the tumour was removed to
improve quality of life (QOL). The excised specimen revealed a
solid semi-hard tissue mass (size, 30×25×20 mm), which was
white-yellow in colour on the cut surface. Despite surgery, the
patient succumbed 35 days later following deterioration of his
medical condition.
Discussion
Since 1960, when Wagner et al (3) demonstrated a high incidence of
mesothelioma among employees working with asbestos in the Cape
Province of South Africa, increasing attention has been paid to
this type of tumour, and numerous reports and reviews of
mesothelioma have appeared in the medical literature (10,11).
Mesothelioma tend to present in adults, predominantly affecting
individuals aged between 50 and 70 years, and occurs marginally
more commonly in males than females (12). It arises from serosal surfaces and
is approximately three times more common in the pleural cavity
compared with the peritoneal cavity. The association between
asbestos exposure and the development of mesotheliomas in
industrial countries has been recognized (13). Previous investigations have
hypothesized that longer amphibole fibres, rather than the shorter
fibre types, harbor an increased potential to induce the formation
of mesotheliomas (12).
Furthermore, a prolonged latency period of 20–40 years following
asbestos exposure and prior to the development of overt disease has
also been recognized (13). In the
present case, the patient was an industrial employee with a
prolonged history of asbestos exposure (~24 years).
There are three common histological types of
mesothelioma; epithelial (1),
fibrous (2) and mixed (3), which demonstrates the close
association between the epithelial and fibrous components. The
epithelial type is the most common variant of diffuse malignant
mesothelioma and is predominantly composed of flattened or cuboidal
epithelioid cells, which form a tubular and papillary pattern.
Mixed types of mesotheliomas appear as a mixture of epithelial and
fibrous elements, resulting in a biphasic pattern, which at times
may appear similar to synovial sarcoma. However, location, specific
stains, immunohistochemical staining and the less cellular nature
of mesotheliomas facilitate this differentiation (13). Differentiating between pleural
epithelial mesotheliomas and pulmonary adenocarcinomas remains a
diagnostic challenge for the pathologist. However, histochemical
stains (13), electron microscopy
and more recently, immunohistochemistry have been used to
distinguish between the two entities. The present case was
diagnosed as mixed-type by observation of positivity for vimentin
and cytokeratin via immunohistochemical staining.
There is currently no effective standard treatment
for mesothelioma and resistance to all treatment modalities is a
typical feature (2). Therefore, the
prognosis is poor and the majority of patients with diffuse
mesothelioma succumb to the disease within one or two years.
Metastasis does occur, however, does so at a
relatively late stage of the disease. Kannerstein and Churg
(14) reported metastases in 18/50
autopsy cases. In their series the most common sites of metastasis
were the regional lymph nodes, particularly those in the
mediastinum, abdomen and supraclavicular region, and the liver,
lung and bone marrow. Metastasis to the oral cavity is particularly
rare, with only six cases previously reported (6–9). Since
the primary site is not controlled, no case of treatment has ever
been found in metastatic lesions. In the present study, and the
majority of previous cases, the final diagnosis was determined by a
biopsy alone, with no radical treatment administered. To the best
of our knowledge, there is only one case available where the tumour
at the primary site was removed, however, this is a case of lost to
follow-up and it is unclear whether the primary site was really
restrained. The treatment method for metastasis to the oral cavity
has not been established and, considering the virulence of
malignant mesothelioma and its poor prognosis, the treatment for
metastasis must be determined via holistic assessment of the
invasiveness and dysfunction of surgery, length of survival and
QOL. In the present case, surgery on the primary site had to be
abandoned due to the possibility of metastases (similar to the
metastasis to the oral cavity).
In conclusion, as the total recovery of the patient
in the present report was not anticipated, the patient’s QOL was
considered and treatments were selected with the aim of improving
the oral condition. This modality of treatment was considered to be
effective as it enabled the patient to continue to eat until just
prior to sucumbing to the disease.
References
|
1
|
Boutin C, Schlesser M, Frenay C and Astoul
P: Malignant pleural mesothelioma. Eur Respir J. 12:972–981.
1998.
|
|
2
|
Sugarbaker DJ and Norberto JJ:
Multimodality management of malignant pleural mesothelioma. Chest.
113(Suppl 1): S61–S65. 1998.
|
|
3
|
Wagner JC, Sleggs CA and Marchand P:
Diffuse pleural mesothelioma and asbestos exposure in the North
Western Cape Province. Br J Ind Med. 17:260–271. 1960.
|
|
4
|
Hanna L and Macbeth F: Mesothelioma.
Practical Clinical Oncology. Hanna L, Crosby T and Macbeth F: 1st
edition. Cambridge University Press; Cambridge: pp. 328–333.
2008
|
|
5
|
Law MR, Hodson ME and Heard BE: Malignant
mesothelioma of the pleura: relation between histological type and
clinical behaviour. Thorax. 37:810–815. 1982.
|
|
6
|
Sproat CP, Brown AE and Lindley RP: Oral
metastasis in malignant pleural mesothelioma. Br J Oral Maxillofac
Surg. 31:316–317. 1993.
|
|
7
|
Stanley MK and Paul DF: Metastatic
mesothelioma of the oral cavity. Report of two cases Oral Surg Oral
Med Oral Pathol. 76:746–751. 1993.
|
|
8
|
Moser S, Beer M, Damerau G, Lübbers HT,
Grätz KW and Kruse AL: A case report of metastasis of malignant
mesothelioma to the oral gingiva. Head Neck Oncol. 3:212011.
|
|
9
|
García-Reija MF1, Matilla JM, De Paz A,
Sánchez-Cuéllar A and Verrier A: Unusual metastasis to the
mandibular alveolus of a malignant pleural mesothelioma.
Otolaryngol Head Neck Surg. 126:435–437. 2002.
|
|
10
|
Lumb PD and Suvarna SK: Metastasis in
pleural mesothelioma. Immunohistochemical markers for disseminated
disease. Histopathology. 44:345–352. 2004.
|
|
11
|
Ribak J, Lillis R, Suzuki Y, Penner L and
Selikoff IJ: Malignant mesothelioma in a cohort of asbestos
insulation workers: clinical presentation, diagnosis, and causes of
death. Br J Ind Med. 45:182–187. 1988.
|
|
12
|
Kane MJ, Chahinian AP and Holland JF:
Malignant mesothelioma in young adults. Cancer. 65:1449–1455.
1990.
|
|
13
|
Enzinger FM and Weiss SW: Mesothelioma.
Soft Tissue Tumors. 2nd edition. CV Mosby; St. Louis, MO: pp.
689–718. 1988
|
|
14
|
Kannerstein M and Churg J: Peritoneal
mesothelioma. Hum Pathol. 8:83–94. 1977.
|