Introduction
Leiomyomas are benign tumors composed of smooth
muscle and vascular collagenous tissue mainly occurring in the
uterus (1). Leiomyomas account for
<2% of soft tissue tumors, with an incidence rate of 8 per
million (2). Leiomyomas in the
spine are extremely rare, with only eight reported cases of
intraspinal leiomyoma (1–8). Epstein-Barr virus, the human
immunodeficiency virus, and immunosuppression may be cofactors in
the pathogenesis (9–11). Leiomyomas usually cause spinal cord
compression and must be surgically removed (1, 5). The
present study reviews a case of intraspinal leiomyoma causing
thoracic cord compression in a 19-year-old female. The clinical
data were retrospectively evaluated, and a literature review of all
other reported cases was performed.
Case report
A 19-year-old female presented to the Beijing
Tiantan Hospital (Capital Medical University, Beijing, China) with
numbness of the right lower extremities and severe progressive
weakness in the right leg that had been apparent for two months.
There was no reported history of other diseases. Written informed
consent was obtained from the patient’s family and study approval
was obtained from the Institutional Review Board of Beijing Tiantan
Hospital.
The neurological examination revealed a muscle power
grade of 3/5 (as classified by the Medical Research Council grading
system) (12) in the right leg and
a grade of 4/5 in the left leg. Deep and superficial sensation
below the T12 level was reduced. The muscle tone of the bilateral
legs was increased and the deep tendon reflexes had
hyper-excitability. Bilateral Babinski signs were present and
sphincter function was normal.
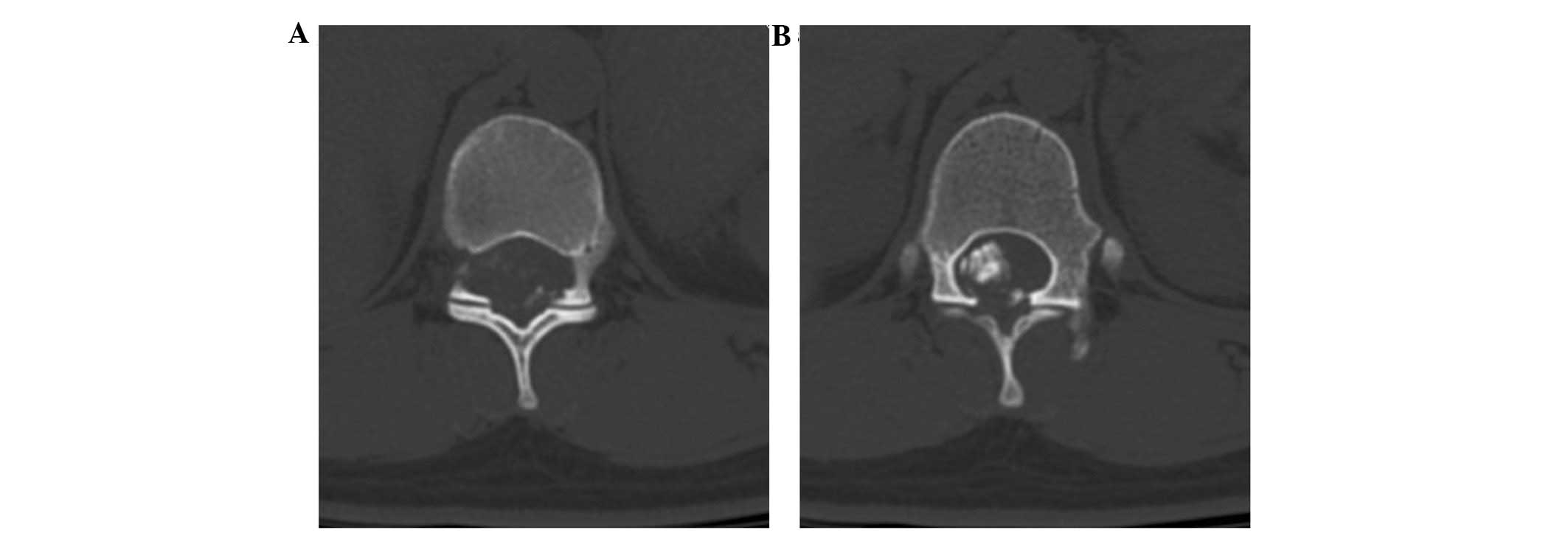
Abdominal computed tomography (CT) scans and an
ultrasound of the uterus demonstrated normal results. CT of the
spine disclosed an epidural mass with patchy calcification at the
T11–12 level, causing compression and deviation of the spinal cord.
An axial CT scan slice at the T11 level showed extension of the
neural foramina on the right, with foraminal enlargement (Fig. 1).
On magnetic resonance imaging (MRI), the tumor was
well-circumscribed, isointense on T1-weighted image and iso- to
hypointensity on T2-weighted image (Fig. 2). Following gadolinium
administration, the tumor showed heterogeneously marked
enhancement. The spinal cord was severely compressed and displaced
to the left, and cord edema was noted.
A T11–12 laminectomy was performed through the
posterior approach. The tumor was located in the epidural space,
with significant calcification and was firm and relatively
avascular. Due to the well-demarcated dissection plane and mild
adhesion to the dura, the tumor was completely removed.
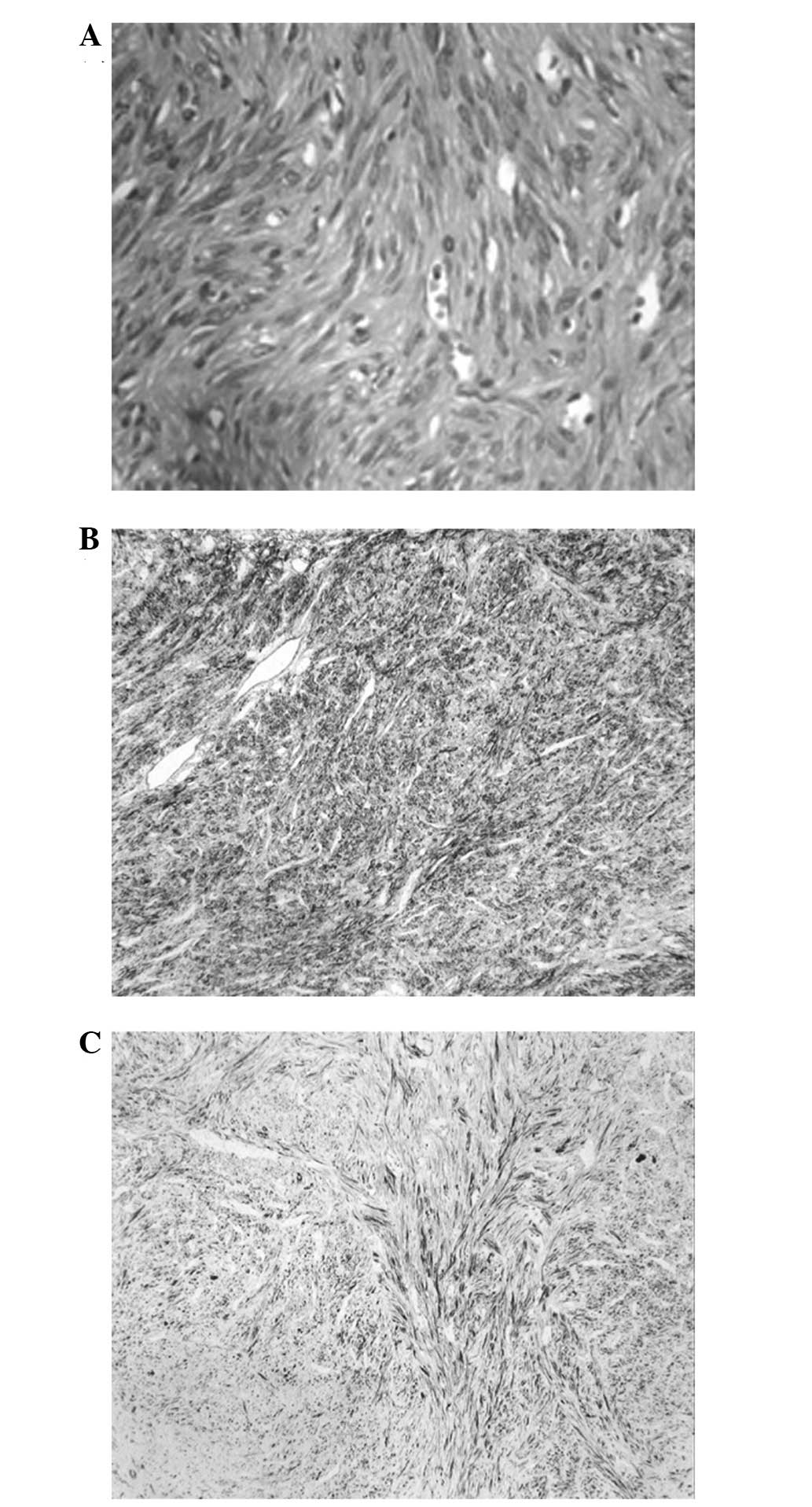
A histopathological examination revealed that the
tumor was composed of intersecting fascicles of acidophilic spindle
cells with blunt-ended nuclei, without significant cellular
pleomorphism or mitotic activity (Fig.
3A). There were no visible signs of cellular atypia or
necrosis. The immunohistochemical examinations revealed that the
tumor cells were positive for smooth muscle actin (SMA) (Fig. 3B) and desmin (Fig. 3C). The Ki67 index was <2%,
whereas staining for S-100 protein, estrogen and progesterone
receptors was negative. Taken together, all of these findings were
consistent with a diagnosis of leiomyoma.
As the nature of the tumor was benign, further
treatment was not recommended. The numbness in the right lower limb
of the patient was relieved following the surgical intervention and
the patient was discharged 1 week later. The patient was able to
walk unaided and no recurrence or regrowth of the tumor was
observed on follow-up MRI after 25 months.
Discussion
Without any histological malignant features,
leiomyomas rarely metastasize. Leiomyoma metastasis to the spine is
extremely rare. Only seven cases of benign metastasizing leiomyoma
of the spine have been reported in the English literature (1–7) since
the first case was described by Gatti et al in 1983
(3). Primary leiomyomas of the
spine are even rarer, with only one case reported by Steel et
al in 1993 (8). Table I summarizes the clinical features of
previous cases of intraspinal leiomyoma, together with the present
case.
 | Table ISummary of previously reported spinal
epidural leiomyoma cases. |
Table I
Summary of previously reported spinal
epidural leiomyoma cases.
| First author, year
(ref.) | Age,
years/gender | Location | Clinical
presentation | Duration of
illness | Origin | MRI findings | Treatment | Estrogen and
progesterone receptors | Follow-up |
|---|
|
|---|
| T1WI | T2WI | +GA |
|---|
| Gatti et al,
1983 (3) | 56/F | C2-3 | Neck pain | 2 months | Uterine | NA | NA | NA | GTR | NA | 18 months, CR, no
rec |
| Steel et al,
1993 (8) | 52/M | T3 | Back pain | 18 months | Primary spinal
leiomyoma | NA | NA | NA | GTR | NA | NA |
| Hekster et al,
1994 (4) | 43/F | C5-7 | Left shoulder and
hand pain | NA | Uterine | NA | NA | NA | STR + HT | NA | 13 years, ICR,
rec |
| Choi et al,
1997 (2) | 9/M | T4 | Paraparesis | 7 months | Right foot and left
axilla | Iso | Hypo | Heter | GTR | NA | NA |
| Joseph et al,
2003 (6) | 38/F | C3-7 | Progressive
spasticity | 12 months | Uterine | Hypo | Hypo | Heter | STR | Negative | 5 months, CR, no
rec |
| Alessi et al,
2003 (1) | 42/F | S2 | Saddle
anesthesia/back pain | 2 weeks | Uterine | Iso | Hypo | Heter | GTR + HT | Positive | 12 months, CR, no
rec |
| Vicente et al,
2005 (7) | 36/F | T6 | Paraparesis | NA | Uterine | NA | Iso to Hypo | NA | GTR | NA | NA |
| Jayakody et
al, 2011 (5) | 44/F | T5, T10 | Thoracic pain | 2 months | Uterine | NA | Iso to Hypo | NA | GTR | Positive | NA |
| Present study | 18/F | T11-12 | Right lower extremity
numbness | 2 months | Primary spinal
leiomyoma | Iso | Iso to Hypo | Heter | GTR | Negative | 23 months, CR, no
rec |
The pathogenesis of intraspinal leiomyoma is poorly
understood, but a few theories have been proposed. Steel et
al (8) hypothesized that
primary intraspinal leiomyoma may arise from blood vessel elements,
either from within the spinal dura or from the epidural vessels.
Other studies have suggested that the Epstein-Barr virus, the human
immunodifficiency virus and immunosuppression may be cofactors in
benign metastasizing leiomyoma (6,9–11).
In the present case, abdominal CT scans and an
ultrasound of the uterus were performed to search for the origin of
the metastasis. Although the results were normal, they were not
sufficient to lead to the conclusion that the spine was the primary
site of the tumor. It is well known that the spinal column and
epidural region can harbor neoplasms of various pathological forms
(8). The spinal tumor of the
present case may have been metastatic and the primary tumor may
have been clinically silent.
In the eight cases presented in the literature, the
patients ranged in age between 9 and 56 years, and there was a
female predominance (2 males and 6 females). All the lesions were
located in the epidural space, with three involving the cervical
segment, four involving the thoracic segment and one involving the
sacral segment.
The signs and symptoms of spinal epidural leiomyomas
are consistent with those of other epidural tumors. The clinical
presentation of a spinal leiomyoma can include radicular pain,
progressive or sudden weakness in the limbs, progressive spasticity
and saddle anesthesia when the cauda equina is involved (3,6,7). The
symptoms usually evolve over a period of weeks to years (1,6,8).
In the reported cases, the intraspinal leiomyomas
showed isointensity on T1-weighted images and iso- to hypointensity
on T2-weighted images (1,2,6). In
certain cases, heterogeneous enhancement, with well-defined tumor
margins, was detected following gadolinium administration. The
imaging features identified in the present case were consistent
with these previously reported characteristics.
Due to a lack of any particular features, definitive
pre-operative diagnosis may be challenging based only on CT and
MRI. Therefore, histopathological examination is required to
differentiate leiomyomas from other common epidural lesions,
including metastases, lymphoma and leiomyosarcoma.
The pathological features of the present case were
typical of leiomyoma. The tumor was composed of interlacing
fascicles of acidophilic cells, resembling a nerve-sheath tumor.
Immunohistochemistry is often a necessary adjunct to make a
differential diagnosis. Strong and diffuse immunostaining for SMA
and desmin has been recognized as the most suitable and reliable
diagnostic marker (4,5). No cellular atypia or necrosis was
observed in the present case. The Ki67 index was <2%, therefore
excluding the diagnosis of leiomyosarcoma. In the literature,
immunostains are occasionally positive for oestrogen and
progesterone receptors (1,5,13).
However, the present case was immuno-negative for each of these
receptors.
Due to the benign nature of the tumor, gross total
resection is the optimal treatment for patients with symptomatic
leiomyomas, in order to achieve a relatively good prognosis
(14). The majority of spinal
leiomyomas present with an intact capsule and are located in the
epidural space (4,5,8). It is
usually not difficult to achieve complete removal of the mass
whilst avoiding damage to the adjacent nerves. In the reported
cases, a gross total resection was achieved in seven patients and a
subtotal resection in one case. The subtotal removal in this case
was due to tight adherence of the tumor to the nerve roots.
Hormonal therapy is considered to be beneficial for
preventing tumor recurrence, particularly when the histological
examination is positive for the estrogen and progesterone receptors
(1). The mechanism behind this has
been indicated to be based on the feedback inhibition of estrogen
secretion (4,6,15–17).
In the literature, two cases underwent post-operative hormonal
therapy, and one of these cases experienced tumor recurrence as the
hormonal therapy was discontinued. The reason for the recurrence
may be due to hormonal dependency or hormonal fluctuations
(18,19).
The reported post-operative course ranged between 5
months and 13 years. Good outcomes were obtained following surgery
in 4/5 cases with follow-up evaluations. Seven cases experienced
gradual or complete functional improvement, and there was only one
tumor recurrence. In the present case, the spinal cord was severely
compressed, however, a good result was obtained following gross
total resection.
In conclusion, although intraspinal leiomyoma is
rare, it should be considered in the differential diagnosis of
other common epidural lesions in females. Due to the potential for
the patient to experience neurological recovery and be cured,
clinicians and neurosurgeons should be aware of this pathology.
Acknowledgements
The authors would like to thank the patient, and all
the physicians and staff who performed roles in this study.
References
|
1
|
Alessi G, Lemmerling M, Vereecken L and De
Waele L: Benign metastasizing leiomyoma to skull base and spine: a
report of two cases. Clin Neurol Neurosurg. 105:170–174. 2003.
|
|
2
|
Choi S, Levy ML, Krieger MD and McComb JG:
Spinal extradural leiomyoma in a pediatric patient with acquired
immunodeficiency syndrome: case report. Neurosurgery. 40:1080–1082.
1997.
|
|
3
|
Gatti JM, Morvan G, Henin D, et al:
Leiomyomatosis metastasizing to the spine. A case report. J Bone
Joint Surg Am. 65:1163–1165. 1983.
|
|
4
|
Hekster RE, Lambooy N, van Hall EV, Kazzaz
BA and van Rijssel EJ: Hormone-dependent spinal leiomyoma. Surg
Neurol. 41:330–333. 1994.
|
|
5
|
Jayakody S, Young K, Young B and Ferch R:
Serial spread of benign metastasizing leiomyoma to the thoracic
spine. J Clin Neurosci. 18:1135–1137. 2011.
|
|
6
|
Joseph V, Chacko G, Raghuram L and
Rajshekhar V: Benign metastasizing leiomyoma causing spinal cord
compression. Surg Neurol. 60:575–577. 2003.
|
|
7
|
Vicente LF, Maia AP, Carvalho MJ, et al: A
benign leiomyoma causing paraparesis: a case report and
histopathogenesis. Acta Obstet Gynecol Scand. 84:704–706. 2005.
|
|
8
|
Steel TR, Pell MF, Turner JJ and Lim GH:
Spinal epidural leiomyoma occurring in an HIV-infected man. Case
report J Neurosurg. 79:442–445. 1993.
|
|
9
|
Lee ES, Locker J, Nalesnik M, et al: The
association of Epstein-Barr virus with smooth muscle tumors
occurring after organ transplantation. N Engl J Med. 332:19–25.
1995.
|
|
10
|
McClain KL, Leach CT, Jenson HB, et al:
Association of Epstein-Barr virus with leiomyosarcomas in young
people with AIDS. N Engl J Med. 332:12–18. 1995.
|
|
11
|
Zevgaridis D, Tsonidis C, Kapranos N, et
al: Epstein-Barr virus associated primary intracranial leiomyoma in
organ transplant recipient: case report and review of the
literature. Acta Neurochir (Wien). 151:1705–1709. 2009.
|
|
12
|
Dyck PJ, Boes CJ, Mulder D, Millikan C,
Windebank AJ, Dyck PJ and Espinosa R: History of standard scoring,
notation, and summation of neuromuscular signs. A current survey
and recommendation. J Peripher Nerv Syst. 10:158–173. 2005.
|
|
13
|
Awonuga AO, Shavell VI, Imudia AN, et al:
Pathogenesis of benign metastasizing leiomyoma: a review. Obstet
Gynecol Surv. 65:189–195. 2010.
|
|
14
|
Hua W, Xu F, Mao Y, et al: Primary
intracranial leiomyomas: Report of two cases and review of the
literature. Clin Neurol Neurosurg. 11:907–912. 2009.
|
|
15
|
Britten JL, Malik M, Levy G, Mendoza M and
Catherino WH: Gonadotropin-releasing hormone (GnRH) agonist
leuprolide acetate and GnRH antagonist cetrorelix acetate directly
inhibit leiomyoma extracellular matrix production. Fertil Steril.
98:1299–1307. 2012.
|
|
16
|
Grigoriadis C, Papaconstantinou E, Mellou
A, et al: Clinicopathological changes of uterine leiomyomas after
GnRH agonist therapy. Clin Exp Obstet Gynecol. 39:191–194.
2012.
|
|
17
|
Ichigo S, Takagi H, Matsunami K, Suzuki N
and Imai A: Beneficial effects of dienogest on uterine myoma
volume: a retrospective controlled study comparing with
gonadotropin-releasing hormone agonist. Arch Gynecol Obstet.
284:667–670. 2011.
|
|
18
|
Banner AS, Carrington CB, Brooks Emory W,
et al: Efficacy of oophorectomy in lymphangioleiomyomatosis and
benign metastasizing leiomyoma. N Engl J Med. 305:204–209.
1981.
|
|
19
|
Horstmann JP, Pietra GG, Harman JA, Cole
NG and Grinspan S: Spontaneous regression of pulmonary leiomyomas
during pregnancy. Cancer. 39:314–321. 1977.
|