Introduction
Myeloid sarcoma (MS) is a tumor mass consisting of
myeloid blasts with or without maturation occurring at an
anatomical site other than the bone marrow (BM). The disease was
first described in 1811 by Burns (1). The term ‘granulocytic sarcoma’ was
first used by Rappaport in 1966 to describe MS (2) and the World Health Organization (WHO)
Classification of Tumours of Haematopoietic and Lymphoid Tissues
adopted the use of the term MS in 2008 (3). MS may precede, follow or occur
simultaneously with acute myeloid leukemia (AML). MS rarely
develops in patients with chronic myeloid leukemia, myelodysplastic
syndromes (MDS) or myeloproliferative neoplasms (MPN). Isolated MS
is rare and defined by the absence of a history of leukemia, MPN
and MDS, as well as a negative BM examination. Furthermore, MS has
been associated with various cytogenetic abnormalities. Only a
small number of cases with inversion of chromosome 16 [inv(16)] and the CBFβ/MYH11
fusion gene have been reported (4–13). The
present study describes a case of an isolated duodenal MS
associated with the CBFβ/MYH11 fusion gene followed
by AML progression. Patient provided written informed consent.
Case report
A 58-year-old female was admitted to the Department
of Gastroenterology at the Huashan Hospital (Shanghai, China) in
June, 2013 with the chief complaint of constantly feeling full and
abdominal pain for one month. At one week prior to admission, the
patient underwent an upper endoscopy (EGD) examination at Tai’an
City Hospital (Tai’an, China), which demonstrated a mass in the
duodenum. Biopsies of the lesion indicated a lymphoma. On admission
to the Huashan Hospital, decreased bowel sounds and tenderness upon
palpation in the left upper quadrant were notable during the
physical examination, however, no shifting dullness or
hepatosplenomegaly were identified. Upper gastrointestinal series
indicated incomplete obstruction of the descending duodenum. In
addition, computed tomography (CT) of the abdomen showed thickening
of the intestinal wall of hte descending duodenum with
heterogeneous contrast enhancement. A repeat EGD was performed
following admission, which revealed luminal stenosis of the
descending duodenum and multiple proliferative lesions that were
subsequently biopsied. The biopsy revealed blast cells, which were
positive for myeloperoxidase (MPO), cluster of differentiation
(CD)34, CD117 and CD43, and negative for CD20, CD3, CD2, CD79, CD5,
CD1a and CD56. Whereas, the BM aspiration and biopsy did not show
blasts. Laboratory studies, including blood routine, liver function
and renal function tests, as well as the partial thromboplastin and
prothrombin times, were within normal range. The patient was
diagnosed with duodenal MS and subsequently underwent an additional
BM aspiration 14 days following the initial BM examination. The
results showed hypercellularity with 30% myeloblasts, 23%
monoblasts and 2.5% eosinophils. Flow cytometry identified the
positive expression of CD34, CD117, CD15, CD33, CD38, HLA-DR, CD13,
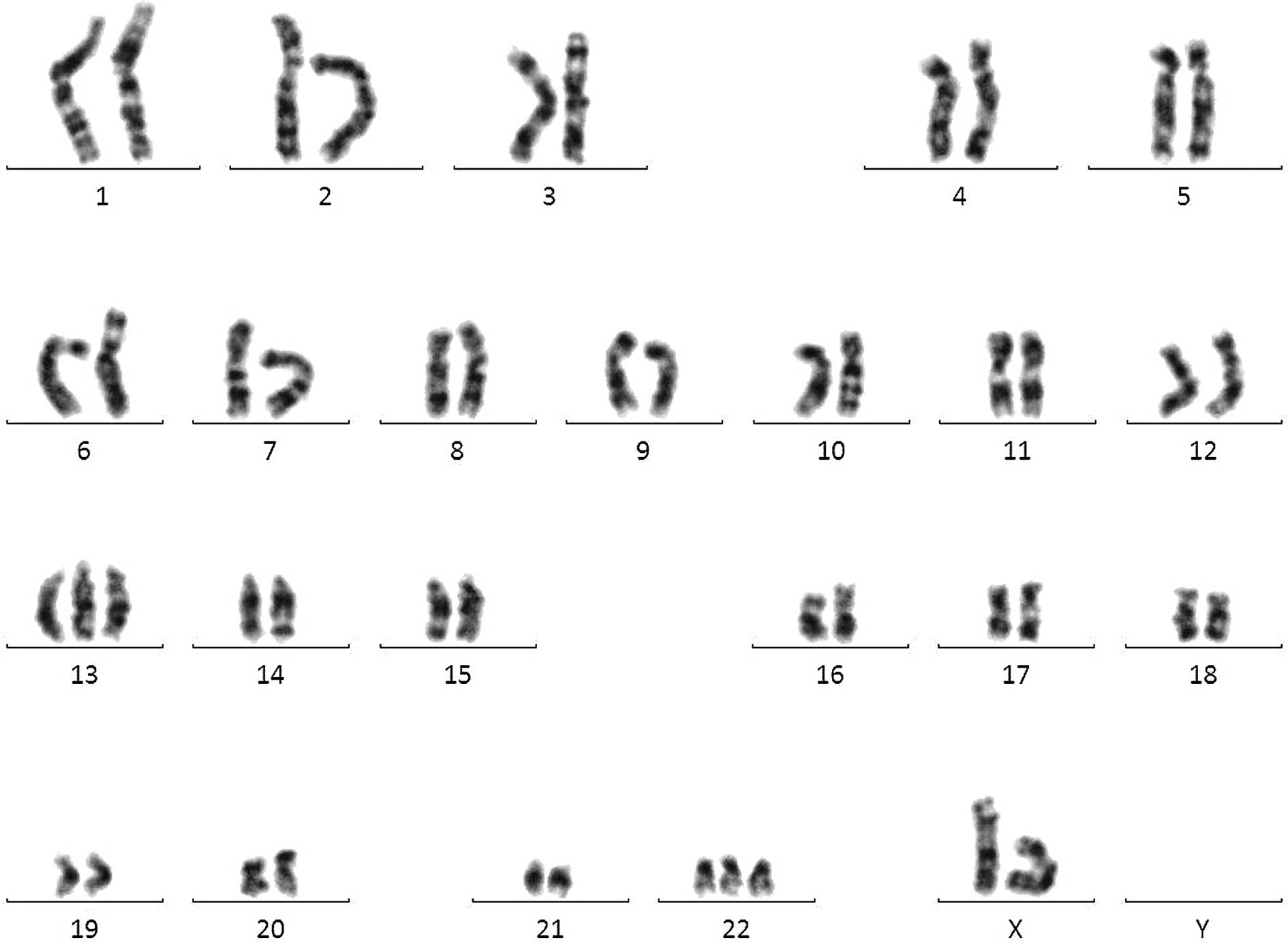
MPO and CD36, and cytogenetic analysis showed karyotype
48,XX,inv(16),+13,+22 (Fig. 1). Leukemia-associated fusion gene
analysis detected positive expression of CBFβ/MYH11,
and negative expression of BCR-ABL, TEL-ABL, PML-RARα,
PLZF-RARα, MLL-AF9, AML-ETO, E2A-PBX1, E2A-HLF, MLL-AF4,
MLL-AF6, MLL-AF10, MLL-ENL, MLL-AF17, MLL-AF1q, MLL-ELL, MLL-SEPT6,
NPM-RARα, NPM-MLF, AML1-MDS1/EVI1, AML1-MTG16,
AML1-EAP, FIP1L1-PDGFRA, SET-CAN, DEK-CAN, TEL-AML1, TEL-PDGFRB,
TLS-ERG and SIL_TAL1. Based on the abovementioned
results, the final diagnosis was AML, subtype M4 [according to the
French-American-British (FAB) classification system] associated
with the CBFβ/MYH11 fusion gene and duodenal MS. The
patient was administered anthracycline (14 mg/m2 losomal
doxorubicin intravenously on days one and two) and cytarabine (100
mg/m2 on days one to five) for one cycle of 28 days.
Following the induction of chemotherapy, the abdominal symptoms
disappeared and a BM examination showed complete remission (CR)
with only 0.5% blasts. The patient then received one further cycle
of losomal doxorubicin (28 mg/m2 intravenously on day
one) and cytarabine (100 mg/m2 cytarabine on days one to
seven) for one cycle of 28 days, as well as two courses of
high-dose cytarabine (2 g/m2 on days one, three and
five) for one cycle of 28 days for consolidation. A repeat CT scan
showed that there was no tumor in the abdomen and a BM examination
indicated complete hematologic and molecular remission. At present,
the patient is being followed up while undergoing regular
chemotherapy and no signs of disease relapse have been
observed.
Discussion
MS is a neoplastic proliferation of immature myeloid
precursors forming a tumorous mass, which occurs at anatomical
sites other than the BM. The incidence of MS is 2.5–9.1% among
patients with AML in Europe and the USA (14–16).
MS is most common in certain subtypes of AML, in particular M5, M4
and M2 according to the FAB classification system. Isolated MS,
also termed aleukemic, primary or de novo MS, is
particularly rare. Isolated MS has been described in limited case
reports and the incidence of isolated MS remains unclear.
Specific cytogenetic abnormalities and genetic
mutations have been reported in MS. The t(8,21)
translocation is the most common recurrent chromosomal abnormality
associated with MS. Furthermore, the AML1-ETO
(RUNX1-RUNX1T1) fusion gene is consistently detected in
patients with the t(8;21) translocation (17,18).
An additional common recurrent chromosomal abnormality in MS is
inv(16), which is associated with
the CBFβ/MYH11 fusion gene. In the majority of cases,
MS with these two recurrent cytogenetic abnormalities occur in AML
with the same cytogenetic abnormalities; these MS cases are the
extramedullary manifestation of AML. In rare cases, isolated MS
with a recurrent cytogenetic abnormality may develop.
The current study presents a rare case in which a
duodenal isolated MS, which was associated with the
CBFβ/MYH11 fusion gene and inv(16), rapidly progressed (within two weeks)
to overt AML. A search for similar case reports via the PubMed
database retrieved only 10 reported cases of isolated MS involving
inv(16) or the
CBFβ/MYH11 fusion (4–13).
Among these 10 cases, two cases were not included in the current
review. One of the two cases (4)
was an isolated MS with inv(16)
and 10.4% myeloblasts in the BM. According to the recommendation of
the WHO (2008), cases with inv(16)(p13.1;q22) and <20% BM blasts must
be diagnosed as AML (19). The
other case report (5) was MS
following an allogeneic hematopoietic stem cell transplantation
(Allo-HSCT). Prior to the Allo-HSCT, the patient was diagnosed with
AML with inv(16) and based on the
information, the MS appeared to be an extramedullary relapse of
AML. The remaining eight cases of isolated MS and the current study
are listed in Table I (6–13).
 | Table INine reported cases of isolated MS
associated with the CBFβ/MYH11fusion gene and/or inv(16)
AML. |
Table I
Nine reported cases of isolated MS
associated with the CBFβ/MYH11fusion gene and/or inv(16)
AML.
| Age, years | Gender | Karyotype | Fusion gene
detection | MS location | Progression to
AML | Reference |
|---|
| 49 | M |
49,XY,inv(16)(p13q;22),+6,+14,+22 | NA | Small intesine | Yes | 6 |
| 30 | M |
46,XY,inv(16)(p13q;22) | NA | Small intesine | Yes | 7 |
| 25 | M |
47,XY,inv(16)(p13;q22),+22 | Yes | Mesentery | No | 8 |
| 37 | M |
46,XY[3]47,XY,+9,inv(16)(p13;q22)[1]
48,XY,+9,inv(16)(p13;q22),+22[19]
49,XYY,+9,inv(16)(p13;q22),+22[2] | NA | Jejunum | Yes | 9 |
| 23 | F | 47,XX,+8,
inv(16)(p13;q22) | NA | Breast | Yes | 10 |
| 50 | F | inv(16)(p13;q22) | Yes | Small bowel | No | 11 |
| 14 | M |
46,XY,t(16;16)(p13;q22)7q− | Yes | Mesentery | No | 12 |
| 41 | M |
46,XY,inv(16)(p13;q22) | Yes | Small bowel, greater
omentum and peritoneum | No | 13 |
| 58 | F |
48,XX,inv(16)(p13;q22),+13,+22 | Yes | Duodenum | Yes | Current case |
Of the nine cases included in this study, the
isolated MS with CBFβ/MYH11 fusion and inv(16) was consistently identified in the
abdomen (eight out of nine cases). Furthermore, the intestinal
tract was the most commonly involved site, including the small
intestine and mesentery. It appears that the small intestine is a
relatively specific target for MS with the CBFβ/MYH11
fusion. Abdominal pain and/or intestinal obstruction are the most
common symptoms.
The diagnosis of MS in the setting of leukemia is
not complex. However, in the absence of a history of leukemia, the
diagnosis of MS becomes challenging. One study has shown that ~40%
of patients with isolated MS are initially diagnosed as other
conditions, most often as diffuse large B-cell lymphoma (20,21).
The diagnosis is based on morphological examination and
immunohistochemistry. The use of specific markers for myeloid
disease, such as MPO, CD43, lysozyme, CD33, CD117 and CD34, is
required to establish the diagnosis of MS. Other
immunohistochemistry markers may be used depending on the
differential diagnosis. The differential diagnosis for MS is broad,
including non-Hodgkin’s lymphoma, blastic plasmacytoid dendritic
cell neoplasm, histiocytic sarcoma and poorly differentiated
carcinoma.
Due to the rarity of isolated MS, the optimal
treatment has not yet been established. However, it is well known
that the delayed or inadequate treatment of isolated MS almost
always leads to AML (16). In the
current literature review, five of the nine patients with isolated
MS developed AML. Although the other four patients did not show
overt evidence for AML, AML clones were detected in the BM using
cytogenetic and/or molecular biological polymerase chain
reaction-based methods.
The current recommended treatment for isolated MS is
conventional AML-type chemotherapy protocols. This recommendation
is based on the observation of a markedly higher risk of
progression to AML in patients with isolated MS receiving localized
treatment compared with isolated MS patients receiving systemic
chemotherapy (16,22). Anthracycline and cytarabine are the
standard remission induction chemotherapy agents and the
consolidation treatment regimen is administered following CR as in
AML. The CR rate of AML with the CBFβ/MYH11 fusion is
reported to be between 81 and 93%, which is markedly higher than
the majority of other subtypes of AML (23,24).
The prognosis of AML with the CBFβ/MYH11 fusion and
inv(16) is optimistic compared
with other types of AML, with disease-free survival ranging between
48 and 63% (23,24). Allo-HSCT is therefore not the
first-line treatment option and is usually reserved for relapsed or
refractory cases. It remains unclear whether similar CR rates and
the optimal prognosis of MS with the CBFβ/MYH11
fusion can be predicted based on the current data concerning AML
with the CBFβ/MYH11 fusion.
In conclusion, in the present case, the patient
responded well to the standard induction therapy followed by the
high-dose cytarabine-based consolidation treatment. However, due to
the lack of experience regarding the treatment of this rare
disease, controlled prospective multicenter clinical trials are
considered to be important and necessary to guide treatment.
Acknowledgements
The authors would like to thank Dr Ling Mei for the
critical reading and editing of the manuscript. This study was
supported by the National Natural Science Foundation of China
(grant nos. NSFC 81170491 and NSFC 81170357) and the Shanghai
Municipal Health Bureau (grant no. 2010079).
References
|
1
|
Burns A: Observation of Surgical Anatomy,
Head and Neck. Thomas Royce and Co; Edinburg: pp. 364–366. 1811
|
|
2
|
Rappaport H: Tumours of the hematopoietic
system. Atlas of Tumour Pathology, Section III, Fascicle 8. Armed
Force Institute of Pathology; Washington, DC: pp. 241–243. 1996
|
|
3
|
Pileri SA, Orayi A and Falini B: Myeloid
sarcoma. WHO Classification of Tumours of Haematopoietic Lymphoid
Tissues. Swerdlow S, Campo E, Harris NL, et al: IARC Press; Lyon:
pp. 140–141. 2008
|
|
4
|
Xavier SG, Fagundes EM, Hassan R, Bacchi
C, Conchon M, Tabak DG, Spector N and Zalcberg IR: Granulocytic
sarcoma of the small intestine with CBFbeta/MYH11 fusion gene:
report of an aleukaemic case and review of the literature. Leuk
Res. 27:1063–1066. 2003.
|
|
5
|
Zaenker S, Schweyer S, Hasenkamp J,
Truemper L and Wulf G: Granulocytic sarcoma by AML M4eo (inv16)
after allogeneic stem cell transplantation without bone marrow
involvement. Case Rep Hematol. 2011:6929822011.
|
|
6
|
Russell SJ, Giles FJ, Thompson DS, Scanlon
DJ, Walker H and Richards JD: Granulocytic sarcoma of the small
intestine preceding acute myelomonocytic leukemia with abnormal
eosinophils and inv(16). Cancer Genet Cytogenet. 35:231–235.
1988.
|
|
7
|
Le Beau MM, Larson RA, Bitter MA, Vardiman
JW, Golomb HM and Rowley JD: Association of an inversion of
chromosome 16 with abnormal marrow eosinophils in acute
myelomonocytic leukemia. A unique cytogenetic-clinicopathological
association. N Engl J Med. 309:630–636. 1983.
|
|
8
|
Billio A, Pianezze G, Amato B and Fabris
P: ‘Isolated’ peritoneal granulocytic sarcoma with molecular and
chromosomal bone marrow involvement. Haematologica.
87:EIM012002.
|
|
9
|
Morel F, Herry A, Le Bris MJ, Le Calvez G,
Marion V, Berthou C and De Braekeleer M: Isolated granulocytic
sarcoma followed by acute myelogenous leukemia type FAB-M2
associated with inversion 16 and trisomies 9 and 22. Leukemia.
16:2458–2459. 2002.
|
|
10
|
Quitt M, Elmalach I, Dar H and Aghai E:
Isolated chloroma of breast preceding acute nonlymphatic leukemia.
Leukemia. 11:1995–1996. 1997.
|
|
11
|
McKenna M, Arnold C, Catherwood MA,
Humphreys MW, Cuthbert RJ, Bueso-Ramos C and McManus DT: Myeloid
sarcoma of the small bowel associated with a CBFbeta/MYH11 fusion
and inv(16)(p13q22): a case report. J Clin Pathol. 62:757–759.
2009.
|
|
12
|
Göhring G, Erlacher M, van Buiren M,
Jüttner E, Niemeyer CM and Schlegelberger B: Mesenteric chloroma
with t(16;16) followed by acute myelomonocytic leukemia with clonal
evolution. Cancer Genet Cytogenet. 179:162–164. 2007.
|
|
13
|
Alvarez P, Navascués CA, Ordieres C, Pipa
M, Vega IF, Granero P, Alvarez JA and Rodríguez M: Granulocytic
sarcoma of the small bowel, greater omentum and peritoneum
associated with a CBFβ/MYH11 fusion and inv(16) (p13q22): a case
report. Int Arch Med. 4:32011.
|
|
14
|
Neiman RS, Barcos M, Berard C, Bonner H,
Mann R, Rydell RE and Bennett JM: Granulocytic sarcoma: a
clinicopathologic study of 61 biopsied cases. Cancer. 48:1426–1437.
1981.
|
|
15
|
Breccia M, Mandelli F, Petti MC, D’Andrea
M, Pescarmona E, Pileri SA, Carmosino I, Russo E, De Fabritiis P
and Alimena G: Clinico-pathological characteristics of myeloid
sarcoma at diagnosis and during follow-up: report of 12 cases from
a single institution. Leuk Res. 28:1165–1169. 2004.
|
|
16
|
Bakst RL, Tallman MS, Douer D and Yahalom
J: How I treat extramedullary acute myeloid leukemia. Blood.
118:3785–3793. 2011.
|
|
17
|
Dusenbery KE, Howells WB, Arthur DC,
Alonzo T, Lee JW, Kobrinsky N, Barnard DR, Wells RJ, Buckley JD,
Lange BJ and Woods WG: Extramedullary leukemia in children with
newly diagnosed acute myeloid leukemia: a report from the
Children’s Cancer Group. J Pediatr Hematol Oncol. 25:760–768.
2003.
|
|
18
|
Tsimberidou AM, Kantarjian HM, Wen S,
Keating MJ, O’Brien S, Brandt M, Pierce S, Freireich EJ, Medeiros
LJ and Estey E: Myeloid sarcoma is associated with superior
event-free survival and overall survival compared with acute
myeloid leukemia. Cancer. 113:1370–1378. 2008.
|
|
19
|
Arber DA, Burnning RD, Le Beau MM, et al:
Acute myloid leukemia with recurrent genetic abnormalities. WHO
Classification of Tumours of Haematopoietic Lymphoid Tissues.
Swerdlow S, Campo E, Harris NL, et al: IARC Press; Lyon: pp.
110–123. 2008
|
|
20
|
Byrd JC, Edenfield WJ, Shields DJ and
Dawson NA: Extramedullary myeloid cell tumors in acute
nonlymphocytic leukemia: a clinical review. J Clin Oncol.
13:1800–1816. 1995.
|
|
21
|
Tóth E, Balint I, Deák B and Orosz Z:
Complex pathological diagnosis of granulocytic sarcoma: apropos of
a case. Pathol Res Pract. 198:55–57. 2002.
|
|
22
|
Antic D, Elezovic I, Milic N, Suvajdzic N,
Vidovic A, Perunicic M, Djunic I, Mitrovic M and Tomin D: Is there
a ‘gold’ standard treatment for patients with isolated myeloid
sarcoma? Biomed Pharmacother. 67:72–77. 2013.
|
|
23
|
Delaunay J, Vey N, Leblanc T, Fenaux P,
Rigal-Huguet F, Witz F, Lamy T, Auvrignon A, Blaise D, Pigneux A,
et al; French Acute Myeloid Leukemia Intergroup; Groupe Ouest-Est
des Leucémies Aiguës Myéoblastiques; Leucémies Aiguës
Myéoblastiques de l’Enfant; Acute Leukemia French Association and
Bordeaux-Grenoble-Marseille-Toulouse cooperative groups. Prognosis
of inv(16)/t(16;16) acute myeloid leukemia (AML): a survey of 110
cases from the French AML Intergroup. Blood. 102:462–469. 2003.
|
|
24
|
Dombret H, Preudhomme C and Boissel N:
Core binding factor acute myeloid leukemia (CBF-AML): is high-dose
Ara-C (HDAC) consolidation as effective as you think? Curr Opin
Hematol. 16:92–97. 2009.
|