Introduction
Focal fibrocartilaginous dysplasia (FFCD) is a rare,
paraneoplastic disease that presents in children and teenagers.
Less than 100 cases have been reported in the English literature
since the original description by Bell et al (1). Previous studies have reported cases of
lesions in the proximal tibia and distal femur, as well as lesions
in the upper extremities. However, to the best of our knowledge,
there are no reports of FFCD on the transverse process or the rib.
Thus, the present study is the first report of a case of FFCD in
the vertebra and the rib. The aim of this report is to testify that
FFCD may occur in tubular bones and flat bones.
Case report
A 38-year-old male (body mass index, 21.01)
presented at The First Affiliated Hospital of Nanchang University
(Nanchang, China) with pneumonia and lesions on the left first
thoracic vertebra, which were detected using chest computed
tomography (CT). The patient reported that he had experienced a
tolerable level of pain in the area three times during the previous
ten years, with no history of trauma. No other family members had
suffered from a similar condition. The initial consultation was
performed on 28/05/2013. Informed consent was obtained from the
patient.
Physical examinations revealed that the patient was
healthy and ambulated without difficulty. The patient exhibited a
full range of motion of the neck and upper extremities.
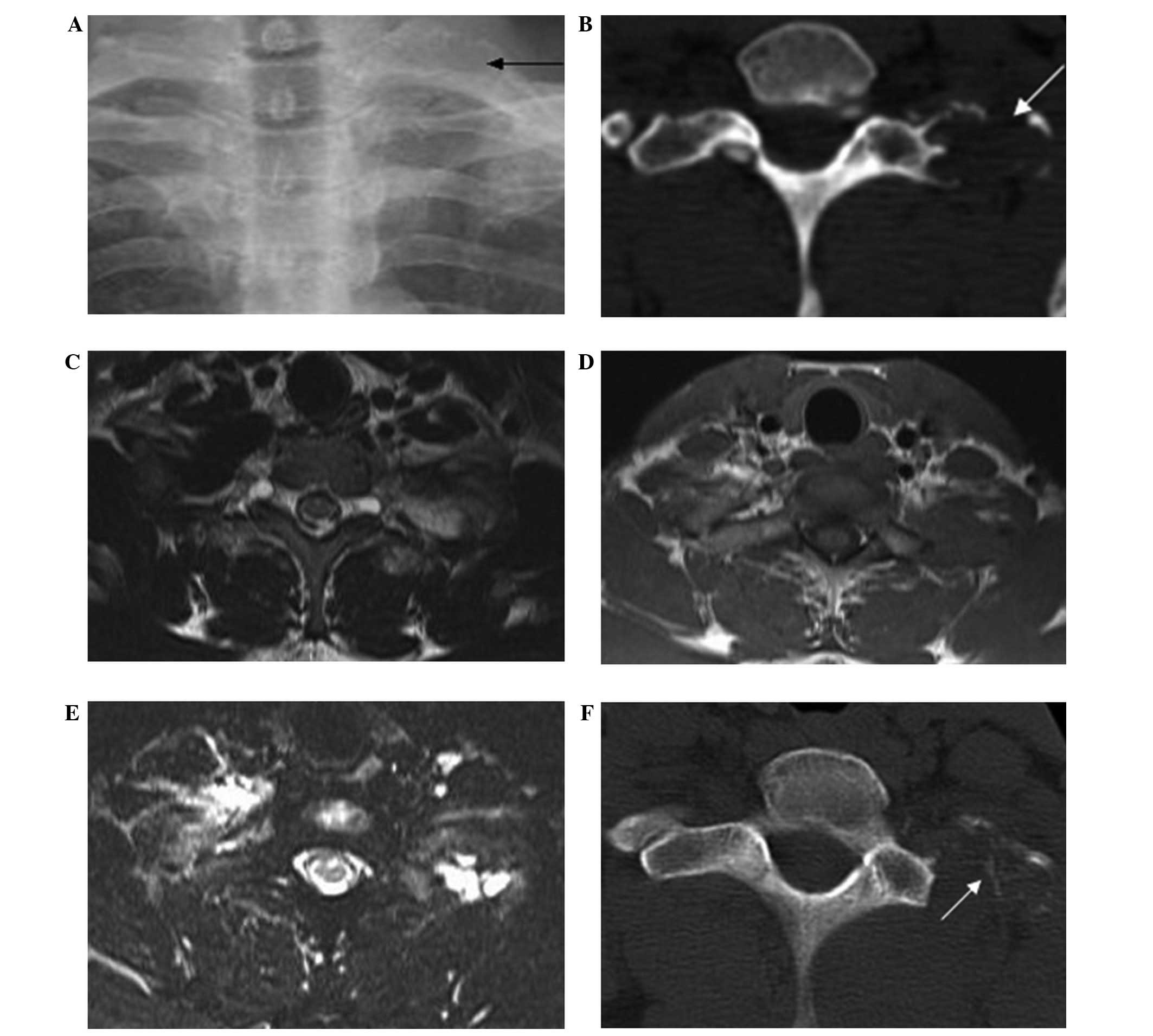
Furthermore, no masses were palpable. X-ray (Fig. 1A) and chest CT scans (Fig. 1B) were performed and revealed a
well-defined, unilateral, lucent and inflated lesion in the left
first transverse process and the costal head (estimated size,
2.2×2.4 cm). The two sides of the lesion, which connected with the
normal bony tissue, were sclerosing. In addition, the cortical bone
of the lesion was found to be thinning; however, there was no
periosteal reaction or cortical destruction. Magnetic resonance
imaging (MRI) demonstrated a low signal of the lesion in the
T1-weighted image (TE 10.0 and TR 581.0; Fig. 1C) and an intermediate signal in the
T2-weighted images (TE 130.0 and TR 4,710.0; Fig. 1D). A high signal was observed in the
lesion in the fat suppression images (TE 130.0 and TR 6,380.0;
Fig. 1E). Thus, the radiologists
proposed that it may be an aneurysmal bone cyst. A full 99mTC-MDP
scan showed that there was no sign of malignant transformation in
the patient’s skeletal system, and the results from the laboratory
examinations and the tumor markers, including α-fetoprotein,
carcinoembryonic antigen and cancer antigen 19-9, were all within
normal limits.
Curettage of the focal lesion and an incisional
biopsy were performed due to the possibility of the lesion being an
aneurysmal bone cyst. The surgery lasted 120 min and the estimated
blood loss was 200 ml. A frozen section obtained during surgery did
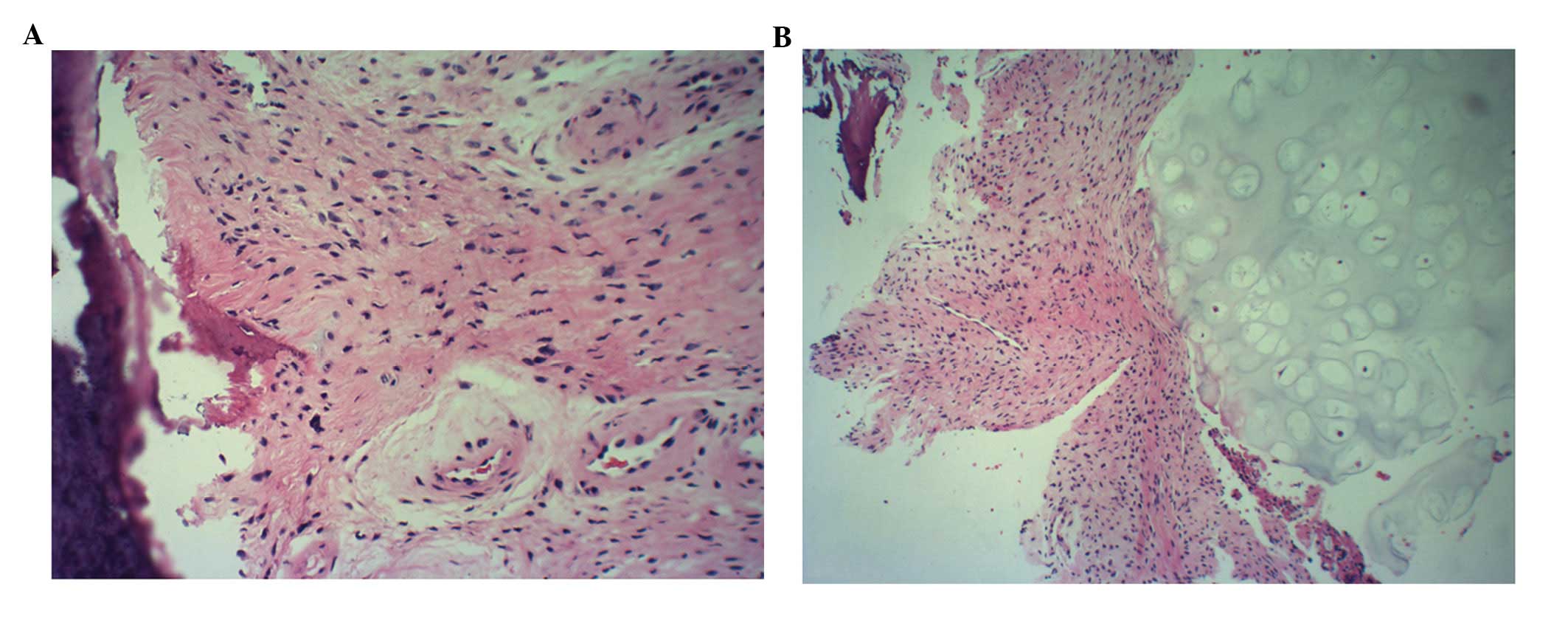
not provide a specific diagnosis. After one week, the pathologic
results from a specimen of the lesion (Fig. 2) demonstrated irregularly-shaped
bony trabeculae surrounded by numerous fibroblasts (Fig. 2A), which were detected using
hematoxylin and eosin (H&E) staining (magnification, ×200).
Furthermore, the cell stroma was observed to be composed of
relatively uniform spindle cells and cartilaginous components
without significant cellular atypia (H&E; magnification, ×100;
Fig. 2B). The patient was informed
of the findings and, as the patient only exhibited slight back
pain, no further treatment was administered and the patient was
closely observed.
Two months after surgery, the patient was followed
up. Chest CT (Fig. 1F) demonstrated
a patchy, high-density shadow in the primary lesion. The patient is
currently pain-free and is not prevented from performing any
activities. The patient will be followed up annually.
Discussion
FFCD is an uncommon, benign bone lesion that deforms
the long bones in children. FFCD predominantly occurs in the
proximal tibia and rarely occurs in the long bones of the upper
limbs. To the best of our knowledge, the present study is the first
study to report a case of FFCD on the transverse process of the
rib. Furthermore, the patients reported in previous studies have
all been adolescents or infants, with only Ohno et al
(2) and Hermann et al
(3) reporting cases of patients
aged >25 years; the current study presents the case of an adult
patient. FFCD lesions in the lower limbs usually present in
patients of a younger age (1,4–6), while
upper limb involvement usually occurs in older individuals
(6,7). The present study reported the case of
a 38-year-old male, thus, FFCD lesions in the vertebrae or ribs may
be more likely to present in post-adolescent or middle-aged
individuals. However, further investigations are required to assess
this hypothesis.
The lower extremities are the most frequent site for
FFCD; however, its pathogenesis is controversial. For example, Bell
et al (1) proposed that in
lesions of the tibia, failure of the mesenchymal anlage to
differentiate in the area of the pes anserinus, as well as the
persistence of a focus of fibrocartilage, may impair growth on the
medial aspect of the proximal tibia. Jouve et al (8) hypothesized that FFCD is a pathology of
the pes anserinus insertion, which interferes with its
physiological migration during growth through creating a
pseudo-epiphysiodesis. Langenskiöld (9) proposed that trauma during delivery may
be a predisposing factor by causing necrosis of the medial aspect
of the physis. However, the pathogenesis of lesions in the
transverse process or the rib remains unclear.
FFCD may be easily diagnosed using imaging
techniques. The typical radiographic signs include a well-defined,
lucent defect in the metaphyseal cortex of the medial long bone and
sclerosis along the lateral border of the lesion (10). MRI may be performed in cases where
the diagnosis is uncertain. Furthermore, MRI excludes the
possibility of soft tissue lesions. The typical appearance of FFCD
on T1- and T2-weighted MRI slices consists of a low-signal area
(corresponding to the radiolucent area) and an intermediate signal
(corresponding to the sclerotic area) (11). In the present case, the chest CT and
X-ray images showed a well-defined, unilateral, lucent and inflated
lesion in the left first transverse process and the costal head.
The cortex was thinning, but intact and there were no signs of
periosteal reaction or cortical destruction. In the present case,
the radiographic and MRI findings corresponded with the typical
features of FFCD. However, a specific diagnosis was not determined,
as FFCD had not been reported in the vertebrae or ribs in previous
studies.
FFCD is a variant of fibrous dysplasia (FD).
Radiologically, FFCD is similar to conventional FD, in that the
lesion is well demarcated and exhibits cortical expansion, but with
an intact cortex. In order to diagnose FFCD it must be
differentiated from dyschondrosteosis, Ollier’s disease,
neurofibromatosis and trauma (12).
In contrast to FFCD, FD lesions are purely fibrous and show no
evidence of cartilaginous or osseous elements (4). In the present case, the most important
differential diagnosis was osteofibrous dysplasia, as typical
osteofibrous dysplasia exhibits a similar image morphology to FFCD,
with frosted glass-like lesions, inflated and thickened lesions in
the bone, cortical plate thinning and no periosteal reaction or
cortical destruction. However, osteofibrous dysplasia always
present as a palpable mass with bone deformities. Furthermore, a
number of cases present with pathologic fractures and high alkali
phosphatase levels (13).
Additional differential diagnoses include osteoblastic sarcoma and
aneurysmal bone cysts.
It has been hypothesized that each of the
deformities associated with FFCD may spontaneously correct or
progressively improve and studies have reported an incidence of
spontaneous correction ≤45% (5).
Through observing the healing process of FFCD, Jouve et al
(8) demonstrated that an infantile
active growth plate of the proximal tibia is able to correct a
varus deformity of ≤30°. Peroneal nerve palsy (12,14)
and overcorrection to valgus deformity were reported to be a
consequence of certain cases that were treated with an osteotomy
(15). Surgical treatment may be
avoided if there is no evidence of the deformity increasing or
pathological fracture at presentation; however, in the present
case, the lesion was potentially an aneurysmal bone cyst and,
although the tumor was small, the patient requested that it was
removed, thus, it was excised.
In lesions in any of the four limbs, FFCD is
consistently associated with angular deformities in children. The
associated deformities commonly result in limb-length inequalities,
with disparities of ≤30 mm (1,4,9).
Furthermore, a limb-length discrepancy of 7.7 cm has previously
been reported in the upper limbs (6). The present study reported a case of
FFCD of the vertebra and rib. Surgery was performed to treat the
patient and a long-term follow-up was recommended in order to
assess the likelihood of FFCD recurrence.
In conclusion, the present case proposes that FFCD
may affect tubular bones as well as flat bones. However, the
underlying mechanism and treatment of FFCD requires further
investigation.
Acknowledgements
The authors would like to thank the patient for
participating in the present study.
References
|
1
|
Bell SN, Campbell PE, Cole WG and Menelaus
MB: Tibia vara caused by focal fibrocartilaginous dysplasia. Three
case reports. J Bone Joint Surg Br. 67:780–784. 1985.
|
|
2
|
Ohno I, Shimizu N, Nakase T and Yoshikawa
H: Adult case of tibia vara associated with focal
fibrocartilaginous dysplasia. J Orthop Sci. 10:328–330. 2005.
|
|
3
|
Hermann G, Klein M, Abdelwahab IF and
Kenan S: Fibrocartilaginous dysplasia. Skeletal Radiol. 25:509–511.
1996.
|
|
4
|
Beaty JH and Barrett IR: Unilateral
angular deformity of the distal end of the femur secondary to a
focal fibrous tether. A report of four cases. J Bone Joint Surg Am.
71:440–445. 1989.
|
|
5
|
Choi IH, Kim CJ, Cho TJ, et al: Focal
fibrocartilaginous dysplasia of long bones: report of eight
additional cases and literature review. J Pediatr Orthop.
20:421–427. 2000.
|
|
6
|
Lincoln TL and Birch JG: Focal
fibrocartilaginous dysplasia in the upper extremity. J Pediatr
Orthop. 17:528–532. 1997.
|
|
7
|
Kariya Y, Taniguchi K, Yagisawa H and Ooi
Y: Focal fibrocartilaginous dysplasia: consideration of healing
process. J Pediatr Orthop. 11:545–547. 1991.
|
|
8
|
Jouve JL, Kohler R, Mubarak SJ, et al:
Focal fibrocartilaginous dysplasia (‘fibrous periosteal
inclusion’): an additional series of eleven cases and literature
review. J Pediatr Orthop. 27:75–84. 2007.
|
|
9
|
Langenskiöld A: Tibia vara. A critical
review. Clin Orthop Relat Res. 195–207. 1989.
|
|
10
|
Herman TE, Siegel MJ and McAlister WH:
Focal fibrocartilaginous dysplasia associated with tibia vara.
Radiology. 177:767–768. 1990.
|
|
11
|
Meyer JS, Davidson RS, Hubbard AM and
Conard KA: MRI of focal fibrocartilaginous dysplasia. J Pediatr
Orthop. 15:304–306. 1995.
|
|
12
|
Albiñana J, Cuervo M, Certucha JA,
Gonzalez-Mediero I and Abril JC: Five additional cases of local
fibrocartilaginous dysplasia. J Pediatr Orthop B. 6:52–55.
1997.
|
|
13
|
Taylor RM, Kashima TG, Ferguson DJ, et al:
Analysis of stromal cells in osteofibrous dysplasia and
adamantinoma of long bones. Mod Pathol. 25:56–64. 2012.
|
|
14
|
Bradish CF, Davies SJ and Malone M: Tibia
vara due to focal fibrocartilaginous dysplasia. The natural
history. J Bone Joint Surg Br. 70:106–108. 1988.
|
|
15
|
Olney BW, Cole WG and Menelaus MB: Three
additional cases of focal fibrocartilaginous dysplasia causing
tibia vara. J Pediatr Orthop. 10:405–407. 1990.
|