Introduction
The most common type of intraocular tumor in adults
is the metastatic variety, with the choroid as the typical site of
involvement (1–3). In a survey of patients who presented
with an identifiable primary malignancy (3), lung cancer was the most common and
breast cancer was the next most common type, as observed in other
studies (4–10). In the present report, a case of
non-small cell lung cancer presenting with choroidal metastasis is
described. Furthermore, the apparently normal chest X-ray images
that were obtained highlight a limitation of using X-ray, as a
computed tomography (CT) scan subsequently detected the presence of
a large primary lung lesion. To the best of our knowledge, there
are few cases of choroidal metastasis presenting with non-small
lung cancer reported in the existing literature (9).
Case report
A 71-year-old Malay female was referred to the
Department of Ophthalmology, Tan Tock Seng Hospital (Singapore) in
October 2011 complaining of blurred vision in the superior field of
the right eye, which had persisted for the previous five days. The
patient did not exhibit any associated symptoms, such as eye
redness, pain or floaters and the patient was not myopic. The
patient was admitted to the internal medical unit with suspected
pneumonia and was also a carrier of the human immunodeficiency
virus for which she was undergoing Highly Active Anti Retroviral
Therapy (HAART). The patient had no other medical history. Written
informed consent was obtained from the family of the patient.
Examination revealed best-corrected visual acuity of
6/9 bilaterally. Slit-lamp examination of the anterior segment was
unremarkable, however, mild cataracts were apparent. Examination of
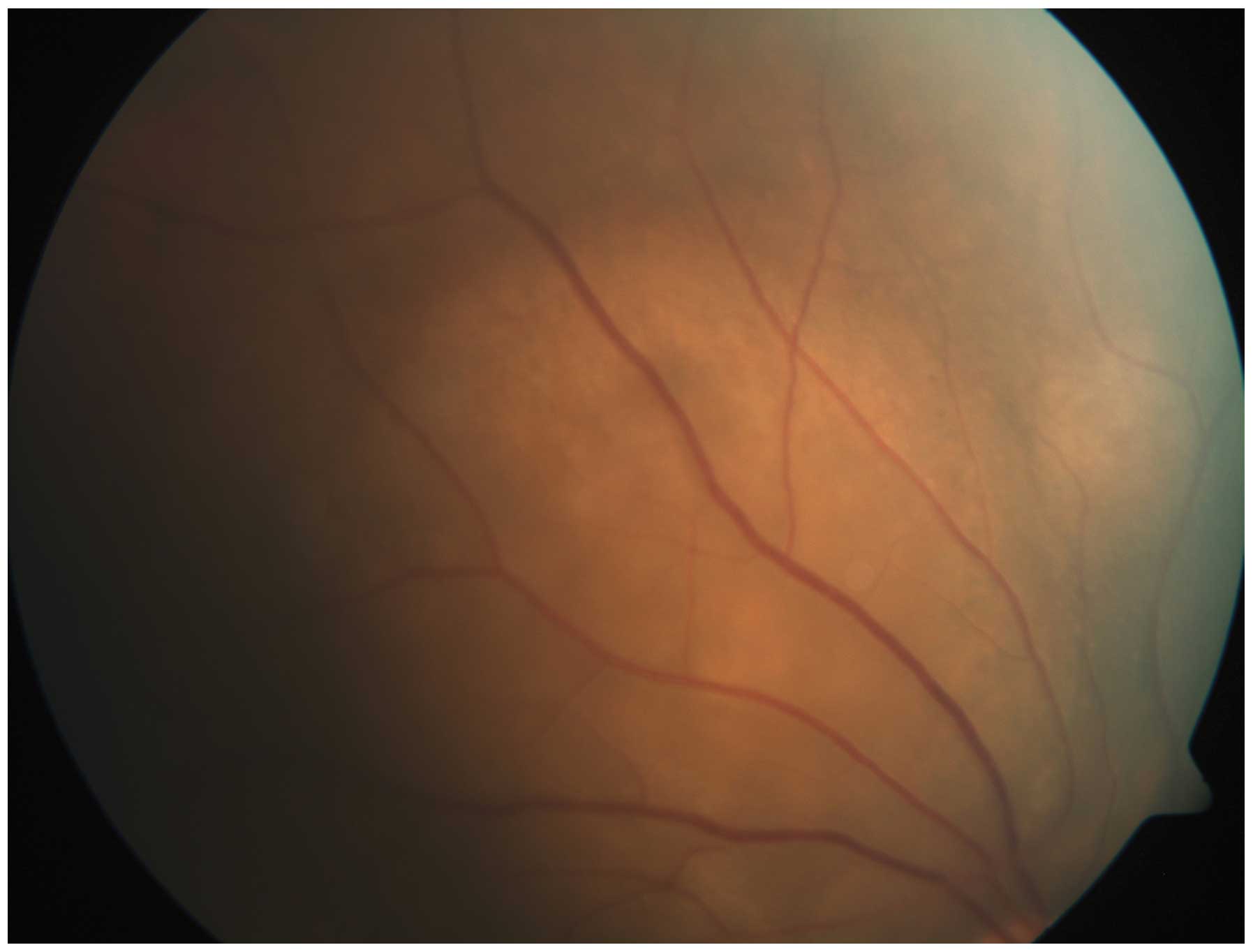
the posterior segment showed a choroidal lesion spanning ~8 mm and
involving the superior half of the macula and the superior temporal
quadrant of the right eye, with an overlying area of exudative
retinal detachment (Fig. 1). In
addition, there was a small choroidal lesion inferior to the
lesion. The posterior segment of the left eye was normal. The two
optic discs were considered to be normal and had a cup-to-disc
ratio of 0.4. The pupillary light reflex was normal, with no
relative afferent defects observed and the extraocular movements
were normal.
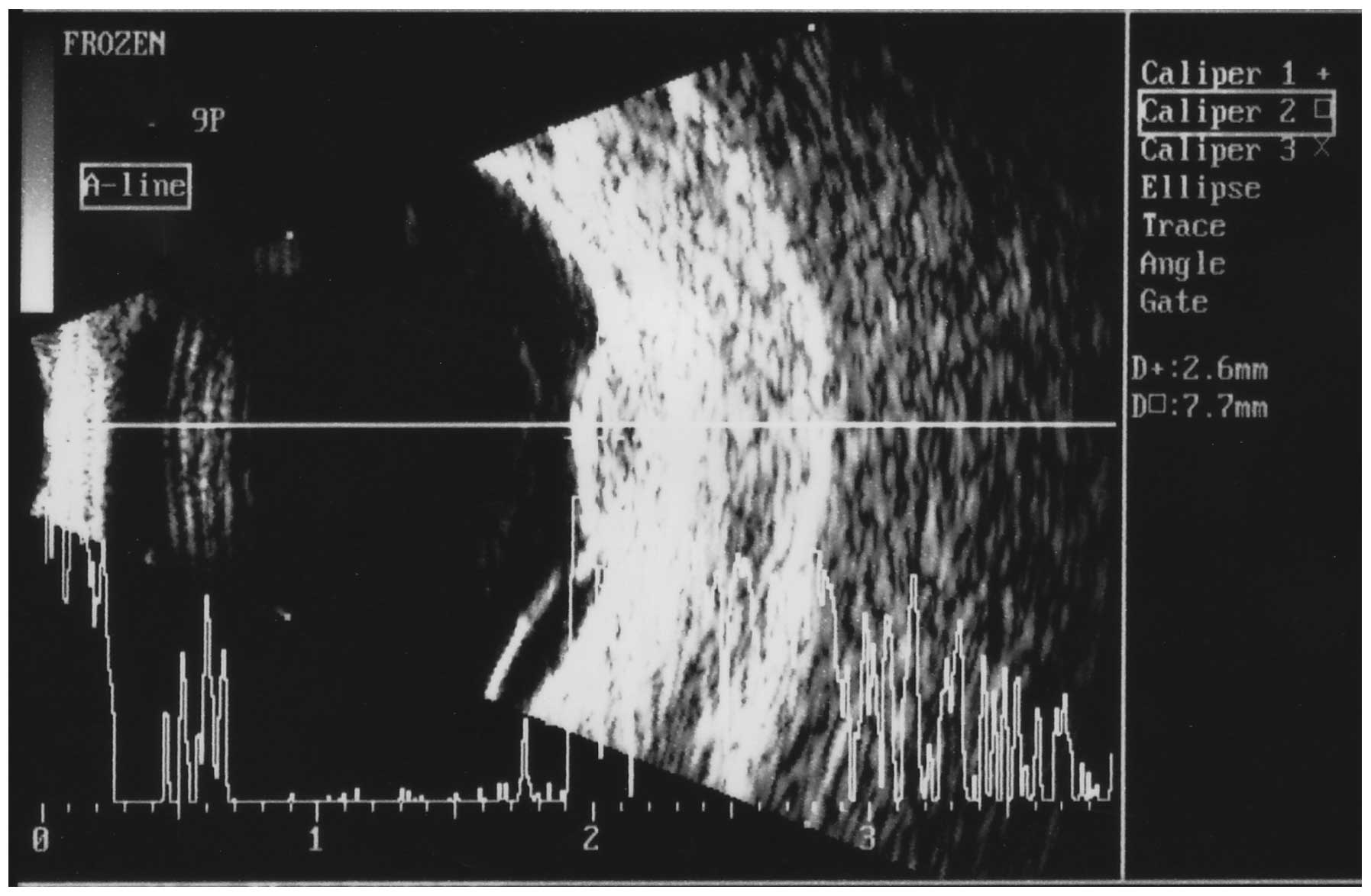
A B-scan ultrasound of the right eye showed the
superior temporal lesion measuring 7.7 mm laterally, 9.5 mm
radially and a maximum thickness of 2.6 mm, in addition, internal
reflectivity was medium to high (Fig.
2). There was an overlying area of exudative retinal
detachment. The second choroidal lesion at the inferior equator was
small with a maximal thickness of 1.5 mm and medium to high
internal reflectivity. Fluorescein angiography demonstrated early
blocked hypofluorescence with progressive hyperfluorescence at the
border of the lesion in the later phases and pinpointed leakages.
Indocyanine green angiography showed blocked hypofluorescence with
hyperfluorescence at the border of the lesion.
A full blood count indicated normocytic normochromic
anemia, however, was otherwise normal. The C-reactive protein level
was markedly elevated and the levels of liver transaminases were
mildly raised. Serology for syphilis was identified as negative,
however, immunoglobulin G serology for the cytomegalovirus and
toxoplasmosis were positive. Serum electrolyte levels and the
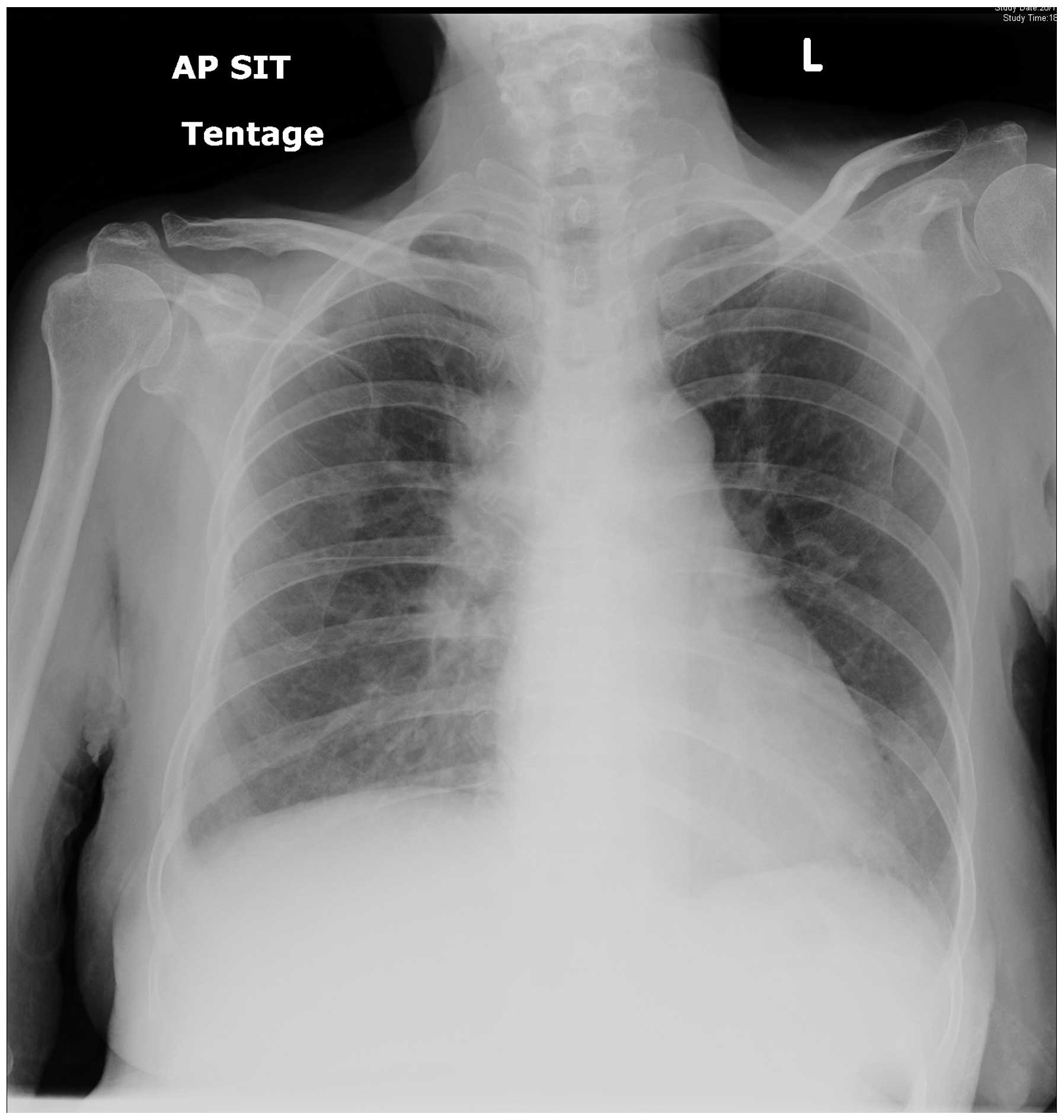
patient’s coagulation profile were normal. Notably, a chest X-ray
showed increased air space shadowing in the left lower lobe, which
was consistent with pneumonia; the right lung lobes were normal
(Fig. 3). It was hypothesized,
based on the clinical findings, that the patient was presenting
with ocular tuberculosis or choroidal metastasis, therefore, a CT
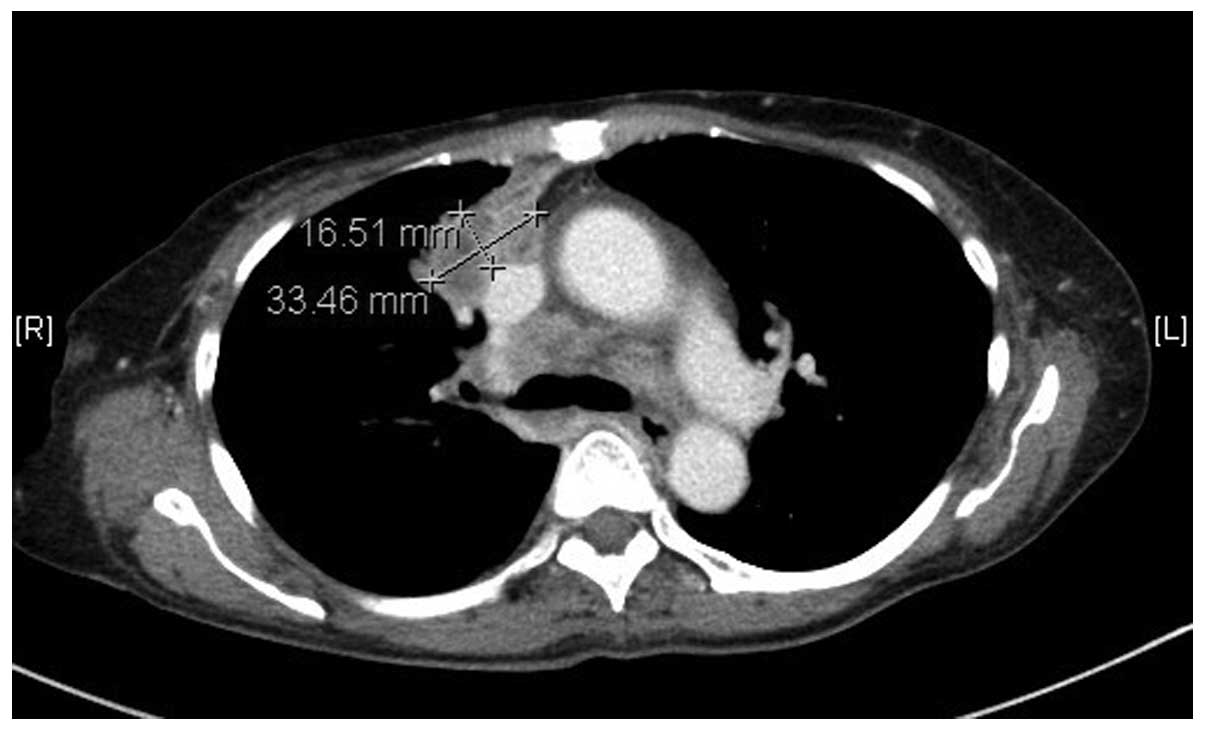
scan of the whole body was performed. The CT scan of the thorax
revealed a large lobulated mass in the right upper lobe, measuring
3.3×1.6 cm (Fig. 4). Metastases
were indicated by multiple, subcentimeter lesions in the other
regions of each lung, as well as by multiple hypodense lesions in
the liver and multiple lytic lesions in the thoracolumbar spine.
Multiple enlarged bilateral supraclavicular, pretracheal,
subcarinal and right hilar lymph nodes were also observed. Thus,
the patient was advised to undergo a confirmatory lung biopsy,
which revealed a non-small cell lung carcinoma that was indicative
of an adenocarcinoma. Immunohistochemistry demonstrated that there
were more thyroid transcription factor 1-positive cells than
p63-positive cells in addition to faint diffuse staining for the
two markers. Immunohistochemistry, therefore, indicated an
adenocarcinoma. Although the preservation of the DNA in this case
was not sufficient to allow a confident analysis of exon 18, the
other three axons of clinical significance were wild-type.
Mutations in exons 19 and 21 represented >90% of the total
mutations. Furthermore, the KRAS mutation was identified in
codon 13 of exon 2 and there was no rearrangement of the ALK
gene. However, pleural fluid cytology did not reveal any malignant
cells. Based on the clinical findings, it was hypothesized that the
choroidal lesions in the right eye were potentially metastatic. A
repeat chest X-ray was conducted two weeks following the initial
presentation, which showed interval enlargement of the right-sided
pleural effusion and further compressive collapse of the right
lung. Bony destruction in the lateral aspects of the right, fifth
to seventh ribs and erosion of T11 was noted, which indicated a
neoplastic process was occurring. The patient’s family was
counseled regarding the terminal nature of the illness and the
prognosis of 6–12 months was reiterated to them. Palliative
management was advised based on discussion with the family and the
patient continued receiving HAART therapy for the retroviral
disease. However, the patient succumbed to the cancer within the
following two weeks.
Discussion
Metastatic tumors are the most common type of
intraocular malignancy, with the choroid being the typical site of
involvement (1–3). The symptoms include blurred vision in
80% of patients, pain in 14%, photopsia in 13%, red eye and
floaters in 7% and field defects in 3% (1–4).
Metastatic tumors have a creamy yellow appearance and additional
clinical features that indicate metastasis are multifocality and
bilateralism (4).
The differential diagnosis of choroidal metastasis
include choroidal melanoma, choroidal osteoma, choroidal
hemangioma, choroidal neovascularization with disciform scarring,
tuberculoma and posterior scleritis (2–4).
Common primary sites include the lungs,
gastrointestinal tract, pancreas, kidney, the skin, the breasts (in
females) and the prostate (in males) (2–4). In a
previous study, at the time of ocular diagnosis, 66% of patients
reported no history of previous cancer and of the remaining 34%,
49% exhibited a subsequently identifiable primary site (3). In another study, of all of the
patients presenting with choroidal metastasis, 58% had lung cancer
and 28% had breast cancer (4).
However, it was estimated in a study by Kreusel et al
(5) that in patients with
metastatic lung carcinoma, just 7.1% presented with ocular
involvement. In the present study, the patient presented with a
visual field defect and a fundus examination demonstrated the
presence of a large choroidal mass lesion.
B-scan ultrasounds of metastatic lesions regularly
show echogenic subretinal masses with diffuse, ill-defined borders
and moderate internal reflectivity. Furthermore, overlying retinal
detachment is common (4,5). The fluorescein angiographic
characteristics of choroidal metastases show early hypofluorescence
in the arterial phase, progressive hyperfluorescence in subsequent
phases and retinal capillary dilatation at the border of the lesion
with persistent pinpoint leakages (4,5). This
was consistent with the the observations of the patient in the
present study.
The characteristic notable observation in the
current case report was an apparently normal chest X-ray in the
presence of a significantly large tumor in the right upper lobe.
X-ray is routinely conducted by the majority of ophthalmologists to
rule out associated pulmonary tuberculosis in patients exhibiting a
granulomatous uveitis or choroidal granuloma, however, the use of a
normal X-ray (as was used in the current case) may be misleading.
Based on this observation, it is proposed that ophthalmologists
perform a CT scan to rule out a primary lung lesion rather than
advising the performance of a chest X-ray, which may present
erroneous findings.
Treatment for ocular metastases is considered to be
palliative as the presence of such metastases indicates a
hematogenous spread of cancer. Therefore, the aim of any treatment
strategy is to maximize the patient’s quality of life and restore
or preserve their vision, which may be achieved via radiotherapy or
chemotherapy. Surgery is not significant other than for conducting
diagnostic biopsies, as often there is no need for tumor debulking
and surgery is associated with an increased risk of morbidity.
A review of the literature revealed 12 cases where
lung cancer patients were suffering from choroidal metastases as
the primary clinical symptom (5–10). In
all of these cases, the diagnosis of choroidal metastases indicated
the end-stage disease and the cancer dissemination appears to be
inevitable; thus, the prognosis is poor and life expectancy is
short (5–10). In the present case, on determining
the diagnosis and planning the treatment strategy, the patient
succumbed due to metastasis. Therefore, the presence of choroidal
metastasis in patients with lung carcinoma appears to indicate
end-stage disease and is associated with a particularly short life
expectancy.
In conclusion, the diagnosis of ocular metastases is
based primarily on clinical findings, which may be supplemented by
imaging studies and determined via histopathology. Choroidal
metastasis should be anticipated when a large choroidal lesion and
overlying exudative retinal detachment are observed. An X-ray may
appear to be normal even in the presence of a large pulmonary
lesion; therefore, in cases of potential metastasis, a CT scan
should be performed. The presence of choroidal lesions with the
primary lesion in the lungs is indicative of end-stage disease and,
therefore, is associated with a limited life expectancy.
References
|
1
|
Ferry AP and Font RL: Carcinoma metastatic
to eye and orbit. I A clinicopathologic study of 227 cases. Arch
Ophthalmol. 92:276–286. 1974.
|
|
2
|
Stephens RF and Shields JA: Diagnosis and
management of cancer metastatic to the uvea: a study of 70 cases.
Ophthalmology. 86:1336–1349. 1979.
|
|
3
|
Shields CL, Shields JA, Gross NE, et al:
Survey of 520 eyes with uveal metastases. Ophthalmology.
104:1265–1276. 1997.
|
|
4
|
Kreusel KM, Bechrakis N, Wiegel T, et al:
Clinical characteristics of choroidal metastasis. Ophthalmologe.
100:618–622. 2003.(In German).
|
|
5
|
Kreusel KM, Wiegel T, Stange M, et al:
Choroidal metastasis in disseminated lung cancer: frequency and
risk factors. Am J Ophthalmol. 134:445–447. 2002.
|
|
6
|
Kreusel KM, Bornfeld N, Hosten N, Wiegel T
and Foerster MH: Solitary choroidal metastasis as the first sign of
metastatic lung carcinoid. Arch Ophthalmol. 116:1396–1397.
1998.
|
|
7
|
Simsek T, Ozdamar Y and Berker N:
Choroidal mass as an initial presentation of lung cancer. Med
Oncol. 25:400–402. 2008.
|
|
8
|
Fernandes BF, Fernandes LH and Burnier MN
Jr: Choroidal mass as the presenting sign of small cell lung
carcinoma. Can J Ophthalmol. 41:605–608. 2006.
|
|
9
|
Ascaso FJ, Castillo JM, García FJ,
Cristóbal JA, Fuertes A and Artal A: Bilateral choroidal metastases
revealing an advanced non-small cell lung cancer. Ann Thorac Surg.
88:1013–1015. 2009.
|
|
10
|
Koçak Z, Tabakoğlu E, Benian O, Bayir G,
Unlü E and Uzal C: Bilateral choroidal metastases as an initial
manifestation of small-cell carcinoma of the lung. Tuberk Toraks.
54:61–64. 2006.
|