Introduction
Lung cancer is one of the most commonly observed
malignancies in clinical diagnosis. In total, ~85% of lung cancer
cases are diagnosed as non-small cell lung cancer (NSCLC). Due to
environmental deterioration and changes in lifestyle, the incidence
rate of NSCLC has significantly increased, becoming one of the
predominant diseases to threaten human health (1,2).
Radical surgery is commonly used to treat NSCLC; however, relapse
frequently occurs following surgery, which reduces the
postoperative survival time of patients (3). Causes of relapse in NSCLC may include
the incomplete resection of the tumor and the inhibition of the
human immune system, which may enable tumor cells to avoid immune
killing (4). CD4+ T
lymphocytes can be divided into T helper 1 (Th1) and Th2 cell
subgroups, according to the secreted cytokine types. The Th1
subgroup releases interleukin 2 (IL-2) and interferon-γ (INF-γ),
which has antitumor effects in the human body. The Th2 subgroup
predominantly releases IL-4 and IL-10, which are involved in the
inhibition of the immune system, preventing the human body from
killing tumor cells (5,6).
In several studies, the Th1/Th2 immunological
balance in tumor patients has been shown to be significant in
tumorigenesis, development and relapse (7,8). A
number of studies have also revealed that in breast, gastric and
lung cancer patients, the immunological balance of Th1 and Th2 in
the peripheral blood is altered, with the human body maintaining a
Th2-dominant shift. The immunodominance of Th2 prevents the patient
from effectively killing the tumor cells that have survived
incomplete resection, which eventually results in relapse (9–11).
Studies have indicated that when Th2 cytokines are dominant in the
peripheral blood of NSCLC patients, the patient’s immunity is in a
state of immune tolerance (12,13).
However, few studies have investigated the changes in the levels of
Th1 and Th2 cytokines in the peripheral blood following surgery, as
well as the correlation between such changes and relapse or
survival. Therefore, the current study began by analyzing the
changes in the levels of Th1 and Th2 cytokines in NSCLC patients
prior to and following surgery. In addition, the correlation
between cytokine levels and patient relapse and survival was
explored. The aim of this study was to investigate the serum
Th1/Th2 cytokine shift and its clinical significance in the tumor
tissues of patients with NSCLC.
Patients and methods
Patient presentation
A total of 124 patients with NSCLC, who were
admitted to Xinxiang Central Hospital (Xinxiang, China) between
June 2010 and June 2013, were selected for this study. All patients
underwent radical surgery treatment and were diagnosed
pathologically with NSCLC. All patients did not receive
chemotherapy, radiotherapy or immune enhancer treatment prior to or
following surgery. The hepatorenal functions of patients were
normal and patients had no general infectious diseases. Of the 124
patients, 82 were male and 42 were female, with an average age of
60.25±10.01 years (range, 40–75 years). In terms of pathological
types, there were 43 cases of squamous cell carcinoma, 60 cases of
adenocarcinoma and 21 cases of mixed type. For TNM staging
(3), there were 50 cases of stage
IIa and 74 cases of stage IIb. Concomitantly, 124 healthy people
undergoing physical examination at the same hospital during this
period were selected as controls, including 90 males and 34
females, with an average age of 58.65±11.42 years (range, 41–69
years). The comparison between the control and observation groups
with respect to gender and age range did not show statistical
significance, exhibiting a certain comparability (P>0.05). This
study was conducted in accordance with the declaration of Helsinki
and with approval from the ethics committee of Xinxiang Central
Hospital (Xinxiang, China). Written informed consent was obtained
from all participants.
Detection of cytokines
In the observation group, 5 ml of venous blood was
obtained 10 days prior to and 10 days following surgery, and was
not processed with anticoagulation. Following the stratification of
blood by 30 min of quiescence at 4°C, the blood was centrifuged at
5,000 × g for 5 min and the serum was extracted. Serum of the
control group was collected using the same approach. Samples were
frozen at −80°C for further use. An ELISA kit (R&D Systems
Inc., Minneapolis, MN, USA) was used to measure IL-2, IL-4, IL-10
and INF-γ levels in the serum. During the assay, standard curves
were established for all four cytokines, and the corresponding
cytokine concentration was calculated according to the standard
curve. The assays were conducted according to the manufacturer’s
instructions. All experiments for each sample were performed in
triplicate. The normal ranges for the four cytokines were as
follows: IL-2, 1.5–3.6 mg/ml; IL-4, 1.8–2.9 mg/ml; IL-10, 2.5-6-4.6
mg/ml; and IFN-γ, 7.3–16.5 mg/ml. Cytokine levels outside of these
ranges were considered to be abnormal.
Statistical analysis
All data were analyzed using SPSS 17.0 (SPSS, Inc.,
Chicago, IL, USA), and the data are presented as the mean ±
standard deviation. Comparisons of measurement data were assessed
by Student’s t-test, and comparisons of count data were assessed
using Pearson’s χ2 test. Comparisons between cumulative
relapse frequencies and the cumulative survival rate were assessed
by Kaplan-Meier and log-rank tests. P<0.05 was considered to
indicate a statistically significant difference.
Results
Comparison between the Th1/Th2 cytokine
levels of two groups prior to and following surgery
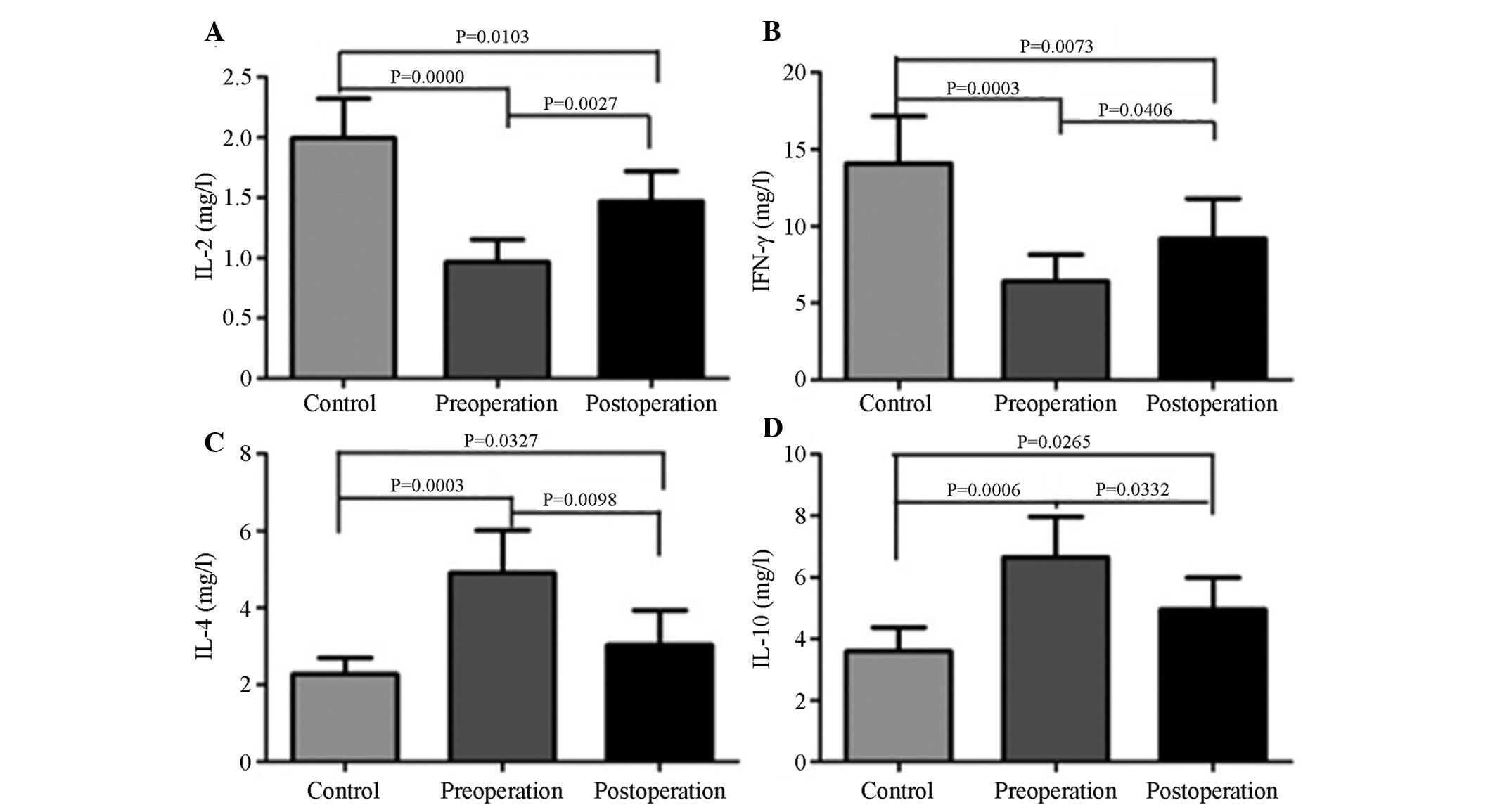
Compared with IL-4 (2.28±0.27 mg/ml) and IL-10
(3.60±0.32 mg/ml) levels in the control group, the IL-4 (4.90±0.46
mg/ml) and IL-10 (6.65±0.54 mg/ml) concentrations in the peripheral
blood of the observation group prior to surgery were significantly
higher (P<0.05) (Fig. 1).
Following surgery, the IL-4 (3.03±0.37 mg/ml) and IL-10 (4.96±0.42
mg/ml) concentrations in the peripheral blood of the observation
group had decreased significantly compared with the levels prior to
surgery (P<0.05), but remained significantly higher than those
in the control group (P<0.05).
Compared with the IL-2 (2.00±0.13 mg/ml) and INF-γ
(14.07±1.25 mg/ml) levels in the control group, the IL-2 (0.97±0.08
mg/ml) and INF-γ (6.40±0.71 mg/ml) levels in the peripheral blood
of the observation group prior to surgery were significantly lower
(P<0.05). Additionally, following surgery, the IL-2 (1.47±0.10
mg/ml) and INF-γ (9.21±0.91 mg/ml) levels in the peripheral blood
of the observation group had increased significantly compared with
the levels prior to surgery (P<0.05), but remained significantly
lower than those in the control group (P<0.05).
Correlation between various cytokines and
patient relapse
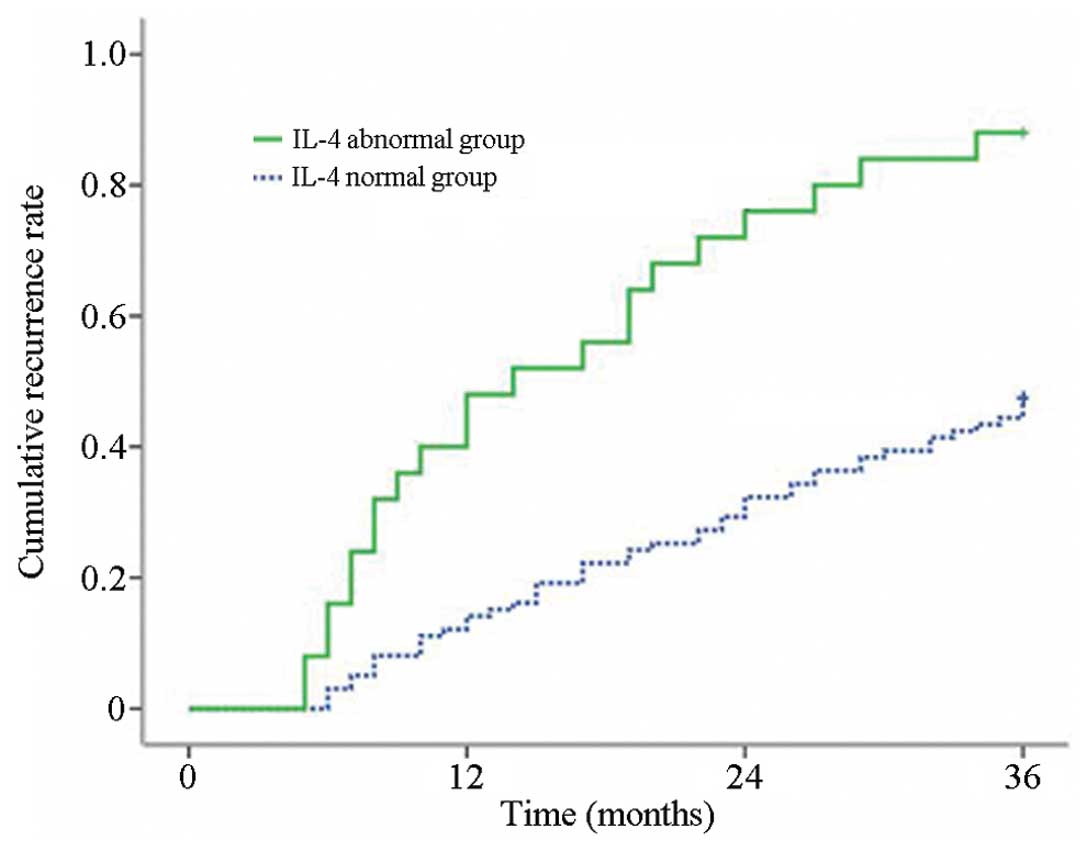
As shown in Table I
and Fig. 2, the one- and three-year
cumulative relapse rates of patients with postoperative IL-4
abnormalities were higher than those of patients without
postoperative IL-4 abnormalities, and the difference showed
statistical significance (P<0.05). Furthermore, the one-and
three-year cumulative relapse rates of patients with postoperative
IL-2, IL-10 and INF-γ abnormalities were not significantly
different compared with those of patients without such
abnormalities (P>0.05).
 | Table IComparison between the postoperative
cumulative relapse rates of patients with varying cytokine
levels. |
Table I
Comparison between the postoperative
cumulative relapse rates of patients with varying cytokine
levels.
| | Cumulative relapse
rate, % | | |
|---|
| |
| | |
|---|
| Cytokine | Cases, n | 1-year | 3-year | Log-rank | P-valuea |
|---|
| IL-2 |
| Normal | 91 | 19.78 | 42.96 | 2.456 | 0.147 |
| Abnormal | 33 | 24.24 | 42.42 | | |
| INF-γ |
| Normal | 82 | 17.07 | 50.00 | 0.063 | 0.802 |
| Abnormal | 42 | 21.43 | 52.38 | | |
| IL-4 |
| Normal | 99 | 15.15 | 33.33 | 5.119 | 0.001a |
| Abnormal | 25 | 40.00 | 72.00 | | |
| IL-10 |
| Normal | 102 | 25.49 | 54.90 | 1.157 | 0.307 |
| Abnormal | 22 | 31.82 | 50.00 | | |
Correlation between various cytokines and
patient postoperative survival
As shown in Table
II, the median survival time and the cumulative survival rate
of patients with postoperative IL-2, INF-γ and IL-10 level
abnormalities were not significantly different compared with those
of patients without these abnormalities (P>0.05). However, the
median survival time and cumulative survival rate of patients with
abnormal postoperative IL-4 levels were significantly lower
compared with those of patients with normal postoperative IL-4
levels (P<0.05).
 | Table IICorrelation between the various
cytokine levels and postoperative survival time in patients with
non-small cell lung cancer. |
Table II
Correlation between the various
cytokine levels and postoperative survival time in patients with
non-small cell lung cancer.
| Cytokine | Cases, n | Median survival time
(range), months | Cumulative survival
rate, % | Log-rank | P-valuea |
|---|
|
|---|
| 1-yea | r 3-year |
|---|
| IL-2 |
| Normal | 91 | 26 (13.34–31.35) | 84.84 | 48.48 | 0.078 | 0.801 |
| Abnormal | 33 | 22 (9.56–35.21) | 76.92 | 52.75 | | |
| INF-γ |
| Normal | 82 | 28 (16.49–36.14) | 85.37 | 64.63 | 1.386 | 0.219 |
| Abnormal | 42 | 24 (12.56–30.87) | 73.81 | 57.14 | | |
| IL-4 |
| Normal | 99 | 26 (18.55–34.49) | 90.90 | 78.79 | 4.487 | 0.021a |
| Abnormal | 25 | 18 (7.51–25.39) | 76.00 | 44.00 | | |
| IL-10 |
| Normal | 102 | 28 (18.19–32.33) | 73.53 | 46.08 | 1.987 | 0.115 |
| Abnormal | 22 | 26 (15.12–35.89) | 68.18 | 40.91 | | |
Discussion
NSCLC is one of the most commonly observed lung
cancers in clinical practice, with morbidity and mortality
exhibiting a significant increasing trend, and with a poor
postoperative prognosis. NSCLC has become one of the predominant
causes of cancer-related mortalities in a number of countries
(14). In recent years, with the
progression of tumor immunology studies, Th1 cytokines have been
found to dominate the peripheral blood of numerous tumor patients
(15). However, certain studies
have also identified a Th2 cytokine shift in tumor cells. This
phenomenon has been closely associated with clinical stages and
postoperative effects in patients (15).
The present study analyzed the levels of Th1 and Th2
cytokine expression in the peripheral blood of NSCLC patients. The
results demonstrated that, compared with the healthy controls, the
levels of Th1 cytokines, IL-2 and INF-γ, in the peripheral blood of
NSCLC patients significantly decreased. However, the levels of Th2
cytokines, IL-4 and IL-10, significantly increased, indicating that
the NSCLC patients exhibited an evident Th2 cytokine shift. This
finding is consistent with the majority of existing studies
(13,16). Notably, following the resection of
NSCLC, the Th1 cytokines, IL-2 and INF-γ, in the peripheral blood
increased significantly compared with the levels prior to surgery,
while levels of the Th2 cytokines, IL-4 and IL-10, decreased. The
Th1/Th2 cytokine shift was improved to a certain degree, but did
not reach the normal level, indicating that the resection of the
tumor may help to combat patient immunosuppression.
For NSCLC patients, the relapse rate is relatively
high and the survival time is shorter than that for other cancer
types (17,18). The main causes of this phenomenon
not only include incomplete resection, but also closely correlate
with the inhibition of the patient’s immune system (17). The present study demonstrated that
although surgery may improve immunosuppression in patients, the
effects were limited. For certain patients, the Th1 and Th2
cytokine levels remained abnormal following the resection. However,
if the Th1 and Th2 cytokine levels are normal, even if residual
tumor cells exist, the immune system may kill these remaining tumor
cells and suppress the relapse of the disease. By contrast, whilst
in a state of immunosuppression, the body cannot kill the tumor
cells effectively and, thus, tumor relapse occurs.
The current study initially analyzed the correlation
between Th1 and Th2 cytokine abnormalities and patient relapse.
Patients with postoperative IL-4 abnormalities were found to
exhibit a significantly shorter survival time, indicating that IL-4
levels are significant in the postoperative survival of NSCLC
patients. However, the postoperative IL-2, IL-10 and INF-γ levels
did not exhibit a marked impact on relapse. This finding has also
been verified among breast cancer patients (19). The present analysis of patient
survival time demonstrated that NSCLC patients with postoperative
IL-4 level abnormalities exhibit a decreased median survival time
and survival rate. This finding corresponded with the relapse rate
of patients with postoperative IL-4 level abnormalities. The
reasoning behind the abnormally high postoperative expression
levels of IL-4 leading to reduced relapse and survival rates may be
that IL-4 induces the differentiation of Th1 into Th2 and
therefore, the lymphocyte activation was inhibited. IL-4 may also
upregulate the antiapoptotic protein level, thereby reducing the
killing ability towards tumor cells (20–22).
Notably, in the current study, no statistically
significant difference was identified between the patient relapse
and survival rates in patients with postoperative IL-2, IL-10 and
INF-γ abnormalities. However, this may be attributed to the limited
sample size. In addition, the present study adopted a one-way
analysis of variance, but the tumor relapse and survival rates were
influenced by multiple factors. Therefore, the correlation between
these cytokines, tumor relapse and the survival rate should be
analyzed based on multiple factors.
Furthermore, Th2 cytokines evidently dominated the
peripheral blood of NSCLC patients, and surgery greatly improved
this Th2 cytokine shift. The abnormal expression of IL-4 levels in
the peripheral blood following surgery was also found to inversely
correlate with patient relapse and survival rates. In conclusion,
this study provides guidance regarding postoperative immune
intervention in NSCLC patients.
References
|
1
|
Boukovinas I, Tsakiridis K, Zarogoulidis
P, Machairiotis N, Katsikogiannis N, Kougioumtzi I and Zarogoulidis
K: Neo-adjuvant chemotherapy in early stage non-small cell lung
cancer. J Thorac Dis. 5(Suppl 4): S446–S448. 2013.
|
|
2
|
Zarogoulidis K, Zarogoulidis P, Darwiche
K, et al: Treatment of non-small cell lung cancer (NSCLC). J Thorac
Dis. 5(Suppl 4): S389–S396. 2013.
|
|
3
|
Baltayiannis N, Chandrinos M,
Anagnostopoulos D, et al: Lung cancer surgery: an up to date. J
Thorac Dis. 5(Suppl 4): S425–S439. 2013.
|
|
4
|
Yuanying Y, Lizhi N, Feng M, et al:
Therapeutic outcomes of combining cryotherapy, chemotherapy and
DC-CIK immunotherapy in the treatment of metastatic non-small cell
lung cancer. Cryobiology. 67:235–240. 2013.
|
|
5
|
Becker Y: Respiratory syncytial virus
(RSV) evades the human adaptive immune system by skewing the
Th1/Th2 cytokine balance toward increased levels of Th2 cytokines
and IgE, markers of allergy - a review. Virus Genes. 33:235–252.
2006.
|
|
6
|
Pinto RA, Arredondo SM, Bono MR, Gaggero
AA and Díaz PV: T helper 1/T helper 2 cytokine imbalance in
respiratory syncytial virus infection is associated with increased
endogenous plasma cortisol. Pediatrics. 117:e878–e886. 2006.
|
|
7
|
Krohn M, Listing M, Tjahjono G, Reisshauer
A, Peters E, Klapp BF and Rauchfuss M: Depression, mood, stress,
and Th1/Th2 immune balance in primary breast cancer patients
undergoing classical massage therapy. Support Care Cancer.
19:1303–1311. 2011.
|
|
8
|
Green VL, Alexandropoulou A, Walker MB,
Walker AA, Sharp DM, Walker LG and Greenman J: Alterations in the
Th1/Th2 balance in breast cancer patients using reflexology and
scalp massage. Exp Ther Med. 1:97–108. 2010.
|
|
9
|
Hong CC, Yao S, McCann SE, et al:
Pretreatment levels of circulating Th1 and Th2 cytokines, and their
ratios, are associated with ER-negative and triple negative breast
cancers. Breast Cancer Res Treat. 139:477–488. 2013.
|
|
10
|
Wei H, Sun R, Xiao W, Feng J, Zhen C, Xu X
and Tian Z: Traditional Chinese medicine Astragalus reverses
predominance of Th2 cytokines and their up-stream transcript
factors in lung cancer patients. Oncol Rep. 10:1507–1512. 2003.
|
|
11
|
Liang J, Li Y, Liu X, Xu X and Zhao Y:
Relationship between cytokine levels and clinical classification of
gastric cancer. Asian Pac J Cancer Prev. 12:1803–1806. 2011.
|
|
12
|
Chen G, Wang QR and Hu SM: Relationship
between Th1/Th2 drift and T-bet/GATA3 gene expression in elderly
patients with non-small cell lung cancer. Hua Zhong Ke Ji Da Xue
Xue Bao. 5:509–512. 2011.(In Chinese).
|
|
13
|
Ito N, Suzuki Y, Taniguchi Y, Ishiguro K,
Nakamura H and Ohgi S: Prognostic significance of T helper 1 and 2
and T cytotoxic 1 and 2 cells in patients with non-small cell lung
cancer. Anticancer Res. 25:2027–2031. 2005.
|
|
14
|
Sculier JP: Non small cell lung cancer.
Eur Respir Rev. 22:33–36. 2013.
|
|
15
|
Zheng YW, Li RM, Zhang XW and Ren XB:
Current adoptive immunotherapy in non-small cell lung cancer and
potential influence of therapy outcome. Cancer Invest. 31:197–205.
2013.
|
|
16
|
Ito N, Nakamura H, Metsugi H and Ohgi S:
Dissociation between T helper type 1 and type 2 differentiation and
cytokine production in tumor-infiltrating lymphocytes in patients
with lung cancer. Surg Today. 31:390–394. 2001.
|
|
17
|
Filipits M and Pirker R: Predictive
markers in the adjuvant therapy of non-small cell lung cancer. Lung
Cancer. 74:355–363. 2011.
|
|
18
|
Jemal A, Murray T, Ward E, et al: Cancer
statistics, 2005. CA Cancer J Clin. 55:10–30. 2005.
|
|
19
|
Weng Q, Yu LL, Cai YQ and Tang J:
Relationship between peripheral blood cytokine expression and
recurrence in 58 cases with ovarian cancer. Zhong Liu Xue Za Zhi.
11:861–863. 2010.(In Chinese).
|
|
20
|
Francipane MG, Alea MP, Lombardo Y, Todaro
M, Medema JP and Stassi G: Crucial role of interleukin-4 in the
survival of colon cancer stem cells. Cancer Res. 68:4022–4025.
2008.
|
|
21
|
Conticello C, Pedini F, Zeuner A, et al:
IL-4 protects tumor cells from anti-CD95 and chemotherapeutic
agents via up-regulation of antiapoptotic proteins. J Immunol.
172:5467–5477. 2004.
|
|
22
|
Cui X, Yang SC, Sharma S, Heuze-Vourc’h N
and Dubinett SM: IL-4 regulates COX-2 and PGE2 production in human
non-small cell lung cancer. Biochem Biophys Res Commun.
343:995–1001. 2006.
|