Introduction
Synovial sarcomas (SS) are high-grade soft-tissue
sarcomas that are associated with poor survival (1). The tumor cells, however, do not derive
from synovial cells, but rather from cells of periarticular tissue
or from mesenchymal stem cells elsewhere in the body. SS have been
described at virtually every anatomical site (2). The extremities are the most common
primary sites of SS. The lower extremes account for ~70% of cases
(3). However, SS is uncommon in the
head and neck region; 3–5% of all sarcomas arising in the head and
neck are SS (4).
Due to the low clinical morbidity, concealed
anatomical site, non-specific symptoms and heterogeneous
histopathological features, SS in the ITF are often misdiagnosed.
As a result, clinical diagnosis and treatment planning remain a
challenge. To the best of our knowledge, a search of the English
literature indicated that there are eight previous studies
revealing nine cases of SS located in the ITF, including only one
case with intracranial involvement (Table I) (5–12).
There is a definitive requirement to report cases of SS in the ITF
when diagnosed, as knowledge about its clinical manifestations,
imaging, diagnosis, management strategies and outcome is lacking.
The current study presents a case of biphasic SS located in the
ITF, with intracranial involvement. The details of the clinical,
radiographical, surgical and histopathological findings are
reported. In addition, the reported English literature with regard
to SS of ITF is systematically reviewed and the clinicopathological
characteristics, treatment modality and outcome are discussed.
 | Table ICases of SS of the ITF reported in the
English literature. |
Table I
Cases of SS of the ITF reported in the
English literature.
| Cases | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|
| Age, years | 23 | 30 | 26 | 72 | 72 | 31 | 46 | 61 | 18 | 7 |
| Gender | Female | Male | Female | Female | Male | Female | Female | Female | Female | Female |
| Case history,
months | 5 | 12 | Unspecified | 6 | Unspecified | 6 | Unspecified | Unspecified | Unspecified | Unspecified |
| Symptoms | Swelling | LP | RMO | LP | Unspecified | RMO, LP | Migraines | LP | Unspecified | Unspecified |
| Radiology | CT, MRI | CT, MRI | CT | CT, MRI | MRI | MRI | CT, MRI | CT | MRI | Unspecified |
| Tumor diameter,
cm | 5.1 | 3.3 | 3.2 | 7.0 | 13.0 | 5.0 | 4.7 | Unspecified | Unspecified | Unspecified |
| TMM | Heterogeneous,
septation | Heterogeneous,
calcifications | Homogeneous | Heterogeneous,
necrosis, calcification | Homogeneous cystic
mass | Heterogeneous | Heterogeneous | Heterogeneous,
calcifications | Heterogeneous | Unspecified |
| SSTE | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Unspecified |
| Bony
infiltration | Yes | No | Yes | Yes | No | No | Yes | Yes | Yes | Unspecified |
| ICE | Yes | Yes | No | No | No | No | No | No | No | Unspecified |
| Lymphadenopathy | Negative | Negative | Negative | Negative | Unspecified | Negative | Negative | Unspecified | Unspecified | Unspecified |
| Preoperetive
biopsy | Yes (FNC) | No | Yes (FNC, IB) | Yes (FNC, IB) | Unspecified | Unspecified | Yes (FNC, IB) | Unspecified | Unspecified | Unspecified |
| DB-FNAC | No | No | Yes | No | Unspecified | Unspecified | No | Unspecified | Unspecified | Unspecified |
| Surgery type | En-bloc | En-bloc | En-bloc | En-bloc | Unspecified | En-bloc | En-bloc | Unspecified | None | Unspecified |
| IFB | Yes | Unspecified | Yes | Yes | Unspecified | Unspecified | Yes | Unspecified | None | Unspecified |
| Margin status | Negative | Negative | Negative | Negative | Unspecified | Negative | Negative | Unspecified | Unspecified | Unspecified |
| PD | Biphasic | Biphasic | Biphasic | Biphasic | Unspecified | Monophasic | Monophasic | Monophasic | Monophasic | Unspecified |
| ADT | Yes (IHC) | Yes (IHC) | Yes (IHC) | Yes (IHC) | Unspecified | Yes (IHC) | Yes (IHC) | Unspecified | Unspecified | Unspecified |
| IHC positive for | EMA, Vim CD99, CK7,
CK19, CD34 | EMA, CK | EMA, Vim, CK, Cal,
Bcl-2, S-100 | Vim, CD99 | Unspecified | EMA, Vim, CK,
CD99 | EMA, CK, Cal, Bcl-2,
S-100 | Unspecified | Unspecified | EMA, CK, CD99 |
| Treatment | S+C+R | S+C+R | S+C | S | Unspecified | S | S+C+R | S+R | C+R | Unspecified |
| PMW | Yes (PET-CT) | Yes (MRI) | Yes | Yes | Unspecified | Unspecified | Yes | Unspecified | Yes | Unspecified |
| Follow-up (m) | 24 | 12 | 42 | 14 | Unspecified | Unspecified | 12 | 96 | 180 | 192 |
| Outcome | NED | NED | NED | MPPM | Unspecified | Unspecified | NED | NED | NED | MLCM |
| Survival
status | Alive | Alive | Alive | Death | Unspecified | Unspecified | Alive | Alive | Alive | Unspecified |
| Year | 2013 | 2012 | 2012 | 2010 | 2008 | 2008 | 2007 | 2001 | 2001 | 2000 |
| Country | China | Turkey | India | Spain | Canada | China | USA | France | France | USA |
| First author | Present case | Aslan et
al | Dhawan et
al | Conejeros et
al | O’Sullivan et
al | Wang et
al | Lai et
al | Rangheard et
al | Rangheard et
al | Silverman et
al |
| Reference | | (5) | (6) | (7) | (8) | (9) | (10) | (11) | (11) | (12) |
Case report
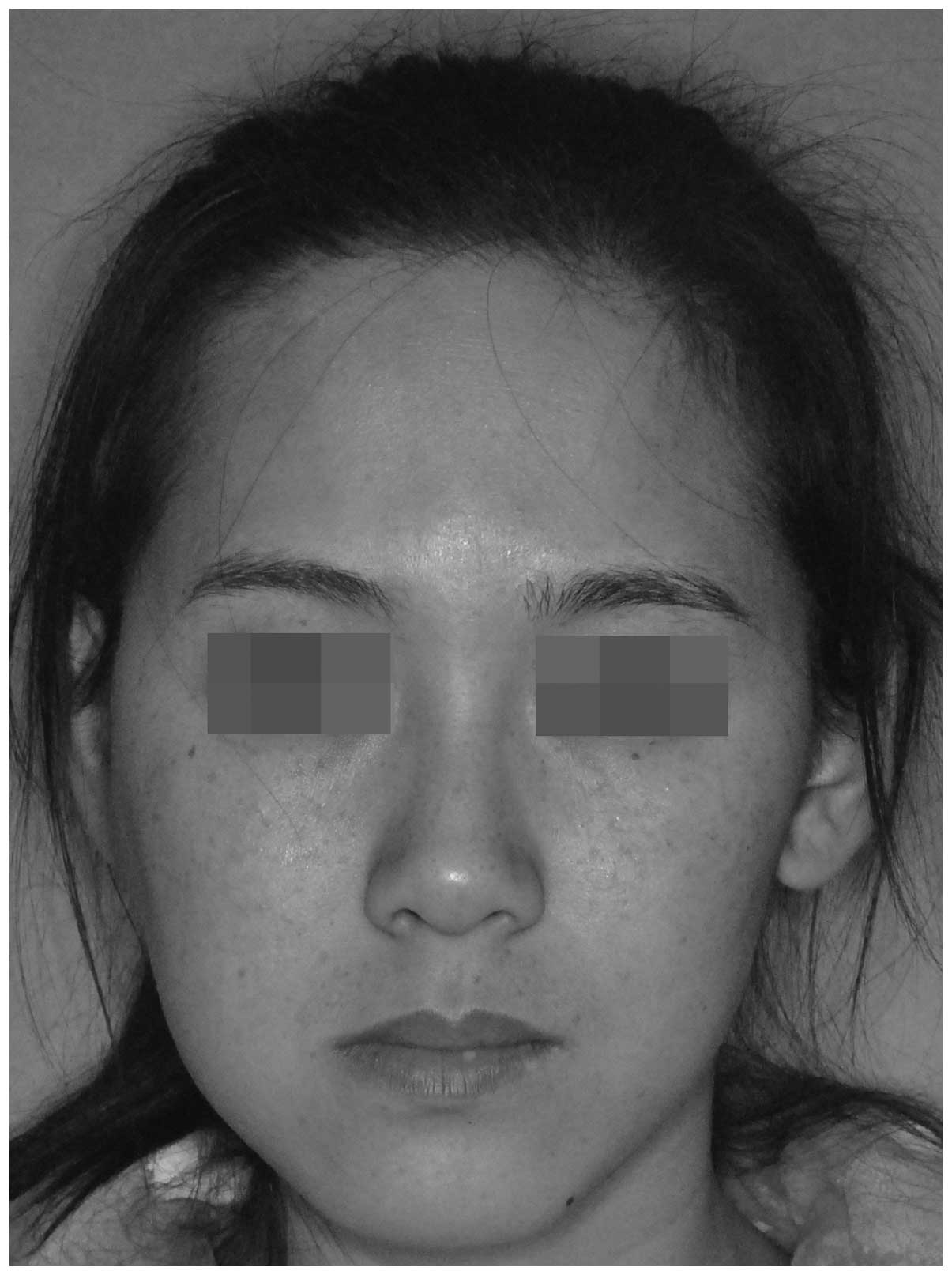
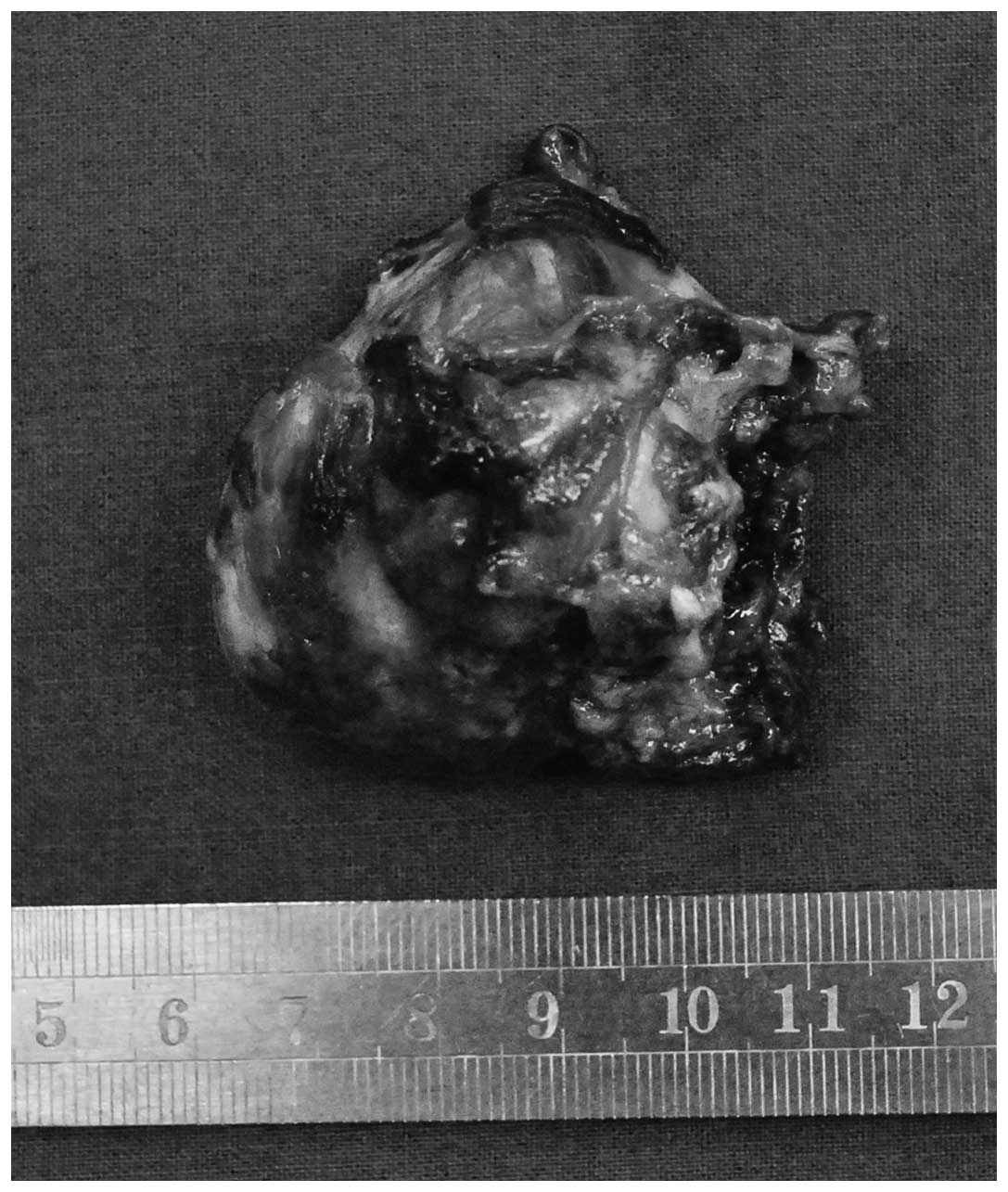
A 23-year-old female was referred to the Stomatology
Hospital of Xi’an Jiao Tong University (Xi’an, China) for
consultation, due to painless swelling of the right cheek that had
been present for five months. The patient had no history of trauma
or facial surgery. Upon physical examination, facial asymmetry and
slight right-sided cheek swelling was observed (Fig. 1). The maximum extent that the mouth
could be opened was 2.8 cm and the occlusal relationship was
normal. A palpable mass without tenderness was present in the
posterolateral wall of the right maxillary sinus; the mass was
moderate in hardness and slight mobile. However, the whole body of
the mass could not be assessed. There was no involvement of the
oral mucosa and the lymphadenopathy was negative. The evaluation of
the cranial nerves returned results within the normal limits. With
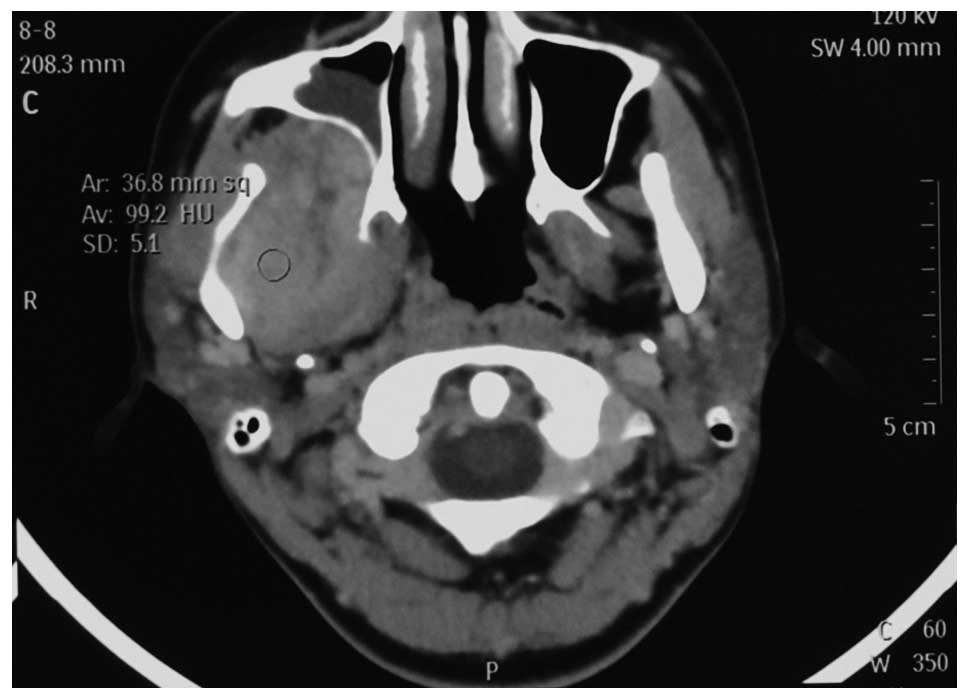
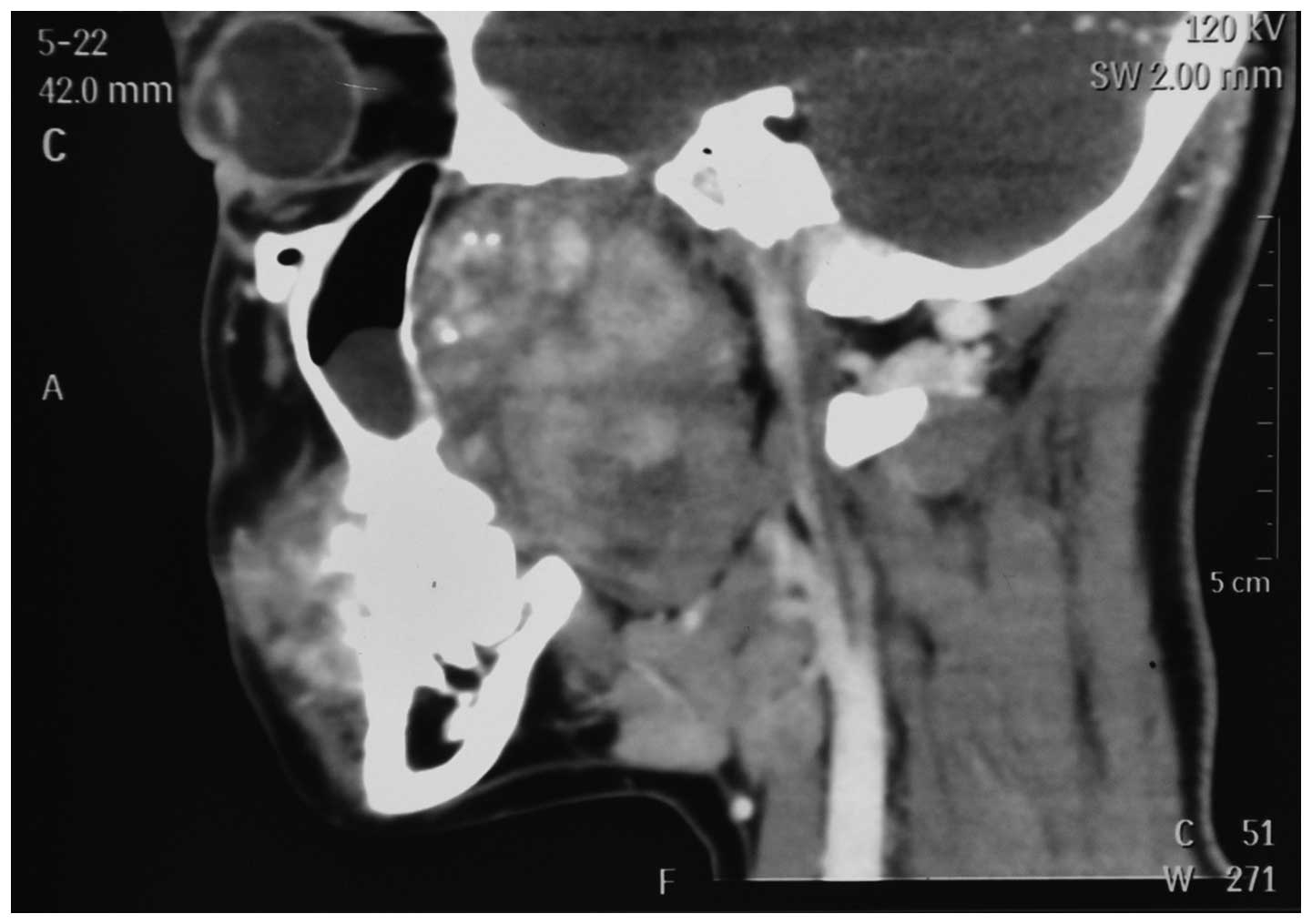
the suspicion of a tumor from the right ITF, imaging examinations
were performed. Computed tomography (CT) demonstrated a soft-tissue
mass in the right ITF, compressing the posterolateral wall of the
right maxillary sinus and causing deformity without osteolysis. The
foramen ovale was also enlarged (Figs.
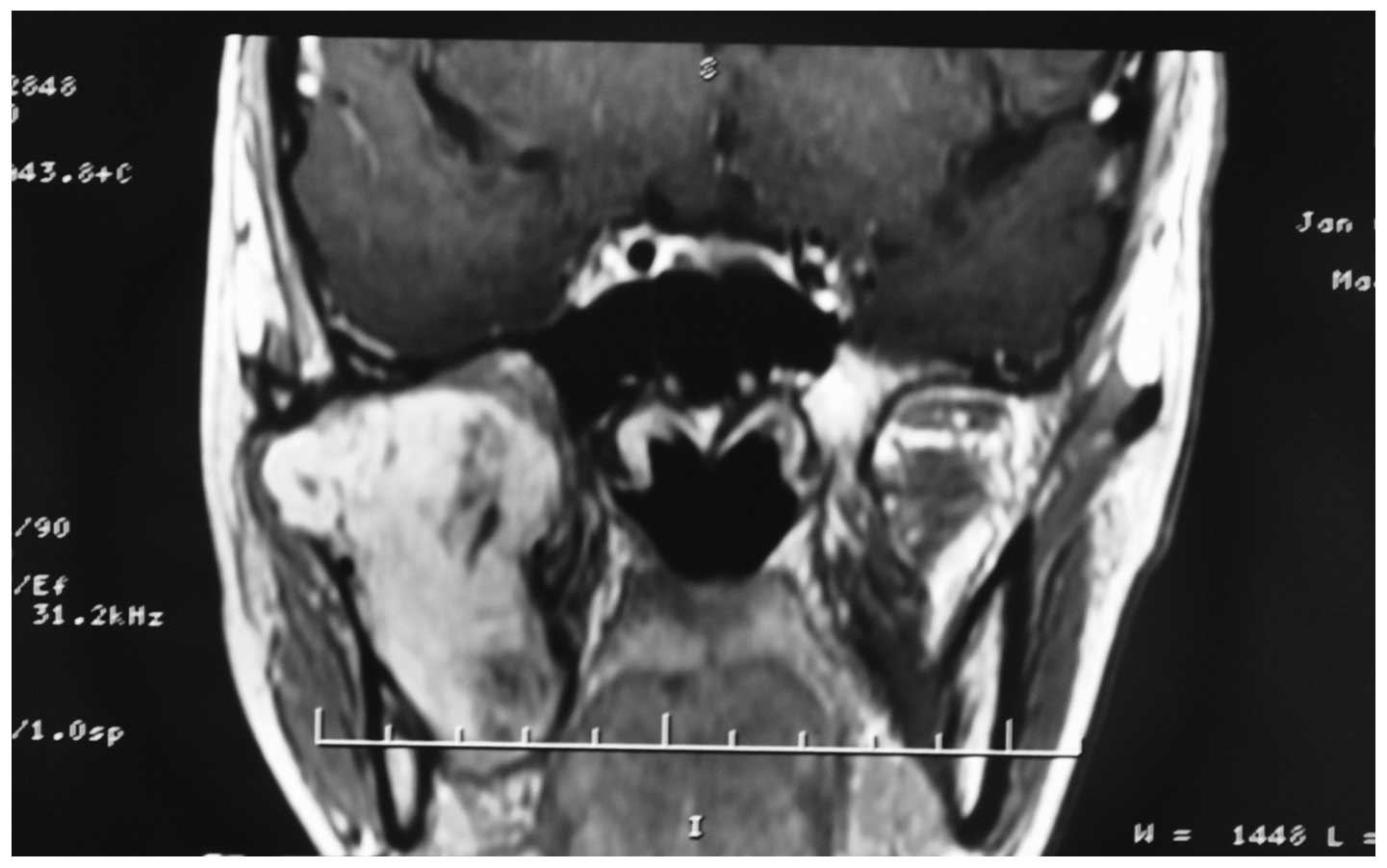
2 and 3). Magnetic resonance
imaging (MRI) revealed a 5.1×3.6-cm mass filling the superior and
inferior aspects of the ITF (Fig.
4). The patient was otherwise healthy, with complete dentition.
Fine-needle aspiration cytology (FNAC) was performed
pre-operatively via an intraoral approach, but it did not result in
a definitive diagnosis. Based on the clinical presentation and
uncommon imaging manifestations with destruction of the foramen
ovale, the primary diagnosis was of a malignant tumor. Next, the
patient underwent surgical excision under general anesthesia
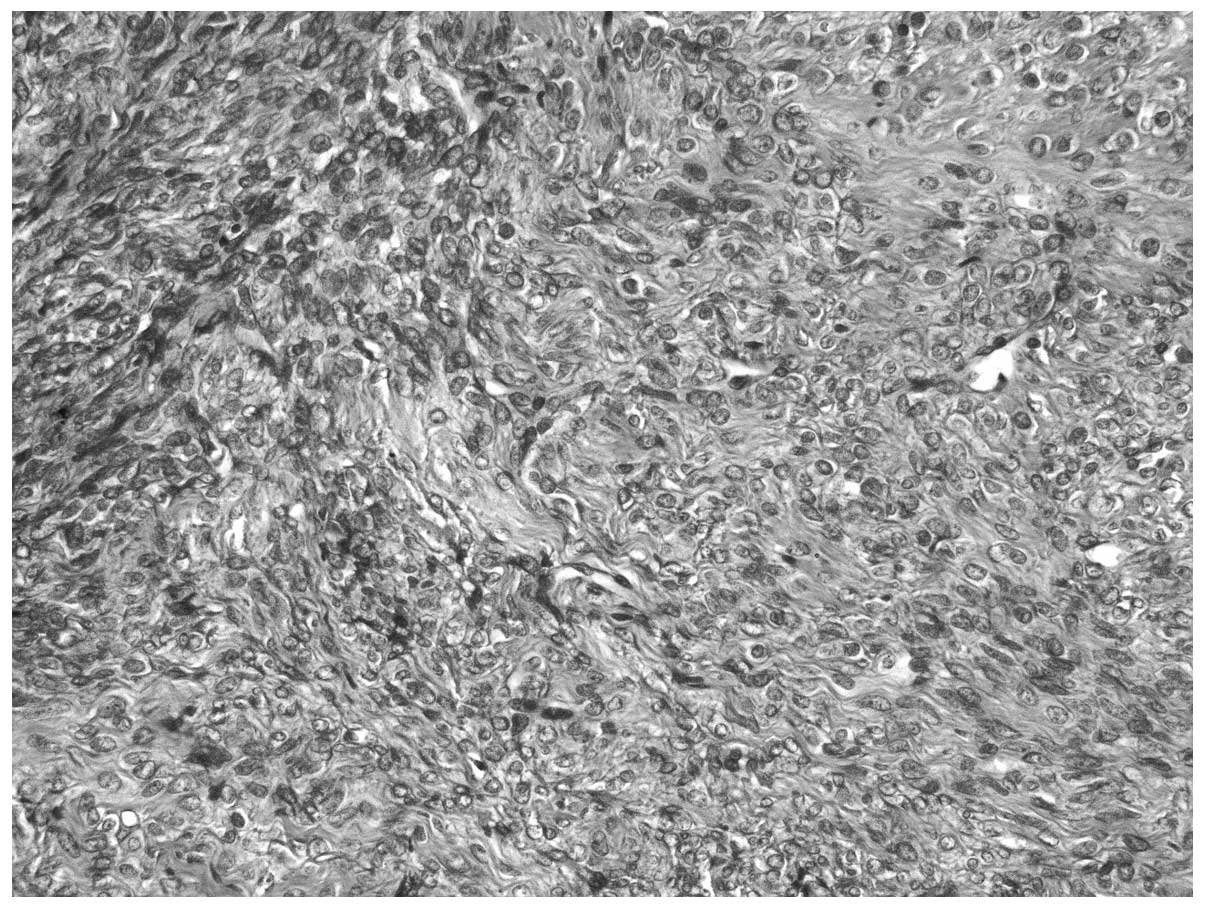
(Fig. 5). A frozen biopsy sample
was obtained intraoperatively, yielding the following microscopic
results: The tumor was composed of uniformly shaped spindle cells,
with a higher proportion of nuclei, and plasma with a rare mitotic
phenomenon (Fig. 6). Surgical
margins were microscopically tumor-free and the dura was intact.
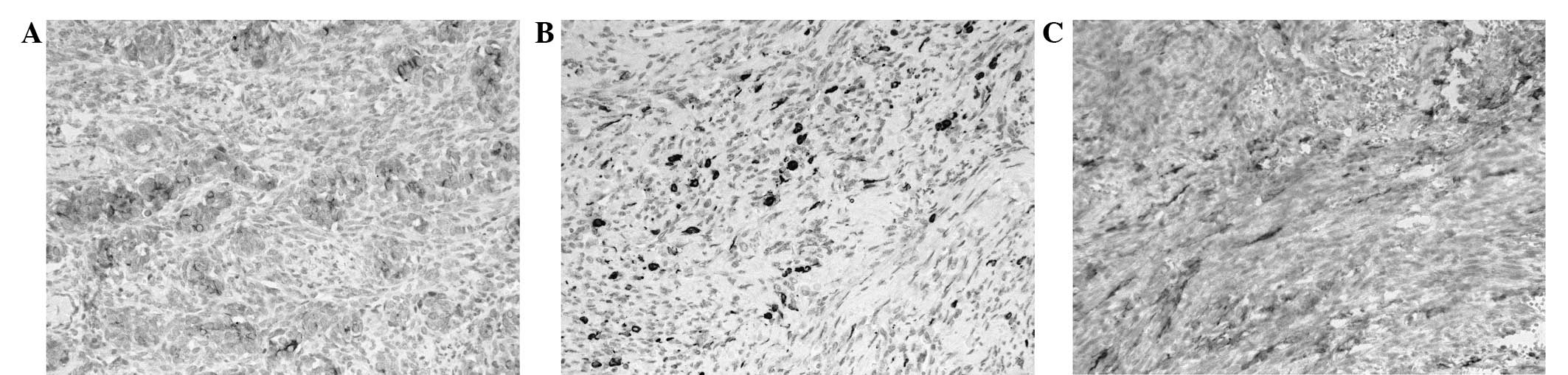
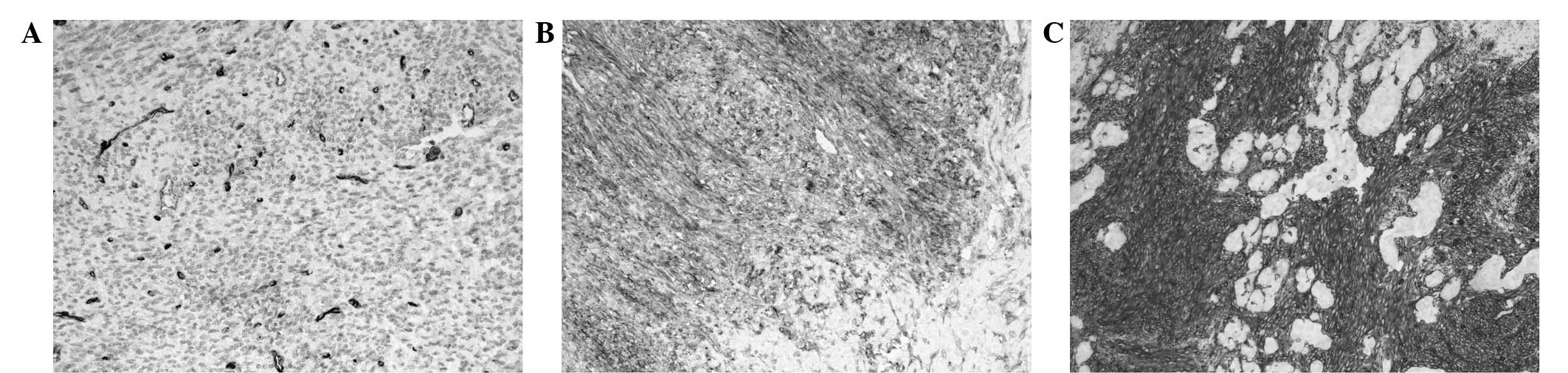
There was no cerebrospinal fluid leakage. Immunohistochemistry was
performed post-operatively and the results showed that the tumor
cells were positive for epithelial markers, cytokeratin 7 (CK7),
CK19 and epithelial membrane antigen (EMA) (Fig. 7), and mesenchymal markers, cluster
of differentiation (CD)34, CD99 and Vimentin (Vim) (Fig. 8). The tumor cells were negative for
p63, smooth muscle actin and S-100. The tumor was subsequently
diagnosed as biphasic SS. Treatment with a total of 60 Gy adjuvant
radiotherapy and chemotherapy, consisting of cisplatin (25
mg/m2 intravenously on days one to three), epirubicin
(25 mg/m2 intravenously on days one and two) and
ifosfamide (1.8 g/m2 intravenously on days one to five)
for three cycles was administered to prevent local recurrence and
distant metastasis. At the 24-month follow-up neither local
recurrence nor metastatic disease were apparent. Written informed
patient consent was obtained for publication of this study.
Discussion
A review of the English literature revealed that a
total of 10 cases, including the present case (Table I), regarding SS arising from the ITF
have been reported, making this an extremely rare entity. This
poses a challenge for physicians to define its clinical behavior
and to standardize a management strategy. All reported series of SS
in the head and neck are sporadic and comparisons are difficult.
According to the largest series from the MD Anderson Cancer Center
(Houston, TX, USA), the median age of patients with SS of the head
and neck was 29 years (mean, 30.6 years; range, 5–55 years), and
73% of occurrences were male and 27% were female (4). Another study also reported similar age
ranges (13). Of the ten cases
identified in the present review, the ages ranged between 7 and 82
years, with a mean of 38.6 years. In contrast to the MD Anderson
Cancer Center study, there was a female predominance, with a female
to male ratio of 4:1.
The tumor site determines the clinical presentation
of the head and neck SS (4). The
ITF, by virtue of its relatively concealed location, is
inaccessible for clinical examination of the tumor in the early
stages. Space-occupying lesions in this area may continue to grow
unnoticed for a considerable period. Clinically, SS of the ITF
appears as a deep-seated, painless and slow-growing mass, and is
usually asymptomatic until it attains a size sufficient enough to
create pressure on the adjacent structures. In the current review,
the mean tumor size was 5.9 cm (range, 3.2–13 cm), and it took 5–12
months for these patients to seek first medical care. In the cases
with reported symptoms, SS in the ITF manifested with painless
check swelling (1/7; present case), local pain (4/7), restriction
of mouth opening (2/7) and migraines (1/7). In case 4, the tumor
presented with local pain associated with asthenia, anorexia and
weight loss (12.0 kg) over 6 months of progression. In cases 3 and
4, tumors in the advanced stage invaded the oral cavity and
presented with oral masses; thus, the growth was similar in
appearance to squamous cell carcinoma arising from the maxillary
sinus (particularly from the posterior wall) and retromolar
triangle (Table I).
Tumors of the ITF present with a wide spectrum of
pathologies, both benign and malignant (14). A smaller number of tumors,
particularly those rare entities such as SS, originate from the
tissues in this space, making them difficult to diagnose correctly.
SS of the head and neck may usually mimic the benign neoplasms in
CT and MRI, with well-defined, smooth margins and a lack of
aggressive infiltration (11,15).
Indeed, its heterogeneity in appearance with septations,
hemorrhage, cysts, calcification or multilocularity should raise
the suspicion of an SS (15). CT
and/or MRI was performed in 9 cases of SS in association with the
ITF, including the present case. Three cases presented with a
heterogeneous mass and calcification (3/9); one case with septation
(1/9); another case presented with a homogeneous cystic mass (1/9);
seven with tumors extending into the surrounding soft tissue (7/9);
six presented with infiltration into the bony structures except the
skull base (6/9); and two cases exhibited intracranial extension
(foramen ovale) (2/9). As indicated by the present review, physical
examinations and CT/MRI imaging were extremely useful to disclose
local invasion and metastasis at the time of presentation.
Lymphadenopathy was not detected in any of these cases.
The diagnosis of SS is made on the basis of its
relatively distinctive, yet markedly variable, histopathological
appearance, in conjunction with histochemical findings,
immunohistochemistry, electron microscopy and cytogenetic analysis,
which have proved valuable in confirming the morphologic diagnosis
(16,17). Two morphologically distinct, but
histogenetically-related cell types form SS and cause the
characteristic biphasic pattern. SS form a continuous
histopathological spectrum, with biphasic, monophasic epithelial,
monophasic fibrous and poorly-differentiated (round cell) types,
depending on the relative prominence of the two cell populations
and the degree of differentiation (1). Biphasic SS is effectively diagnosed by
its unique histopathological features, however, it is difficult to
diagnose monophasic SS. Therefore, immunohistochemistry has a
significant role in the diagnosis of SS. The present case analysis
demonstrated a monophasic:biphasic ratio of 1:1. The literature
review demonstrated that an immunohistochemical analysis was
performed in seven of the known cases, including four cases of
biphasic SS, two cases of monophasic SS and another unspecified
case. The most commonly positive epithelial markers were EMA (6/7)
and CK (5/7), while the mesenchymal markers were CD99 (4/7) and Vim
(4/7). There was no significant difference between monophasic and
biphasic SS with respect to their immunohistochemical features. The
differential diagnosis for this condition includes fibrosarcoma,
Ewing’s sarcoma, leiomyosarcoma, malignant nerve sheath tumors,
hemangiopericytoma and squamous cell carcinoma (18).
In the present case, the diagnosis of biphasic SS
was made from the histopathological findings and supporting
immunohistochemical features. FNAC was performed pre-operatively
and yielded no definitive diagnosis. In fact, of the four patients
that underwent FNAC in the reviewed cases, only one case led to a
confirmed diagnosis, indicating the limited nature of this
technique as a routine diagnostic procedure.
The optimal approach to the treatment of this
malignancy remains undefined and there is no standard treatment
protocol for SS of the head and neck (4). From the analysis of the nine previous
reports, it was apparent that the treatment protocol of the SS
arising from the ITF was inconsistent, consisting of the following
combinations: Surgery only (2/6), surgery and radiotherapy (1/6),
surgery and chemotherapy (1/6), surgery, chemotherapy and
radiotherapy (3/6), and radiotherapy and chemotherapy (1/6).
Generally, radical surgery represented the first approach (6/7).
However, a radical excision with wide margins is rarely possible
due to the anatomical site. With respect to the present patient
with intracranial extension, surgery and chemoradiotherapy were
applied.
For soft-tissue sarcomas in general, the prognosis
is associated with the resection margins (19). SS, one of the highly malignant
tissue sarcomas, remains a disease with a poor prognosis, having an
overall five-year survival rate of 57% (18). For head and neck SS, the 5-year
disease-specific survival rate has been recorded as 72%, and
survival rates have been found to be associated with tumor
location, size, and extension (4).
Of the eight patients with a known outcome in the literature, the
median follow-up period was 71.5 months (range, 12–192 months). As
a result, six patients with combined therapy were disease-free
(6/8). One case thatwas treated exclusively with chemotherapy and
radiotherapy, but not surgery, remained unchanged following 180
months of follow-up, with no signs of tumor aggressiveness. One
patient developed multiple pulmonary and pleural metastases, and
eventually succumbed to the disease 14 months post-operatively. It
is noteworthy that this patient received only surgery, and
exhibited a large tumor of 7.0 cm in diameter, plus surrounding
soft tissue extension and bony infiltration. Another patient with
recurrent disease was a 7-year-old female who suffered from
multiple lung and chest wall metastases at 192 months
post-treatment. However, further information concerning the
clinicopathological characteristics and treatment options in this
case are not available. These cases may advocate the importance of
multidisciplinary management in this rare entity with or without
surrounding soft/bony tissue extension.
Recently, Aslan et al reported a similar case
of SS in the ITF with intracranial extension (5). In this case, the tumor invaded the
foramen ovale, but was not involved with the surrounding soft
tissue or bony structures; the mass was surgically removed en-bloc
and received chemoradiotherapy post-operatively. Unlike the present
case, the tumor was small at only 3.3 cm in diameter, but was much
more aggressive; it destroyed a 0.5×0.5-cm area of bone
posterolateral to the foramen ovale, although the dura remained
intact. Surgicel (Johnson & Johnson Medical Ltd., Zug,
Switzerland) was applied to the destroyed area and there was no
cerebrospinal fluid leakage. Following the use of multidisciplinary
management, the patient had a good prognosis at the 12-month
radiological follow-up.
Due to the limited number of ITF cases, every new
case will highlight novel information about management strategies
and prognosis. The current study presented an extremely rare case
of primary SS in the ITF with intracranial involvement. Albeit with
only a short follow-up period, the patient achieved good outcome
after multimodal therapy. Based on a review of the literature, SS
in the ITF is insidious due to its special anatomical features in
the skull base, and it may not be noticed until there is impairment
of function and the appearance of symptoms. CT and MRI are useful
non-invasive diagnostic tools, and the final diagnosis of SS is
made on the basis of unique pathological and immunohistochemical
findings. In this rare entity with or without surrounding soft/bony
tissue extension, multimodal therapy with surgical excision
followed by early post-operative chemoradiotherapy can be a
promising factor controlling local recurrence and distant
metastasis.
Acknowledgements
This Study was supported by The Shanghai Committee
of Science and Technology Funds (grant no. 12DZ2260100) and The
Fundamental Research Funds for the Central Universities (grant no.
XJJ 2013061).
References
|
1
|
Bergh P, Meis-Kindblom JM, Gherlinzoni F,
et al: Synovial sarcoma: identification of low and high risk
groups. Cancer. 85:2596–2607. 1999.
|
|
2
|
Fisher C: Synovial sarcoma. Ann Diagn
Pathol. 2:401–421. 1998.
|
|
3
|
Kransdorf MJ: Malignant soft-tissue tumors
in a large referral population: distribution of diagnoses by age,
sex, and location. AJR Am J Roentgenol. 164:129–134. 1995.
|
|
4
|
Harb WJ, Luna MA, Patel SR, et al:
Survival in patients with synovial sarcoma of the head and neck:
association with tumor location, size, and extension. Head neck.
29:731–740. 2007.
|
|
5
|
Aslan H, Başoğlu MS, Erdoğan NK, et al:
Synovial sarcoma of the infratemporal fossa with intracranial
extension. Kulak Burun Bogaz Ihtis Derg. 22:348–353. 2012.
|
|
6
|
Dhawan A, Shenoy AM, Chavan P, Sandhu S
and Sriprakash D: Synovial sarcoma of the infratemporal fossa with
extension into the oral cavity - a rare presentation and literature
review. J Oral Maxillofac Surg. 70:2923–2929. 2012.
|
|
7
|
Tamarit Conejeros JM, Estrems Navas P,
Estellés Ferriol E and Dalmau Galofre J: Synovial sarcoma of the
infratemporal fossa. Acta Otorrinolaringol Esp. 61:389–391.
2010.(In Spanish).
|
|
8
|
O’Sullivan PJ, Harris AC and Munk PL:
Radiological features of synovial cell sarcoma. Br J Radiol.
81:346–356. 2008.
|
|
9
|
Wang H, Zhang J, He X and Niu Y: Synovial
sarcoma in the oral and maxillofacial region: report of 4 cases and
review of the literature. J Oral Maxillofac Surg. 66:161–167.
2008.
|
|
10
|
Lai V, Farrag TY, Cao D, et al: Synovial
sarcoma of the infratemporal fossa. Am J Otolaryngol. 28:444–447.
2007.
|
|
11
|
Rangheard AS, Vanel D, Viala J, et al:
Synovial sarcomas of the head and neck: CT and MR imaging findings
of eight patients. AJNR Am J Neuroradio. 22:851–857. 2001.
|
|
12
|
Silverman JF, Landreneau RJ, Sturgis CD,
et al: Small-cell variant of synovial sarcoma: Fine-needle
aspiration with ancillary features and potential diagnostic
pitfalls. Diagn Cytopathol. 23:118–123. 2000.
|
|
13
|
Kartha SS and Bumpous JM: Synovial cell
sarcoma: diagnosis, treatment, and outcomes. Laryngoscope.
112:1979–1982. 2002.
|
|
14
|
Tiwari R, Quak J, Egeler S, et al: Tumors
of the infratemporal fossa. Skull Base Surg. 10:1–9. 2000.
|
|
15
|
Hirsch RJ, Yousem DM, Loevner LA, et al:
Synovial sarcomas of the head and neck: MR findings. AJR Am J
Roentgenol. 169:1185–1188. 1997.
|
|
16
|
Sharif MA, Mushtaq S, Mamoon N, Khadim MT
and Asghar Z: Biphasic synovial sarcoma of oral cavity. J Coll
Physicians Surg Pak. 18:713–715. 2008.
|
|
17
|
Åkerman M, Ryd W and Skytting B:
Fine-needle aspiration of synovial sarcoma: criteria for diagnosis:
retrospective reexamination of 37 cases, including ancillary
diagnostics. A Scandinavian Sarcoma Group study. Diagn Cytopathol.
28:232–238. 2003.
|
|
18
|
Spillane AJ, A’Hern R, Judson IR, Fisher C
and Thomas JM: Synovial sarcoma: a clinicopathologic, staging, and
prognostic assessment. J Clin Oncol. 18:3794–3803. 2000.
|
|
19
|
Gronchi A, Casali PG, Mariani L, et al:
Status of surgical margins and prognosis in adult soft tissue
sarcomas of the extremities: a series of patients treated at a
single institution. J Clin Oncol. 23:96–104. 2005.
|