Introduction
Cysts that form in patients with prostate cancer are
a type of acquired cyst (1). In
prostate cancer, cysts are either secondary cysts caused by
intra-cancerous tissue hemorrhage or central necrosis of the cancer
tissue, or primary cysts associated with the cancer (2). The majority of cysts that form in
prostate cancer patients are secondary cysts (3). In Japan >100 cases have been
reported of prostate cancer with cyst formation (3,4). The
majority were symptomatic and detected by ultrasound or computed
tomography (CT). In total >50% of reported cases presented with
metastatic cancer and endocrine therapies were selected for the
patient and surgery was only performed for localised disease
(5). Nearly all patients were
diagnosed with conventional acinar adenocarcinomas from the
histology. However, papillary cystadenocarcinomas, embryonal
rhabdomyosarcoma and phyllodes tumors are rare (5–7). The
present study reports a case of cyst formation in a patient with
prostate cancer, secondary to a conventional adenocarcinoma. The
patient provided informed consent.
Case report
A 72-year-old male was diagnosed with multiple lung
metastases by chest radiography and CT during a health examination
at a local clinic. The patient was referred to Tokai University
Hachioji Hospital (Tokyo, Japan) for examination and diagnosis of
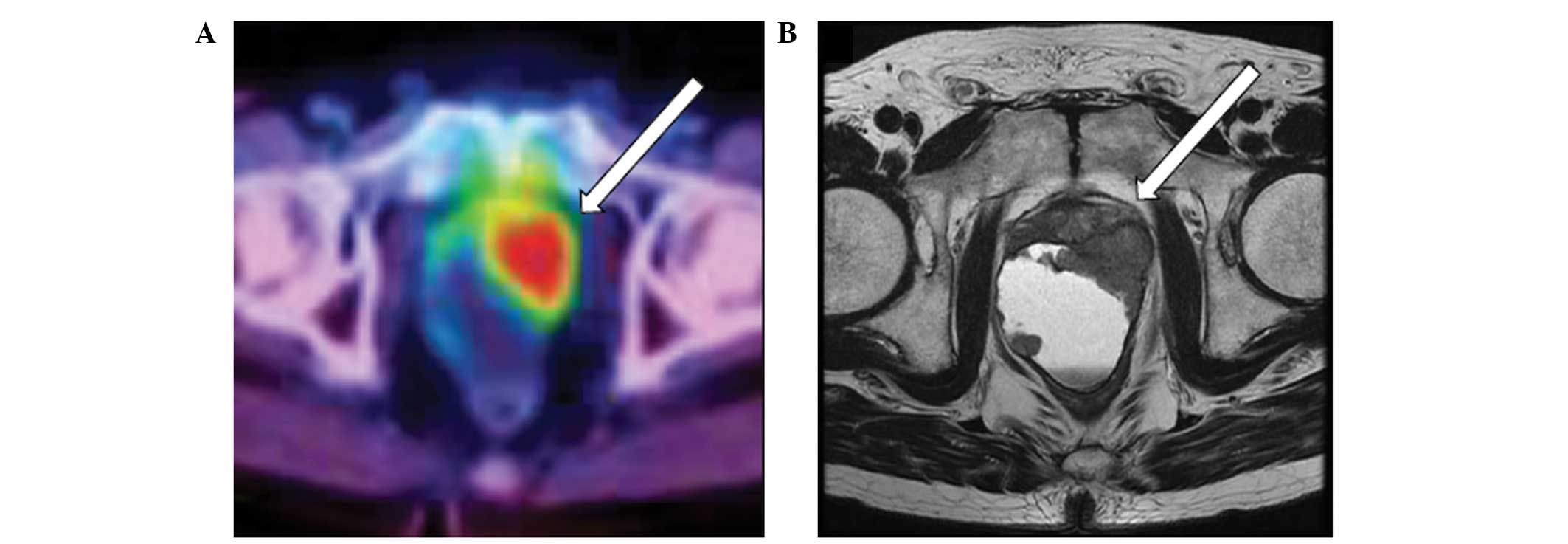
the primary tumor. Whole body
[18F]-fluoro-deoxy-2-glucose positron emission
tomography (FDG-PET)/CT showed strong accumulation in the pelvis
(Fig. 1). Pelvic magnetic resonance
imaging (MRI) revealed a 60×40-mm cystic lesion, with an irregular
thickened wall, behind the left lobe of the prostate (Fig. 1); this finding was consistent with
the FDG accumulation observed on PET/CT. A transperineal needle
biopsy was performed once the serum prostate-specific antigen (PSA)
level was found to be elevated to 211.99 ng/ml (normal range, 4.0
ng/ml). Histological examination of the needle biopsy specimens of
the cystic wall and prostate gland revealed
moderately-differentiated adenocarcinoma (Gleason score 4+3)
(8). The contents of the cyst were
bloody. The cytological findings revealed no malignancy, but the
PSA level of the cystic contents was 45,130 ng/ml. Whole body CT
and bone scans revealed no metastasis other than that in the lung,
and the patient was diagnosed with prostate cancer with multiple
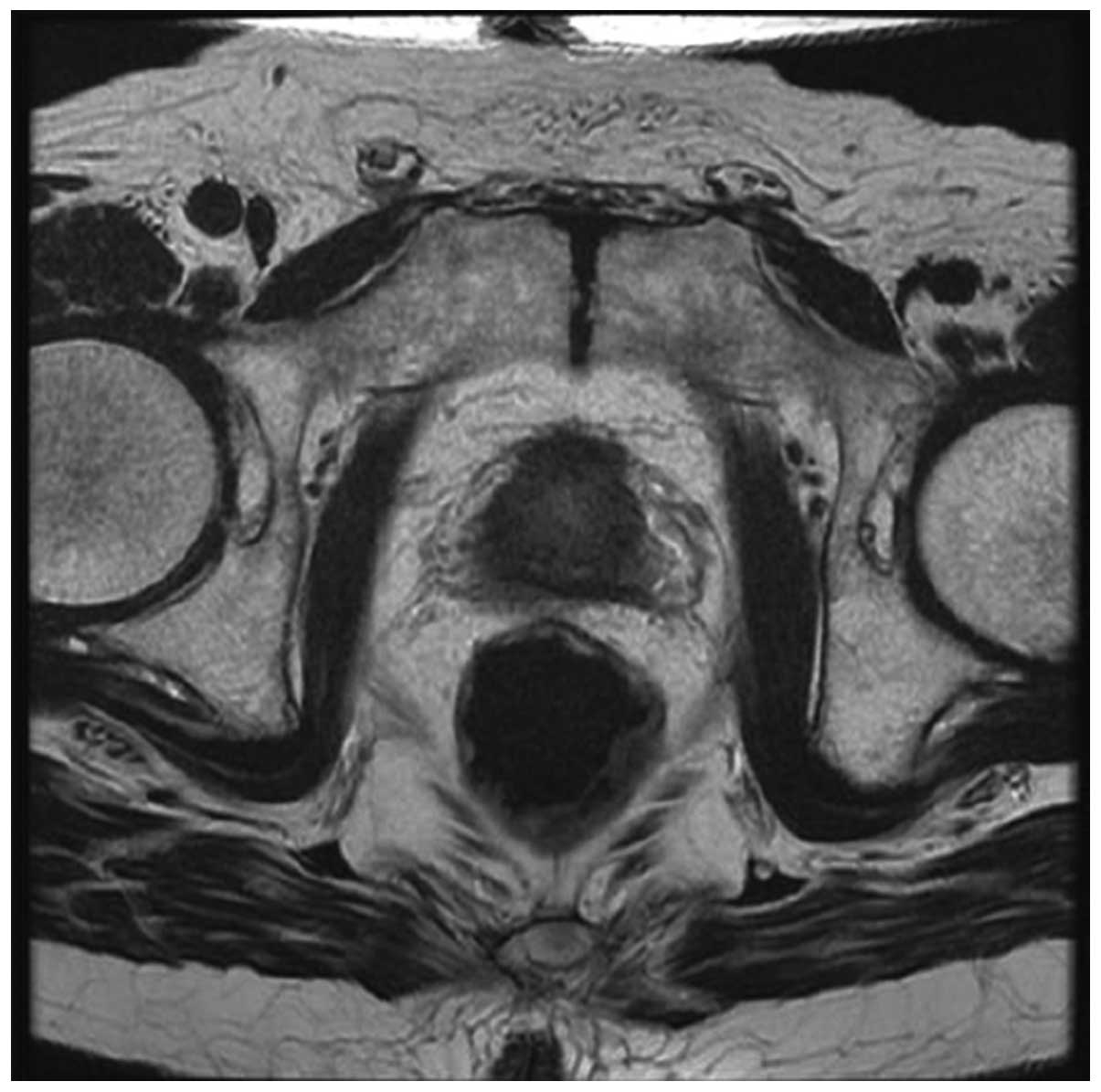
lung metastases. Following 8 months of androgen deprivation therapy
(ADT), the cyst shrank (Fig. 2) and
the serum PSA level decreased to 0.14 ng/ml. At the 24-month
post-ADT follow-up examination, the PSA level was 0.19 ng/ml and
the cyst continued to shrink.
Discussion
In prostate cancer, cysts are considered either
secondary cysts caused by intra-cancerous tissue hemorrhage or
necrosis of the cancer tissue, or primary cysts associated with
cancer (2). In a recent Japanese
study of 96 patients with prostate cancer with cyst formation, the
majority were symptomatic (dysuria was reported in 56.2% of cases
and hematuria in 20.8% of cases), more than half presented with
metastatic cancer (54.1%) and almost all were diagnosed with
secondary cyst formation (82.1%) (3). In the present case, although a cyst
with a diameter of ~6 cm was detected in the small pelvis, the
patient was asymptomatic.
It is difficult to predict tissue type without
histological examination by MRI or PET/CT. Although only the
pathological data acquired by prostate biopsy was obtained, the
cystic fluid was bloody with a high PSA level. Based on these
results, we speculate that the cyst was a secondary cyst that
formed in the prostate cancer patient.
The various histological types of malignant lesions
with gross cystic sections in the prostate have been previously
reported in the literature, and include conventional acinar
adenocarcinomas, papillary cystadenomas (4), embryonal rhabdomyosarcomas (6) and phyllodes tumors (7). Ideally, the histological type of
prostate cancer should be determined prior to the start of
treatment. The present patient did not exhibit the typical clinical
manifestation of conventional acinar adenocarcinoma, but the
pathological examination indicated acinar prostate adenocarcinoma.
Therefore, the standard therapy for metastatic prostate
adenocarcinoma was chosen, which was extremely effective.
FDG-PET/CT is of limited value for detecting
prostate cancer, as only ~1% of prostate cancer lesions are
FDG-avid (9) and benign conditions
of the prostate can also show increased FDG uptake (10). However, there is evidence in the
literature that FDG-PET/CT sensitivity and a positive predictive
value to detect prostate cancer is increased up to 80 and 87%,
respectively, in tumors classified with a Gleason score of ≥7
(11). In the present case, the
thickened wall of the cyst that continued to the left lobe of the
prostate showed a high accumulation of tracer, which aided in the
decision with regard to which part of the body to examine to
identify the primary lesion of the lung metastases.
Abbreviations:
|
FDG
|
[18F]-2-fluoro-2-deoxyglucose
|
|
PET
|
positron emission tomography
|
|
CT
|
computed tomography
|
|
MRI
|
magnetic resonance imaging
|
|
PSA
|
prostate-specific antigen
|
|
ADT
|
androgen deprivation therapy
|
References
|
1
|
Emmett JL and Braasch WF: Cysts of the
prostate gland. J Urol. 36:236–249. 1936.
|
|
2
|
Kojima K, Uehara H, Naruo S, Kanayama H
and Kagawa S: Papillary cystadenocarcinoma of the prostate. Int J
Urol. 3:511–513. 1996.
|
|
3
|
Itami Y, Nagai Y, Kobayashi Y, Shimizu N,
Yamamoto Y, Minami T, Hayashi T, Nozawa M, Yoshimura K, Ishii T and
Uemura H: A case of prostatic cancer with a low PSA level
accompanied with cystic formation requiring differentiation from
adenocarcinoma of the seminal vesicle. Hinyokika Kiyo. 58:349–353.
2012.(In Japanese).
|
|
4
|
Naoe M, Ogawa Y, Fuji K, Fukagai T, Inoue
K and Yoshida H: Papillary cystadenocarcinoma of the prostate. Int
J Urol. 11:1036–1038. 2004.
|
|
5
|
Kim SC1, Fujimoto K, Matsumoto Y, et al: A
case of prostate cancer with cyst formation. Hinyokika Kiyo.
47:653–656. 2001.(In Japanese).
|
|
6
|
Niimi K, Hashimoto Y, Kurokawa S, Okada A,
Tozawa K and Kohri K: Embryonal rhabdomyosarcoma of the prostate.
Int J Clin Oncol. 15:93–96. 2010.
|
|
7
|
Chung HC, Lee HS, Kim TI, Kim DI, Park KH
and Song JM: A large cystic phyllodes tumor of the prostate. Yonsei
Med J. 50:174–176. 2009.
|
|
8
|
Epstein JI, Allsbrook WC Jr, Amin MB, et
al: The 2005 International Society of Urological Pathology (ISUP)
Consensus Conference on Gleason Grading of prostatic carcinoma. Am
J Surg Pathol. 29:1228–1242. 2005.
|
|
9
|
Hinev A, Chaushev B and Klisarova A: FDG
PET/CT in prostate cancer: A valuable method to detect the primary
and metastatic tumor sites and to monitor cancer response to
hormonal therapy. Nephrourol Mon. 4:644–645. 2012.
|
|
10
|
Han EJ, JH O, Choi WH, Yoo IR and Chung
SK: Significance of incidental focal uptake in prostate on
18-fluoro-2-deoxyglucose positron emission tomography CT images. Br
J Radiol. 83:915–920. 2010.
|
|
11
|
Minamimoto R, Uemura H, Sano F, Terao H,
Nagashima Y, Yamanaka S, Shizukuishi K, Tateishi U, Kubota Y and
Inoue T: The potential of FDG-PET/CT for detecting prostate cancer
in patients with an elevated serum PSA level. Ann Nucl Med.
25:21–27. 2011.
|