Introduction
Giant cell tumor of the tendon sheath (GCT-TS) is a
benign soft tissue tumor of the tendon sheath and synovium
(1). GCT-TS is the second most
common type of tumor of the hand, and gnalgion cysts are the most
common (2). The majority of GCT-TS
cases occur in the fingers and toes, however, rare cases of GCT-TS
occur in the knee, exhibiting a nodular pattern of growth (2). GCT-TS usually occurs in individuals
between the ages of 30 and 50 years, with a predominance for
females, and exhibit the capacity for local recurrence following
surgical resection (1). Marginal
excision is the standard treatment for of GCT-TS. However, despite
its benign character, the rate of local recurrence following
excision has been reported to range between 10 and 20% (1). The high local recurrence rate may be
due to the fact that complete excision may be difficult, as the
mass is frequently associated with the tendon sheath or synovial
joint. The current report presents an unusual case of GCT-TS
arising from the patellar tendon sheath, extending into the knee
joint and involving the tibia. Information provided by the present
report may assist clinicians in establishing a more informed
diagnosis and administering the correct treatment. Written informed
consent was obtained from the patient.
Case report
In December 2012, a 41-year-old male with a 15-year
history of a slow-growing, painless mass in the left knee and no
history of trauma was referred to Shinshu Ueda Medical Center
(Ueda, Japan) by the patient’s doctor.
Physical examination revealed a mass, 8 cm in
diameter, in the anterior aspect of the left knee (Fig. 1). No localized warmth, redness or
tenderness was observed in the left knee, however, there was
minimal effusion. The range of motion was 0–125° degrees in the
left knee compared with 0–140° in the right knee. The patient
displayed normal gait and no neurovascular deficit was
observed.
Plain lateral radiographs identified bone erosion in
the proximal tibia (Fig. 2),
however, no bone lesions were observed in the distal femur and
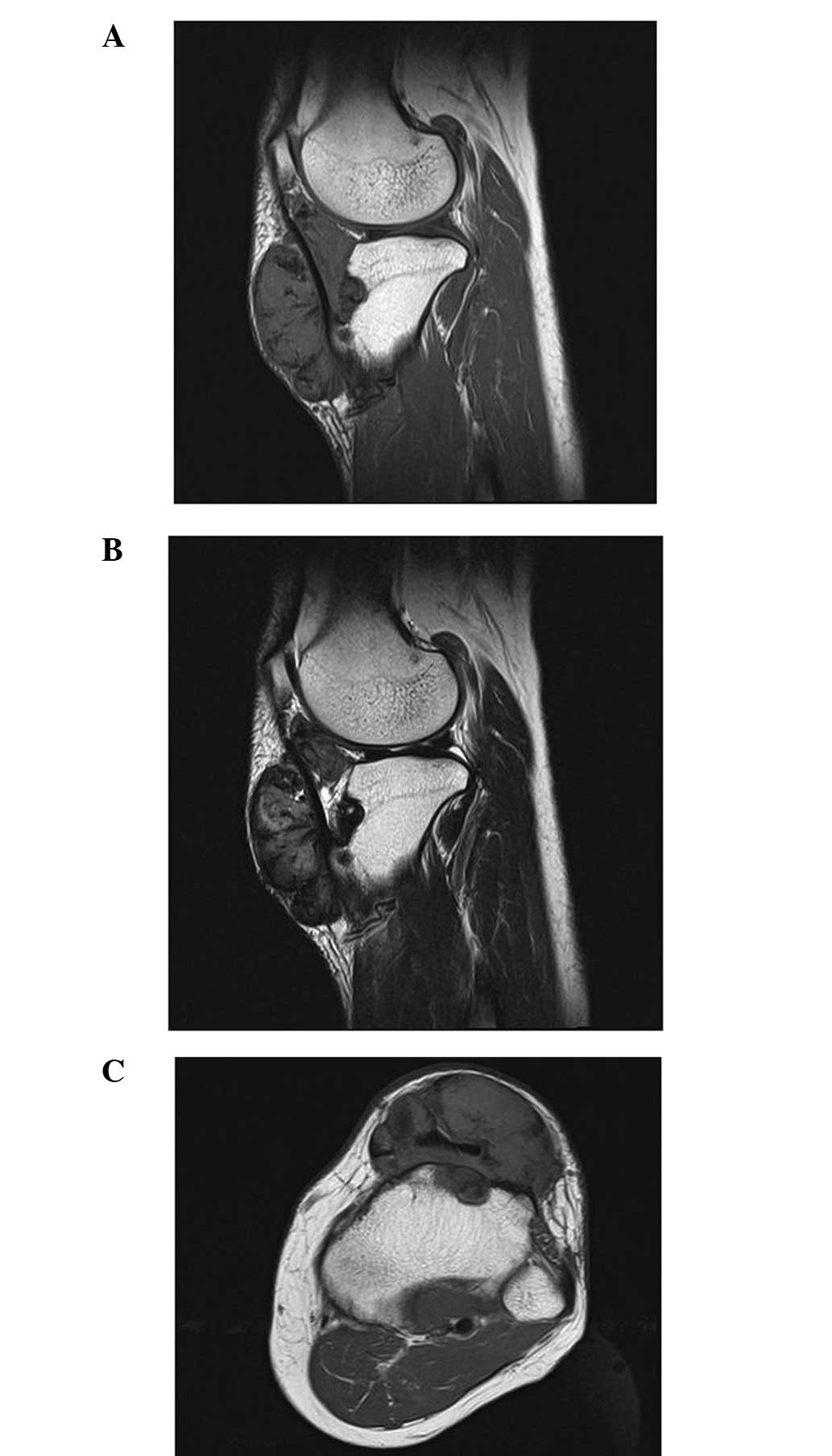
patella. Magnetic resonance imaging (MRI) identified a
well-localized mass that extended from the subcutaneous tissue in
the anterior aspect of the knee to the infrapatellar fat pad, and
deep into the patellar tendon and tibia, exhibiting a homogenous
low signal intensity on T1-weighted [repetition time (TR)/echo time
(TE), 540/12 msec] and T2-weighted (TR/TE, 4000/84 msec) images and
diffuse enhancement (Fig. 3A and
B). An axial image revealed that the tumor was wrapped around
the patellar tendon (Fig. 3C).
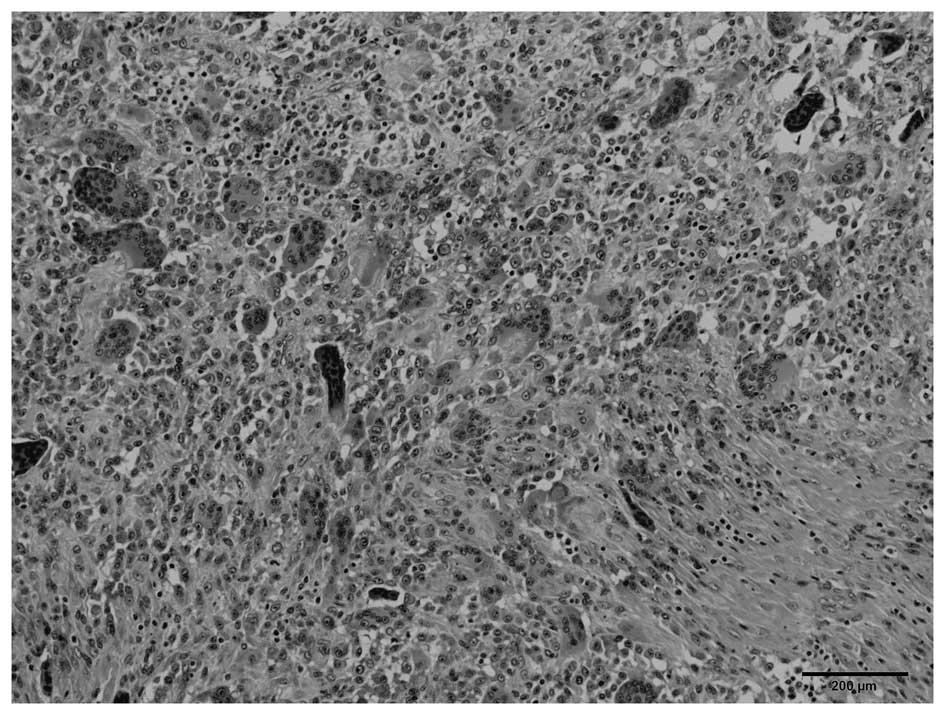
Histopathological examination of the biopsy specimen
revealed prominent histiocytes, as well as a variable number of
foamy cells, hemosiderin-laden macrophages and multinucleated giant
cells (Fig. 4). No mitotic activity
or malignant features were observed, thus, the preoperative
diagnosis was determined as GCT-TS. Although the most appropriate
surgical treatment of GCT-TS is marginal resection, in the present
case, en bloc marginal resection could not be achieved; therefore,
a piecemeal resection was performed and the patellar tendon
remained intact.
The postoperative recovery period was uneventful.
The patient regained full range of motion of the knee joint and at
the one-year follow-up the patient was asymptomatic. Repeat MRI
scans revealed no evidence of recurrence.
Discussion
The diffuse forms of pigmented villonodular
synovitis (PVNS) and GCT-TS are classified as fibrohistiocytic
tumors by the World Health Organization (3). GCT-TS occurs more frequently in the
digits of the hands and feet compared with in the larger joints;
whereas PVNS (also termed diffuse-type giant cell tumors)
infiltrate and grow as diffuse tumors in large joints, such as the
knee, elbow and ankle (3–5). While patients exhibiting diffuse-type
PVNS in the knee typically present with hemarthrosis, patients
exhibiting nodular-type GCT-TS typically present with a painless
mass. However, certain GCT-TS in the knee joint cause continuous
anterior knee pain and/or a locking knee (6,7).
The diagnosis of GCT-TS in the digits is considered
to be straightforward; patients typically present with a painless
mass, the lesion is usually well-circumscribed and localized, and
it infrequently erodes or infiltrates adjacent bone (8). However, GCT-TS in large joints may be
more difficult to diagnose, as there are few symptoms, which are
non-specific (9). In such cases,
differential diagnoses include synovial cyst, ganglion, synovial
sarcoma, malignant fibrous histiocytoma and lipoma.
The diagnosis of GCT-TS is rarely aided by the use
of plain radiographs, although, bone erosion or soft tissue
swelling is occasionally observed using this imaging technique
(9). In the present case, plain
radiographs were used to identify tibial erosion (Fig. 2). MRI is an effective and highly
sensitive tool for the diagnosis of GCT-TS and T1- and T2-weighted
imaging (T1WI and T2WI) of tumors, which may present with a
homogeneous low signal intensity, typically demonstrate dense
collagen and hemosiderin-laden macrophages (9,10). MRI
is used to determine the extent of GCT-TS by evaluating the
longitudinal tumor size and the tumor extent around the phalanx
(the degree of circumferential occupation by a tumor around the
phalanx on an axial plane) (11).
The present case demonstrated 360° tumor involvement around the
patellar tendon (Fig. 3C). To the
best of our knowledge, previously reported cases of nodular-type
GCT-TS were not as large as the tumor investigated in the present
report and exhibited less tumor involvement around the patellar
tendon (6,7).
With respect to the differential diagnosis of a soft
tissue mass around the knee joint, an intra-articular ganglion
demonstrates a homogenous high signal intensity on T2WI; and
synovial sarcoma and malignant fibrous histiocytoma exhibit a
non-homogenous appearance on MRI. However, a giant cell tumor
exhibits a combination of homogenous low signal intensity on T1W1
and T2WI (10). Although the
present case exhibited the characteristics of a giant cell tumor on
plain radiographs and MRI, histopathological determination of the
diagnosis was required.
Treatment of nodular-type GCT-TS involves careful
and complete local excision regardless of the site. Although GCT-TS
is a benign tumor, it has a high incidence of recurrence following
resection (~10–20%) (1), thus,
careful observation for recurrence was required in the present
case. Adequate initial local excision reduces the risk of local
recurrence (5) and postoperative
radiotherapy has been proposed as an optional adjuvant therapy
(12).
In conclusion, the present study highlights the
unique features of GCT-TS in a rare case where the tumor extended
around the patellar tendon, and invaded the knee joint and
tibia.
Acknowledgements
The authors would like to thank Dr Toshitaka Maejima
of the Department of Pathology, Shinshu Ueda Medical Center (Ueda,
Japan) for histopathological advice.
References
|
1
|
Weiss SW and Goldblum JR: Benign tumors
and tumor-like lesions of synovial tissues. Enzinger and Weiss’s
Soft Tissue Tumors. 5th edition. Mosby; St Louis, MO: pp. 769–788.
2007
|
|
2
|
Di Grazia S, Succi G, Fragetta F and
Perrotta RE: Giant cell tumor of tendon sheath: study of 64 cases
and review of literature. G Chir. 34:149–152. 2013.
|
|
3
|
Fletcher CD, Krishnan Unni KK and Mertens
F: Giant cell tumour of tendon sheath. World Health Organization
Classification of Tumors, Pathology and Genetics of Tumors of Soft
Tissue and Bone. IARC Press; Lyon: pp. 110–111. 2002
|
|
4
|
Ushijima M, Hashimoto H, Tsuneyoshi M and
Enjoji M: Giant cell tumor of the tendon sheath (nodular
tenosynovitis). A study of 207 cases to compare the large joint
group with the common digit group. Cancer. 57:875–884. 1986.
|
|
5
|
Monaghan H, Salter DM and Al-Nafussi A:
Giant cell tumour of tendon sheath (localised nodular
tenosynovitis): clinicopathological features of 71 cases. J Clin
Pathol. 54:404–407. 2001.
|
|
6
|
Relwani J, Factor D, Khan F and Dutta A:
Giant cell tumour of the patellar tendon sheath - an unusual cause
of anterior knee pain: a case report. Knee. 10:145–148. 2003.
|
|
7
|
Sun C, Sheng W, Yu H and Han J: Giant cell
tumor of the tendon sheath: A rare case in the left knee of a
15-year-old boy. Oncol Lett. 3:718–720. 2012.
|
|
8
|
Karasick D and Karasick S: Giant cell
tumor of tendon sheath: spectrum of radiologic findings. Skeletal
Radiol. 21:219–224. 1992.
|
|
9
|
Rodrigues C, Desai S and Chinoy R: Giant
cell tumor of the tendon sheath: a retrospective study of 28 cases.
J Surg Oncol. 68:100–103. 1998.
|
|
10
|
Jelinek JS, Kransdorf MJ, Shmookler BM,
Aboulafia AA and Malawer MM: Giant cell tumor of the tendon sheath:
MR findings in nine cases. AJR Am J Roentgenol. 162:919–922.
1994.
|
|
11
|
Kitagawa Y, Ito H, Amano Y, Sawaizumi T
and Takeuchi T: MR imaging for preoperative diagnosis and
assessment of local tumor extent on localized giant cell tumor of
tendon sheath. Skeletal Radiol. 32:633–638. 2003.
|
|
12
|
Kotwal PP, Gupta V and Malhotra R:
Giant-cell tumour of the tendon sheath. Is radiotherapy indicated
to prevent recurrence after surgery? J Bone Joint Surg Br.
82:571–573. 2000.
|