Introduction
Bone marrow metastasis from solid tumors is usually
accepted as not only incurable, but as fatal. Lung, breast and
prostate malignancies in adults, and neuroblastoma and
rhabdomyosarcoma in children are the most common non-hematological
malignancies to frequently involve the bone marrow (1). However, almost all types of malignancy
can metastasize to the bone marrow and these are occasionally
reported (1–3). The frequency of detection depends on
the stage of the disease and the other sites of the metastases.
Colon cancer is a relatively rare malignancy that
involves the bone marrow (2,4), and
to the best of our knowledge, there have been no studies in the
literature reporting only bone marrow metastasis of colon cancer as
the first presentation of relapse. The present study reports the
case of a patient with bone marrow metastasis from colon cancer as
the site of recurrence, presnting with severe thrombocytopenia and
fatal intracranial hemorrhage. Written informed consent was
obtained from the family of the patient.
Case report
A 74-year-old female patient visited the Department
of Hematology-Oncology, Dankook University of Medicine (Cheonan,
Korea) for the evaluation and treatment of thrombocytopenia and an
increased bleeding tendency. The patient had previously undergone a
right hemicolectomy with ileocolostomy due to colon cancer three
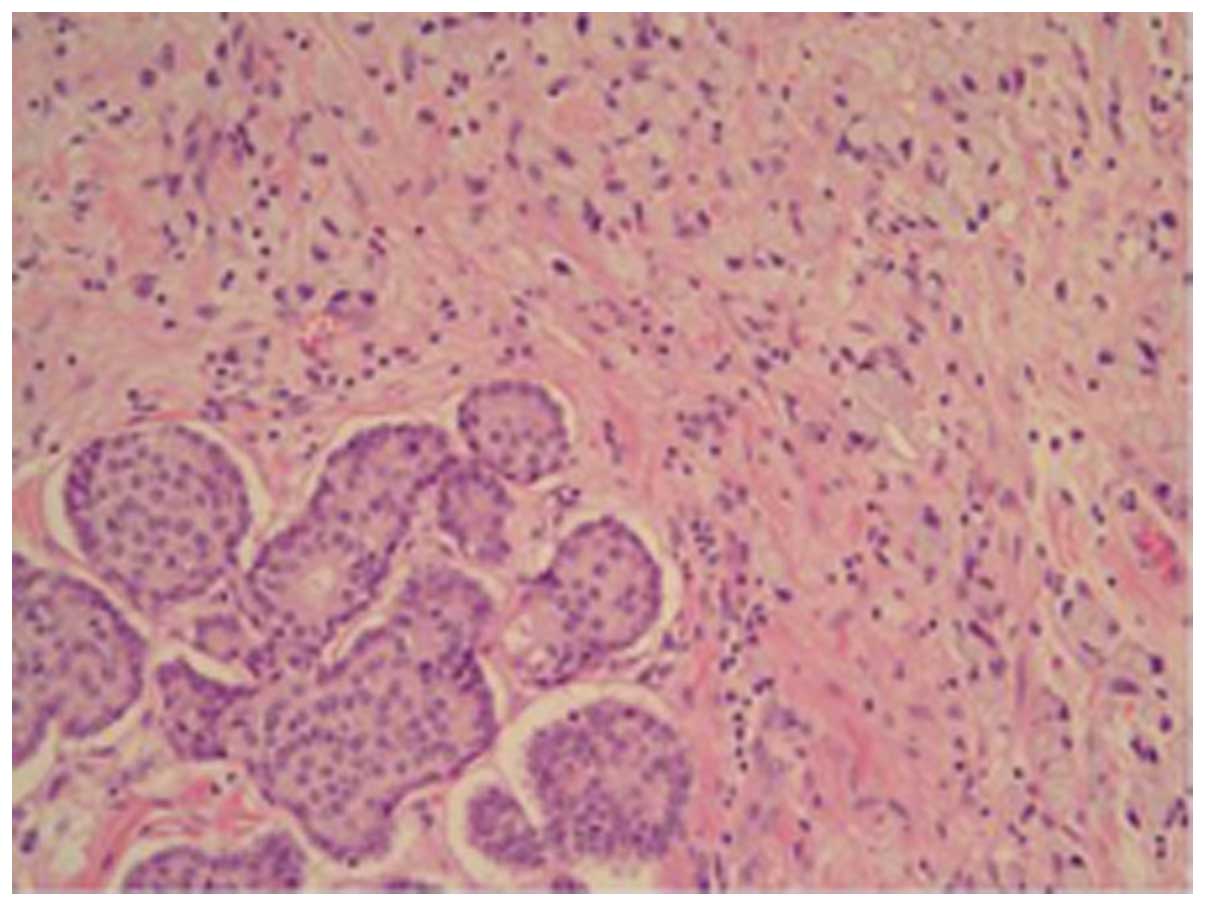
years previously. At that time, the obtained surgical specimen was
diagnosed as adenocarcinoma, with signet ring cell features
(Fig. 1), and the surgical staging
was pT3N2M0, stage IIIc. The patient received adjuvant chemotherapy
with oxaliplatin (85 mg/m2, day 1), leucovorin (200
mg/m2, days 1 and 2) and 5-fluorouracil (400
mg/m2 i.v. bolus and subsequently 600 mg/m2
i.v. continuously for 22 h, days 1–2) every two weeks for six
months. Subsequent to this, the patient was followed up regularly
and there was no evidence of disease recurrence until the last
abdominopelvic computed tomography (CT) scans, 50 days prior to the
current admission.
The patient was treated by the traditional herbal
medicine clinic (Chinese Medicine Clinic, Oriental Hospital of
Daejeon University, Cheonan, Korea) for approximately three weeks
due to back pain that occurred from a fall. The patient was
prescribed herbal medicine and treated with acupuncture on the
back. One day prior to visiting Dankook University of Medicine, the
patient suddenly developed a headache, dizziness, vomiting and
severe thrombocytopenia, with a count of 5,000/μl, decreased from
the count of 111,000/μl measured by the initial laboratory test at
the clinic. The patient was therefore transferred to Dankook
University of Medicine for a transfusion, and for the evaluation
and treatment of the thrombocytopenia.
The initial laboratory data recorded in Dankook
University of Medicine determined a white blood cell count of
5,910/μl (normal range, 4,000–10,000/μl), a hemoglobin level of 6.7
g/dl (normal range, 12–16 g/dl), a platelet count of 4,000/μl
(normal range, 130,000–400,000/μl), an aspartate
transaminase-alanine transaminase ratio of 45/8 IU/l (normal range,
4–37/4–41 IU/l), a total bilirubin level of 1.43mg/dl (normal
range, 0.2–1.2 mg/dl), an alkaline phosphatase level of 262 IU/l
(normal range, 35–104 IU/l) and a protein/albumin ratio of 5.9/3.7
g/dl (normal range, 6.4–8.3/3.4–4.8 g/dl). The prothrombin time
(international normalized ratio) was 18.2 sec (1.50; normal range,
9–13 sec/0.7–1.2 international normalized ratio) and the partial
thromboplastin time was 36.8 sec (normal, 25–37 sec). At the time
of admission, CT scans of the brain revealed acute subdural
hemorrhage on each fronto-parieto-temporal area. The patient was
clinically diagnosed with drug-induced thrombocytopenia owing to
herbal medicine and was initially transfused with packed red blood
cells and platelet concentrates. Hematoma removal and decompression
surgery was planned for after an increase in the platelet count,
however, the thrombocytopenia did not improve despite the patient
discontinuing the suspected herbal medicine and even though a
repeated transfusion of platelet concentrates was performed and
treatment with systemic steroid was administered. A bone marrow
aspiration and biopsy were performed, and the patient was also
injected with human immunoglobulin intravenously, however, the bone
marrow aspirate showed no adequate marrow particles or cellular
elements. Even though all treatment options were attempted, the
platelet count had decreased to 1,000/μl, the patient’s mental
status was worsening and there was an increasing amount of
hemorrhage on follow-up CT scans. The Department of Neurosurgery
therefore decided that an emergency procedure was necessary
regardless of the risk of extreme bleeding, and the probable high
morbidity and mortality. However, the patient’s family did not
consent to the surgery, and following a lack of response to the
medical treatment, the patient succumbed 10 days after
admission.
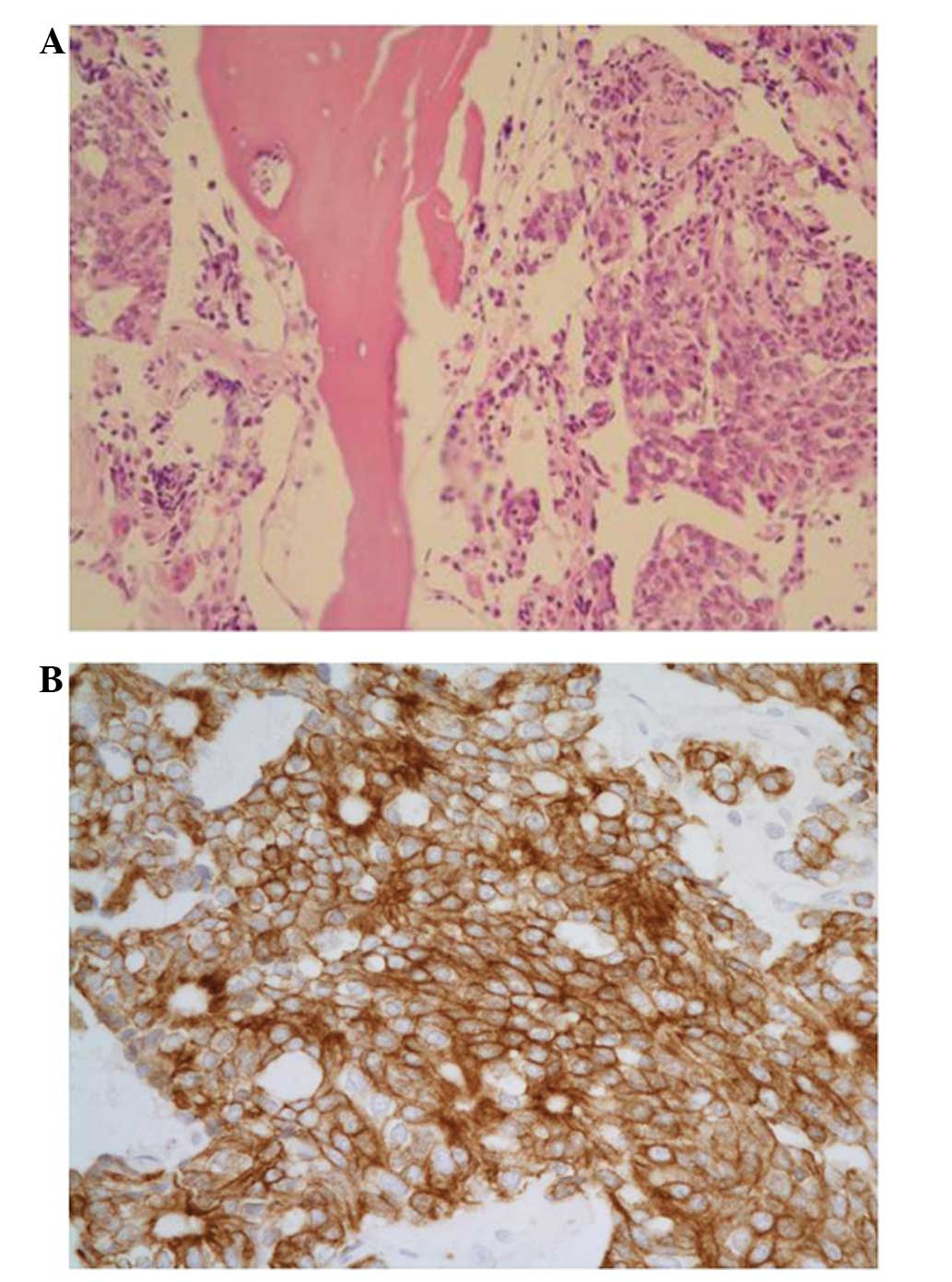
The final result of the bone marrow biopsy was
reported several days later. The overall cellularity was 70–80%,
which was hypercellular for the patient’s age, and there was a
diffuse infiltration of tumor cells that were negative for
leukocyte common antigen and strongly positive for pan-cytokeratin
(Fig. 2). The tumor cells
infiltrating the bone marrow had the same morphological and
immunohistochemical characteristics as the initial colon
adenocarcinoma. The patient was finally diagnosed with bone marrow
metastasis of colon cancer as an initial site of recurrence.
Discussion
To the best of our knowledge, the present study is
the first to report the bone marrow metastasis of colon cancer as
the initial site of recurrence. The clinical course of this case
displayed rapid progression with a fatal intracranial hemorrhage
associated with severe thrombocytopenia. The patient eventually
succumbed despite medical supportive care. The case showed three
notable features, namely, the bone marrow metastasis of colon
cancer as the first site of recurrence, no other metastatic sites,
including skeletal metastasis, and an initial misdiagnosis of
drug-induced thrombocytopenia.
Bone marrow metastasis of solid tumors generally
develops at the late stage of disease (2) and is accompanied by skeletal
metastasis in the majority of cases (1,2). In
the mouse model, the route of injection and the number of cancer
cells appear to have an effect on the colonization of the bone
marrow by the tumor (5). There is
evidence suggesting that bone marrow involvement may be a requisite
for bone metastasis in this experimental model. Human cases are
similar to the animal model, as the solid tumors that frequently
involve the bone marrow, for example, lung, breast and prostate
cancers, also commonly metastasize to the skeletal system. However,
in the present case, the bone marrow was the only site of
metastasis and there was no evidence of systemic metastases,
including bone metastasis, on abdominopelvic CT scans and simple
X-ray. This type of unusual recurrence of the colon cancer was not
suspected initially and therefore, this was first cause of delaying
the diagnosis of the patient.
Numerous patients visit traditional herbal medicine
clinics (Chinese Medicine Clinics) in Korea, particularly those
searching for remedies for musculoskeletal problems, as well as
general medical conditions. A number of individuals are treated
with acupuncture and prescribed herbal medicine with scientifically
indefinite ingredients. Drug-induced thrombocytopenia induced by
herbal remedies is not an uncommon occurrence in Korea and it
represents a significant clinical problem for hematologists.
Hematologists should always be aware of whether patients have been
taking herbal medicine when they perform the initial assessment of
a patient with thrombocytopenia. Drug-induced thrombocytopenia
typically induces the sudden onset of thrombocytopenia, which is
often severe, and can cause major bleeding and mortality (6,7). Nadir
platelet counts are often 20,000/μl. The recovery of
thrombocytopenia begins within 1–2 days of the drug being
discontinued and recovery is usually complete within a week. In the
present study, the patient had a history of taking herbal medicine
and exhibited the aforementioned abrupt decrease in platelet count.
Therefore, the initial condition was diagnosed as drug-induced
thrombocytopenia. This was second cause of the delayed diagnosis of
the patient.
There were certain problems with the diagnosis of
the present patient, particularly with respect to the bone marrow
metastasis of colon cancer, without skeletal metastasis, as the
first site of recurrence. Physicians should always suspect the bone
marrow involvement of solid tumors in cancer patients with
pancytopenia, even when there is no evidence of systemic
metastases, including bone metastasis.
In conclusion, for pancytopenia in cancer patients,
there should be no delay in performing a bone marrow examination to
identify the fatal condition of the present case and manage it
properly, although there are other suspected causes.
References
|
1
|
Anner RM and Drewinko B: Frequency and
significance of bone marrow involvement by metastatic solid tumors.
Cancer. 39:1337–1344. 1977.
|
|
2
|
Jonsson U and Rundles RW: Tumor metastases
in bone marrow. Blood. 6:16–25. 1951.
|
|
3
|
Papac RJ: Bone marrow metastases. A
review. Cancer. 74:2403–2413. 1994.
|
|
4
|
Wong KF, Chan JK and Ma SK: Solid tumour
with initial presentation in the bone marrow - a clinicopathologic
study of 25 adult cases. Hematol Oncol. 11:35–42. 1993.
|
|
5
|
Arguello F, Baggs RB and Frantz CN: A
murine model of experimental metastasis to bone and bone marrow.
Cancer Res. 48:6876–6881. 1988.
|
|
6
|
George JN and Aster RH: Drug-induced
thrombocytopenia: pathogenesis, evaluation, and management.
Hematology Am Soc Hematol Educ Program. 153–158. 2009.
|
|
7
|
Aster RH and Bougie DW: Drug-induced
immune thrombocytopenia. N Engl J Med. 357:580–587. 2007.
|