Introduction
Malignant melanoma is a skin cancer that is caused
by the malignant transformation of melanocytes. The disease rarely
occurs in the mucosal tissues and uvea. Malignant melanoma can be
successfully treated if it is detected in the early stages of
development. Surgery is the standard treatment for early stage
melanoma. In addition, interferon-α has been approved for adjuvant
treatment following excision in disease-free patients at high risk
of recurrence. However, the prognosis associated with
advanced-stage malignant melanoma is poor; the disease accounts for
~4% of all skin cancers, but results in 80% of skin
cancer-associated mortality (1,2). In
total, 75% of thyroid cancers are papilliary thyroid cancer, which
is associated with a good prognosis (3). Papillary thyroid cancer may result
from exposure to radiation. Surgery is the standard treatment for
papillary thyroid cancer. Approximately four-six weeks following
surgical removal of the thyroid, radioiodine therapy may be
administered to detect and remove any metastasis and residual tumor
tissue in the thyroid. Second primary tumors may develop in
patients with malignant melanoma. Previous studies have reported
associations between malignant melanoma and a wide variety of
malignancies including second primary melanoma, non-melanoma skin
cancer, central nervous system tumors, Hodgkin’s lymphoma,
non-Hodgkin’s lymphoma, leukemia, breast carcinoma, ovarian
carcinoma and papillary thyroid carcinoma (4). However, papillary thyroid carcinoma
rarely co-occurs with malignant melanoma. The present study reports
the case of a rare co-occurrence of malignant melanoma and
papillary thyroid carcinoma, which were treated simultaneously.
Written informed consent was obtained from the patient.
Case report
Diagnosis
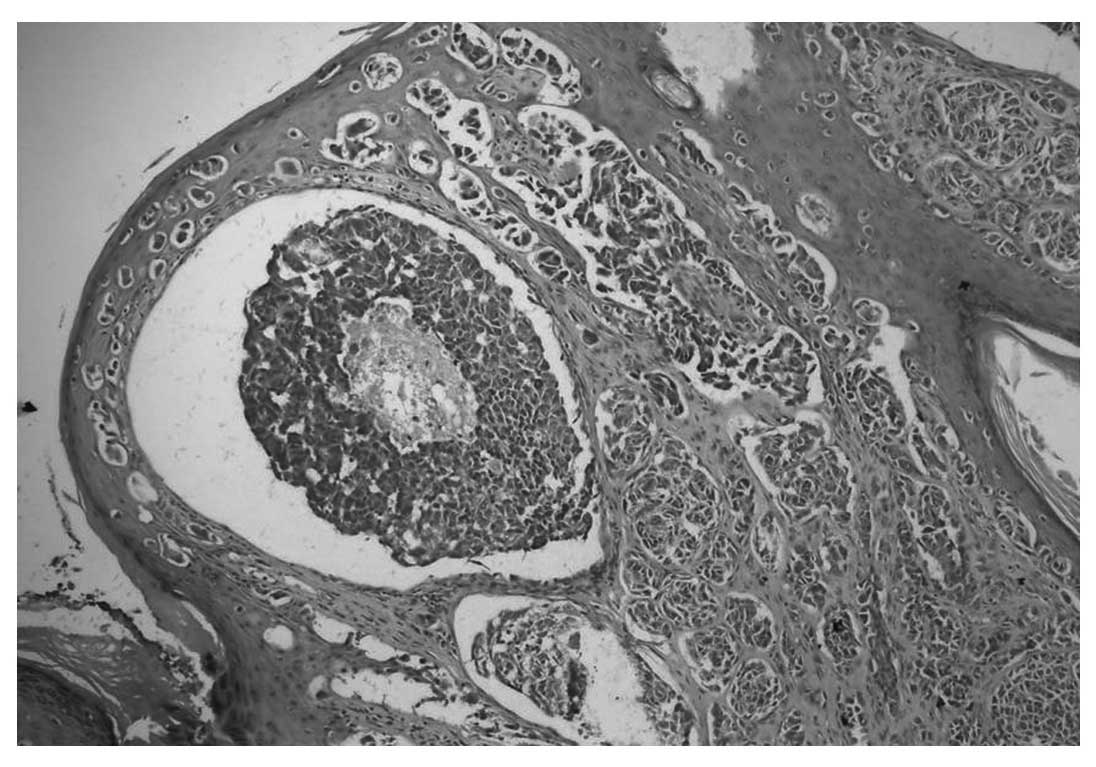
A 37-year-old male patient presented to the Gulhane
Military Medical Academy Haydarpasa Training Hospital (Istanbul,
Turkey) with a one-year history of a growing nevus located in the
right retroauricular region that had been undergoing changes in
color. An excisional biopsy was performed on the suspicious skin
lesion. Pathological examination suggested that the lesion was a
nodular-type malignant melanoma, Clark level IV and with a Breslow
thickness of 3 mm (Fig. 1). Neck
ultrasonography revealed two lymphadenopathies in the right jugular
chain, the largest measuring 11 mm. Thoracic and abdominal computed
tomography and bone scintigraphy did not reveal the presence of
metastasis. Lymphoscintigraphy of the right neck was performed
using Tc99m. The procedure revealed uptake in two foci located in
the right retroauricular region and the right upper cervical lymph
nodes. The patient then underwent extensive re-excision and
sentinel lymph node biopsy. Metastasis of the malignant melanoma
was detected in one of the sentinel lymph nodes.
Treatment
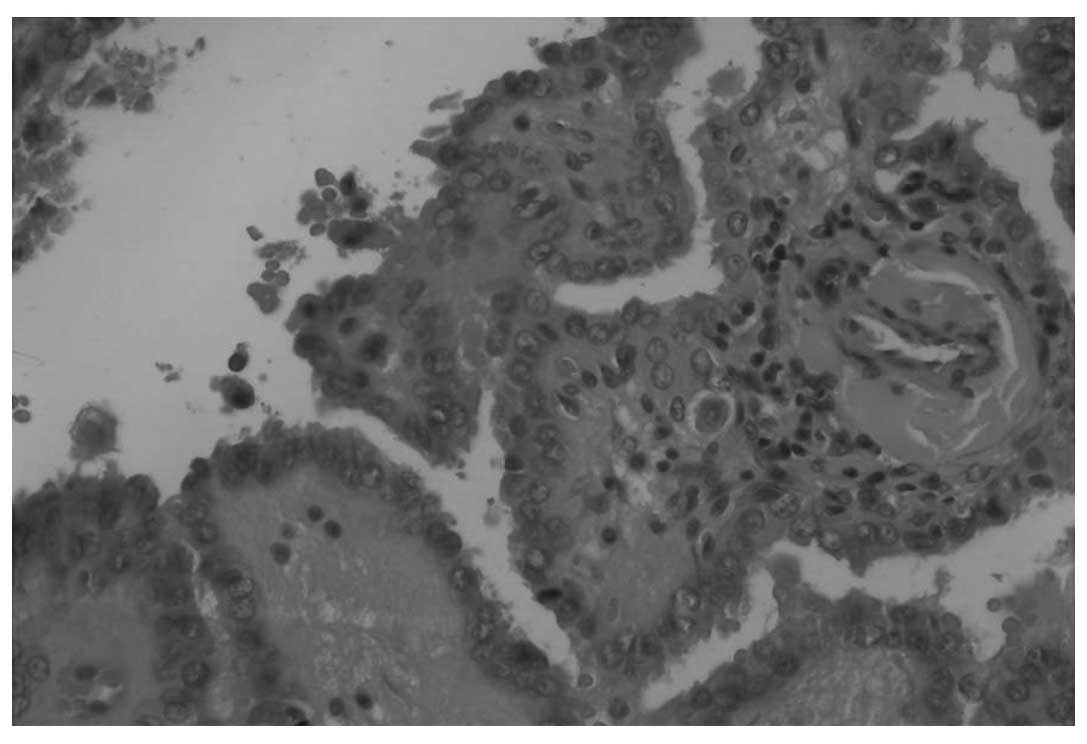
The patient subsequently underwent modified radical
neck dissection and pathological examination revealed the presence
of papilliary thyroid carcinoma metastasis in four out of 38 lymph
nodes and also revealed reactive hyperplasia in the remaining 34
lymph nodes. The patient subsequently underwent total thyroidectomy
and the pathological examination revealed a classical variant of
papillary thyroid carcinoma (Fig.
2). Imaging examinations did not reveal distant organ
metastasis associated with either primary tumor. The patient was
initially intravenously administered with high-dose interferon
therapy (20 MU/m2) five days a week, for four weeks, to
treat the malignant melanoma. In order to treat the papillary
thyroid carcinoma, the patient was administered with low-dose (5
mci) radioactive iodine therapy in the second week of the high-dose
interferon therapy. The high-dose interferon therapy was followed
by moderate-dose interferon therapy (10 MU/m2), which
was intravenously administered three days a week for 48 weeks. The
patient was also administered with high-dose radioactive iodine
(150 mci) therapy in the eighth week of the moderate-dose
interferon therapy.
The two primary tumors observed in the present
patient were successfully treated. No serious side-effects were
observed during therapy, with the exception of a fever caused by
the high-dose interferon therapy. The patient continues to be
followed up by the Gulhane Military Medical Academy Haydarpasa
Training Hospital and is disease-free at present. Moderate-dose
interferon therapy and thyroid hormone replacement therapy continue
to be administered.
Discussion
Advanced-stage malignant melanoma is associated with
a poor prognosis. However, the therapeutic agents identified in
previous years have provided significant improvements in patient
survival (2). Papillary thyroid
carcinoma is the most common type of thyroid cancer, and is
associated with a good prognosis (3). Second primary tumors may occur in
patients with malignant melanoma. In a study by Bhatia et
al, 37 out of 585 patients (6.3%) with malignant melanoma were
found to possess a second primary tumor. Of these patients,23 had
other skin cancers and the remaining patients had lymphoma and
breast, bladder, lung, prostate and cervical cancer lesions
(4).
Papillary thyroid carcinoma rarely occurs as a
second primary tumor in patients with malignant melanoma. Kim et
al reported a case of malignant melanoma in which concurrent
papillary thyroid carcinoma manifested with hypothyroidism
(5). Goggins et al reviewed
73,274 patients with malignant melanoma who were diagnosed between
1973 and 2000, and found that there was a 2.17-fold increase in the
risk of developing thyroid cancer as the concurrent second primary
tumor (6). Previous studies have
reported a higher frequency of BRAF mutation in patients with
malignant melanoma and thyroid cancer compared with patients
suffering from other types of cancer (7–10). In
the study by Goggins et al, a high frequency of BRAF
mutation in the patients with malignant melanoma and thyroid cancer
was suggested to be the cause of the co-occurrence of the two
diseases (6).
In the present study, a radical neck dissection was
performed following a sentinel lymph node biopsy that detected the
presence of metastases from malignant melanoma, which also resulted
in the detection of metastasis from papillary thyroid carcinoma in
the four excised lymph nodes. Therefore, the present patient was
diagnosed with papillary thyroid carcinoma as a second primary
tumor and the two primary tumors were successfully treated.
It should be considered that patients with malignant
melanoma may also possess concurrent papillary thyroid carcinoma as
the second primary tumor, and the lymph nodes removed during
radical neck dissection must be carefully examined from this
perspective. Furthermore, it should be remembered that the two
tumors can be treated simultaneously and that the treatment of
either tumor should not be delayed.
References
|
1
|
Balch CM, Soong SJ, Gershenwald JE, et al:
Prognostic factors analysis of 17,600 melanoma patients: validation
of the American Joint Committe on Cancer melanoma staging system. J
Clin Oncol. 19:3622–3634. 2001.PubMed/NCBI
|
|
2
|
Miller AJ and Mihm MC Jr: Melanoma. N Engl
J Med. 355:51–65. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Weber T, Schilling T and Büchler MW:
Thyroid carcinoma. Curr Opin Oncol. 18:30–35. 2006.
|
|
4
|
Bhatia S, Estrada-Batres L, Maryon T, et
al: Second primary tumors in patients with cutaneous malignant
melanoma. Cancer. 86:2014–2020. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kim CY, Lee SH and Oh CW: Cutaneous
malignant melanoma associated with papillary thyroid cancer. Ann
Dermatol. 22:370–372. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Goggins W, Daniels GH and Tsao H:
Elevation of thyroid cancer risk among cutaneous melanoma
survivors. Int J Cancer. 118:185–188. 2006. View Article : Google Scholar
|
|
7
|
Davies H, Bignell GR, Cox C, et al:
Mutations of the BRAF gene in human cancer. Nature. 417:949–954.
2002. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Kimura ET, Nikiforova MN, Zhu Z, et al:
High prevalence of BRAF mutations in thyroid cancer: genetic
evidence for constitutive activation of the RET/PTC-RAS-BRAF
signaling pathway in papillary thyroid carcinoma. Cancer Res.
63:1454–1457. 2003.PubMed/NCBI
|
|
9
|
Cohen Y, Xing M, Mambo E, et al: RAF
mutation in papillary thyroid carcinoma. J Natl Cancer Inst.
95:625–627. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Xu X, Quiros RM, Gattuso P, et al: High
prevalence of BRAF gene mutation in papillary thyroid carcinomas
and thyroid tumor cell lines. Cancer Res. 63:4561–4567.
2003.PubMed/NCBI
|