Introduction
Cervical cancer has been established as the second
most common cancer among females worldwide (1,2).
Cervical cancer is a serious heath problem and the majority of
cases occur in developing countries (3), as no effective screening procedures
are available (4). Recently, with
the improvement of cervical cancer screening, the worldwide
incidence and mortality of cervical cancer has decreased (5). However, the incidence of cervical
cancer in young individuals worldwide has markedly increased and
exhibits a poor prognosis (6,7).
Patients with localized disease may be cured after definitive
cancer therapy, and previous studies have indicated that surgery or
radiation therapy provide an equivalent outcome (8). Patients that present with regional or
distant disease are at a greater risk of mortality (9). Common metastases of cervical cancer
include local extension and lymph node and pulmonary metastasis.
However, metastasis to the small intestine is rare and, to the best
of our knowledge, it has not been reported in the literature in the
previous several decades. Small intestine metastasis from primary
tumors located elsewhere in the body easily results in a missed or
incorrect diagnosis, as the metastasis is frequently regarded as
acute abdomen, with the main symptom of abdominal pain (10,11).
The present study presents and discusses a case of cervical cancer
with symptomatic small intestine metastasis.
Case Report
A 46-year-old female was admitted to the
gastroenterology department of the Zhongnan Hospital of Wuhan
University (Wuhan, China) due to acute abdominal pain. Abdominal
examination revealed mild tenderness without rebound tenderness,
with decreased peristalsis, detected by auscultation. In the
initial laboratory tests, the serum carcinoembryonic antigen level
was 5.46 ng/ml (normal range, 0–7.2 ng/ml); ferritin, 370.62 ng/ml
(normal range, 12–150 ng/ml); squamous cell carcinoma antigen, 9.9
ng/ml (normal range, 0–1.5 ng/ml) and sodium ion, 133.3 mmol/l
(normal range, 135–145 mmol/l). The results of a routine analysis
of the blood [white blood cell count, 4.0×109/l (normal
range, 4.0–10.0×109/l); red blood cell count,
3.6×1012/l (normal range, 3.5–5.5×1012/l);
hemoglobin, 114 g/l (normal range, 110–150 g/l); platelet count,
125×109/l, (normal range, 100–300×109/l);
neutrophil percentage, 62% (normal range, 50–70%); lymphocyte
percentage, 25% (normal range, 20–40%); monocyte percentage, 5.2%
(normal range, 3–8%); acidophilic cell percentage, 0.7% (normal
range, 0.5–5%); and basophilic cell percentage, 0.1% (normal rane,
0–1%)], urinalysis, a liver function test [Aspertate
aminotransferase (AST), 28 U/l (normal range, 0–46 U/l); Alanine
aminotransferase (ALT), 35 U/l (normal range, 0–46 U/l); AST/ALT
ratio, 0.81 (normal range, 0.2–2.0); total bilirubin, 17.7 μmol/l
(normal range, 0–25 μmol/l); direct bilirubin, 6.8 μmol/l (normal
range, 0–7 μmol/l); indirect bilirubin, 10.9 μmol/l (normal range,
1.5–18 μmol/l); total protein, 65 g/l (normal range, 60–80 g/l);
albumin, 38 g/l (35–55 g/l); globulin, 24 g/l (normal range, 20–30
g/l); albumin/globulin ratio, 1.58 (normal range, 1.5–2.5);
glutamine, 51 U/l (normal range, 5–55 U/l); alkaline phosphatase,
132 U/l (normal range, 35–134 U/l); and total bile acids, 6.4
μmol/l (normal range, 0–15 μmol/l)] and chest films all normal. On
observation, the abdominal X-ray revealed multiple liquid-gas
surfaces, suggesting intestinal obstruction (Fig. 1). In addition, the patient had been
diagnosed with stage IIB cervical cancer in 2010 and treated by
definitive chemoradiotherapy consisting of whole pelvic external
beam radiotherapy of 50 Gy in 25 fractions, with center shielding
and concomitant high-dose rate intracavitary brachytherapy with
192-iridium remote after loading system for 42 Gy to the
intersection of the vaginal vault. The concurrent chemotherapy
regimen was cisplatin, 40 mg/m2/week. The patient was
subsequently diagnosed with lower intestinal obstruction and
cervical cancer following chemoradiotherapy.
The mechanical bowel obstruction was proposed to
have been caused by an advanced complication following pelvic
radiotherapy, or a small intestine primary or metastatic tumor. The
patient was provided with anti-inflammatory treatment, gastric tube
drainage, acid suppression, fluid infusion and nutritional support.
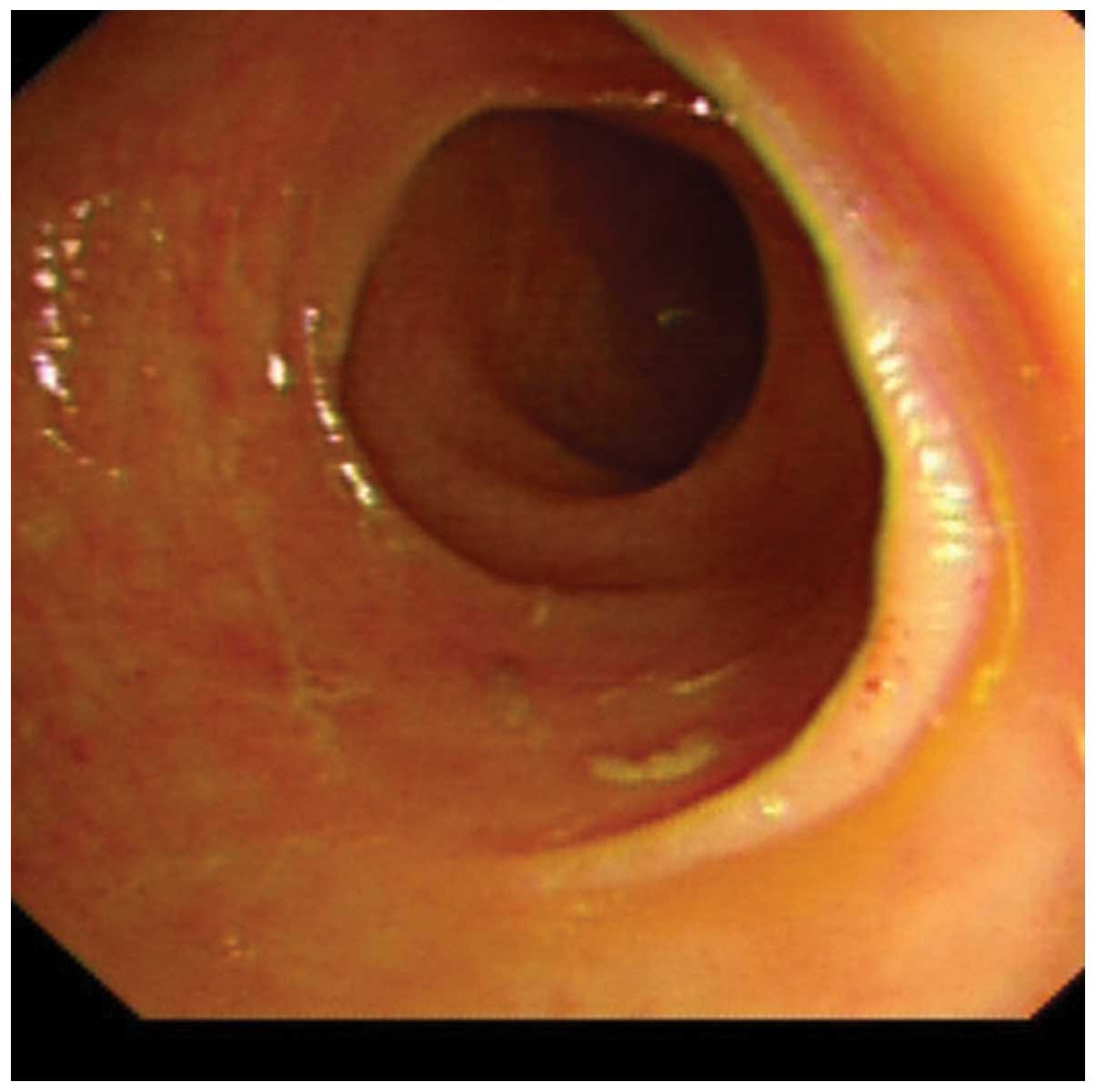
Concomitantly, colonoscopy revealed that the intestinal mucosa was
smooth without any ulcer or lump (Fig.
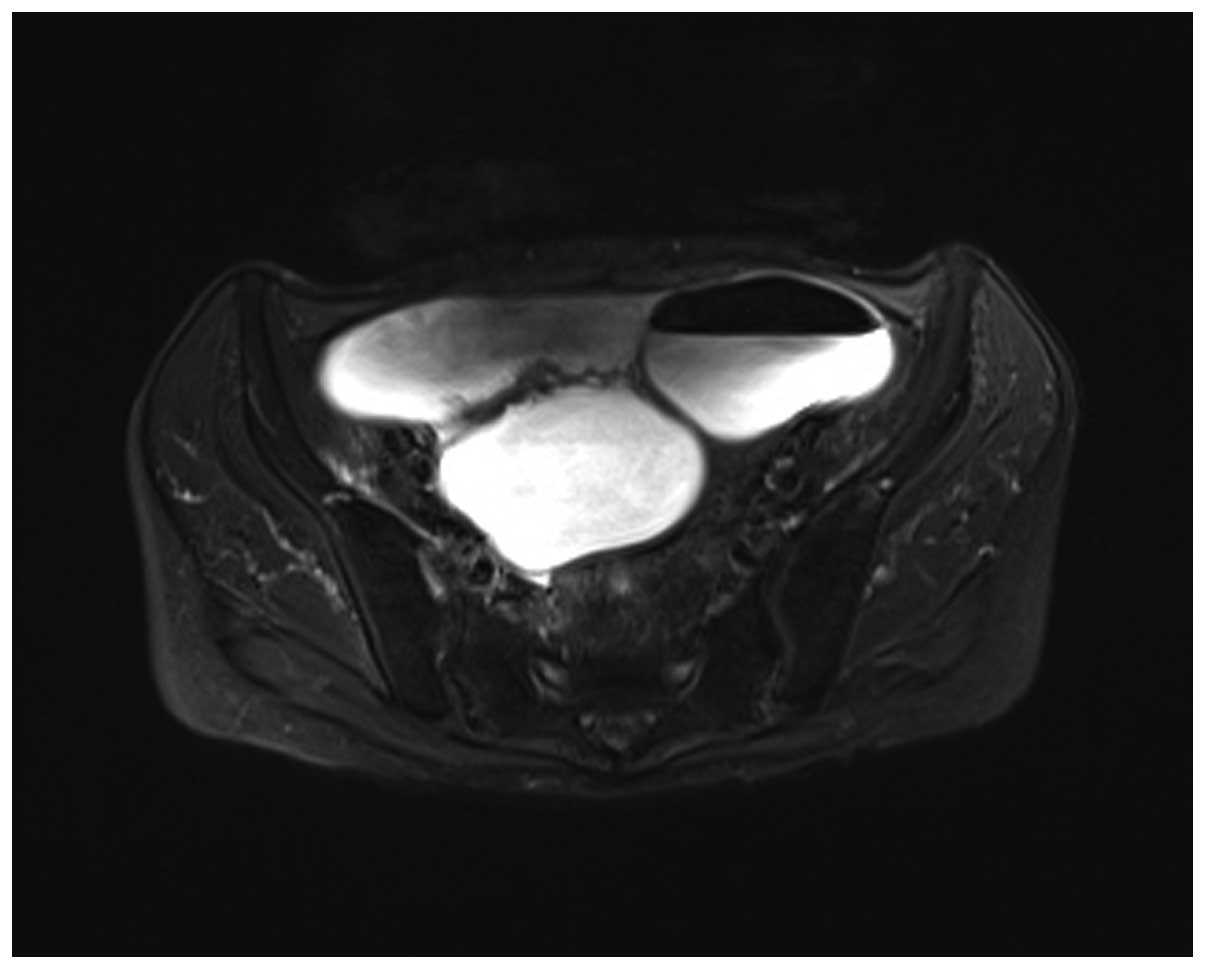
2). Magnetic resonance imaging of the pelvic cavity showed the
change in cervical cancer following chemoradiotherapy, pelvic
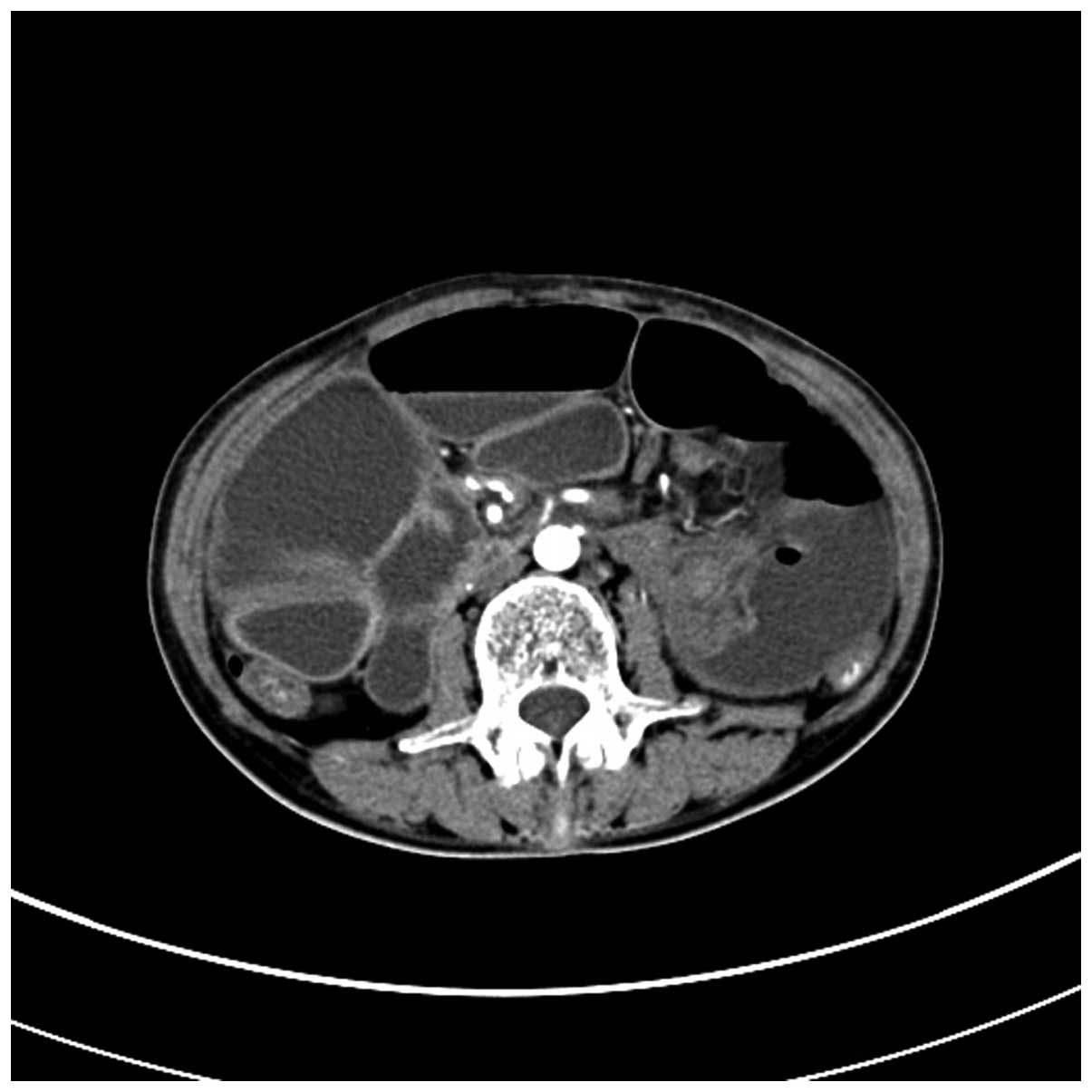
effusion and lower intestinal obstruction (Fig. 3). A computed tomography (CT) scan of
the abdomen revealed cervical cancer following chemoradiotherapy
and lower intestinal obstruction (Fig.
4). As the effect of conservative treatment was not
satisfactory, with gradually worsening abdominal pain, the patient
was transferred to the department of general surgery. Under general
anesthesia, laparotomy was performed, which revealed the
significant expansion of the small intestine, little ascites,
multiple pelvic nodules, wide small mesenteric lymph node
enlargement and a mass that was approximately 30.0 cm in size,
which originated from the ileocecal junction and caused the
complete occlusion of the intestine.
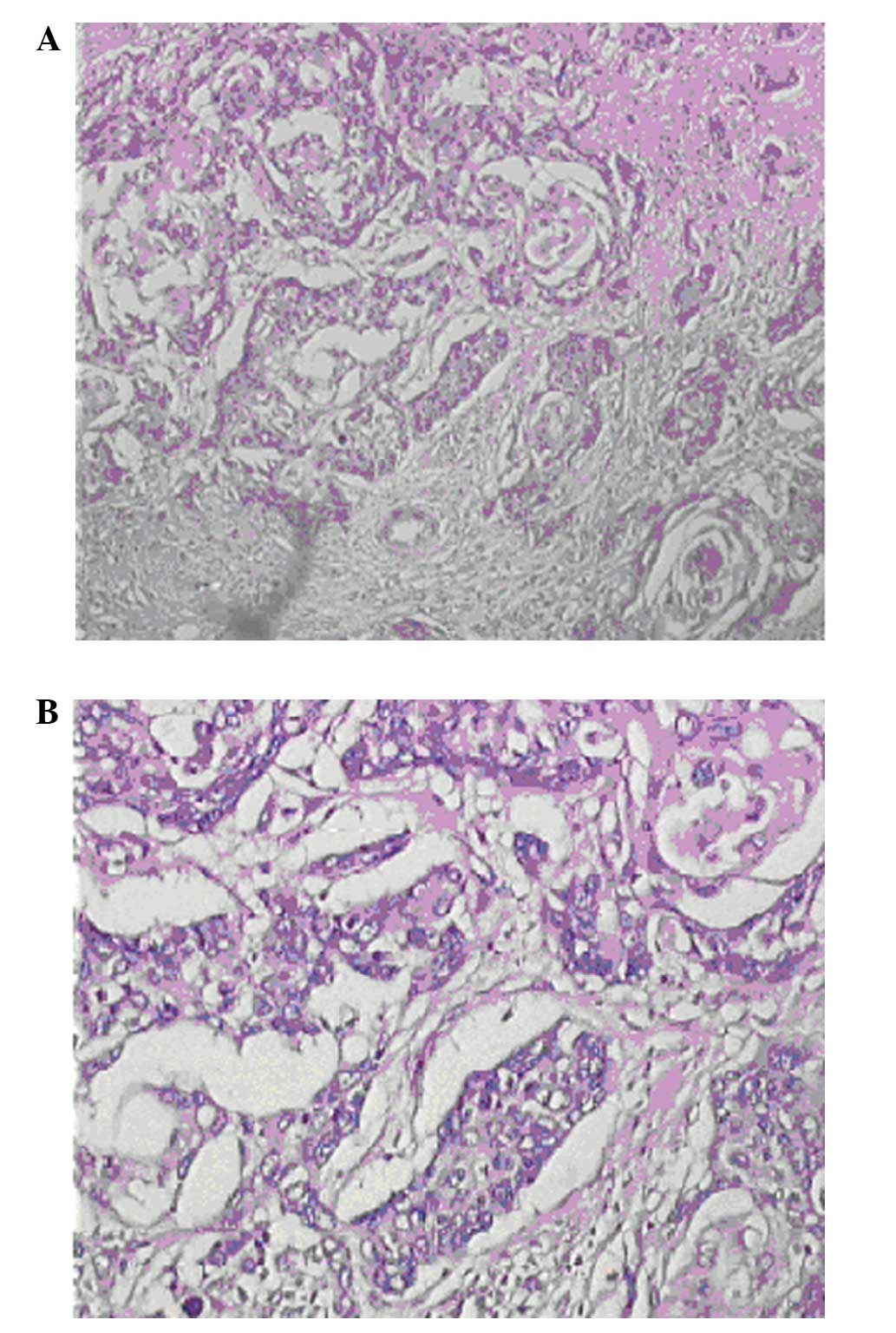
The resection of the small intestinal tumors and
ileostomy was immediately performed. A pathological diagnosis of
squamous carcinoma was determined, and cancer tissue was limited to
the outer muscular layer and serosa (Fig. 5). A final diagnosis of cervical
cancer with small intestine metastases was determined.
Postoperatively, the ileus symptoms improved and the general
condition of the patient also improved. The patient was treated
with four cycles of a docetaxel-cisplatin combination chemotherapy
regimen (day 1, 75 mg/m2 docetaxel; days 1–3, 25
mg/m2 cisplatin, every 21 days). One month following
chemotherapy, the patient returned to the hospital for regular
follow-up appointments, which were subsequently attended every
three months for two years.
Written, informed consent was obtained from the
patient for the publication of the present study and the related
images.
Discussion
Cervical cancer is the second most common cancer in
women, being second only to breast cancer (12). The traditional treatment is radical
surgery, with radiotherapy and chemotherapy predominantly used for
the treatment of advanced or recurrent patients. In 2001, the
National Comprehensive Cancer Network recommended cisplatin-based
concurrent chemoradiotherapy as the standard treatment for advanced
and high-risk early cervical cancer. Over the past decade,
treatment with concurrent chemoradiotherapy has evidently prolonged
the survival of patients with cervical carcinoma (13–15).
However, with the improvement of survival, the patients are also at
increased risk of recurrence and metastases.
When cervical carcinoma metastasizes, it usually
does so via local or lymphatic dissemination. Hematogenous
dissemination occurs less frequently, can spread to almost all
organs and usually affects the lungs initially, followed by the
bones and paraaortic, intraperitoneal and supraclavicular lymph
nodes (16). Cervical cancer
metastasis to the small intestine is rare, and easily misdiagnosed
as it is frequently regarded as acute abdomen. According to the
main diagnosis standard of metastatic small intestinal tumors
(17), it must first be clear where
the primary tumors are located. Secondly, the patient presents with
serious clinical complications, including perforation, obstruction
or hemorrhage. Thirdly, the tumor must be histopathologically
confirmed and, finally, it must arise neither from direct
infiltration nor abdominal metastasis. In the present case,
combined with the histopathological characteristics of the patient
and the history of cervical squamous cell carcinoma, the patient
was finally diagnosed with squamous cell carcinoma with metastasis
to the small intestine.
It is generally considered that small intestine
metastasis does not easily occur, due to the intensive lymphoid
tissue in intestinal wall, which can produce immunoglobulin to
enhance immunity (18). It has been
reported that small intestine metastasis occurs in approximately
4–10.6% of cancer cases (19). The
stomach, colon and ovary are common primary tumor sites (20). Small intestinal tumors are likely to
present with intussusception and intestinal obstruction with bowel
stricture or expansion, and thus, surgeons must investigate the
possibility of bumps close to the lesions. As metastasis from
cervical cancer is considered unlikely, and the lesions are often
considered to be advanced symptoms or side-effects of chemotherapy,
the metastases are difficult to identify. When patients present
with abdominal symptoms, including abdominal pain, nausea,
vomiting, anemia and weight loss, or CT scans depict short
segmental bowel-wall thickening or a polypoid mass in the small
intestine in combination with regional lymphadenopathy,
perforation, or intussusception, the gastrointestinal tract of the
patient must be meticulously examined to enable early detection and
treatment. At the present time, comparison between positron
emission tomography-CT, abdominal contrast-enhanced CT and
endoscopy is the most effective method for determining digestive
tract metastasis (21). In the
current study, the patient’s condition deteriorated following
chemotherapy, and this was hypothesized to be due to small
intestine metastasis.
The present case indicates that if cervical cancer
patients present with small intestine obstruction, small intestine
metastasis must be considered in the differential diagnosis of the
condition as acute abdomen.
Acknowledgements
This study was supported by the Natural Science
Foundation of Hubei Province, China (grant no. 303132043).
References
|
1
|
Ferlay J, Bray F, Pisani P and Parkin DM:
GLOBOCAN 2002: Cancer incidence, mortality and prevalence
worldwide. IARC CancerBase No. 5, version 2.0. IARC Press; Lyon,
France: 2004
|
|
2
|
Ferlay J, Shin HR, Bray F, Forman D,
Mathers C and Parkin DM: Estimates of worldwide burden of cancer in
2008: GLOBOCAN 2008. Int J Cancer. 127:2893–2917. 2010. View Article : Google Scholar
|
|
3
|
Jemal A, Bray F, Center MM, Ferlay J, Ward
E and Forman D: Global cancer statistics. CA Cancer J Clin.
61:69–90. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Waggoner SE: Cervical cancer. Lancet.
361:2217–2225. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Vizcaino AP, Moreno V, Bosch FX, Muñoz N,
Barros-Dios XM, et al: International trends in incidence of
cervical cancer: II. Squamous-cell carcinoma. Int J Cancer.
86:429–435. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Bray F, Loos AH, McCarron P, Weiderpass E,
Arbyn M, et al: Trends in cervical squamous cell carcinoma
incidence in 13 European countries: changing risk and the effects
of screening. Cancer Epidemiol Biomarkers Prev. 14:77–86. 2005.
|
|
7
|
Lau HY, Juang CM, Chen YJ, Twu NF, Yen MS
and Chao KC: Aggressive characteristics of cervical cancer in young
women in Taiwan. Int J Gynecol Obstet. 107:220–223. 2009.
View Article : Google Scholar
|
|
8
|
Rasool N and Rose PG: Fertility-preserving
surgical procedures for patients with gynecologic malignancies.
Clin Obstet Gynecol. 53:804–814. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Macdonald OK, Chen J, Dodson M, Lee CM and
Gaffney DK: Prognostic significance of histology and positive lymph
node involvement following radical hysterectomy in carcinoma of the
cervix. Am J Clin Oncol. 32:411–416. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Savanis G, Simatos G, Lekka I, Ammari S,
Tsikkinis C, et al: Abdominal metastases from lung cancer resulting
in small bowel perforation: report of three cases. Tumori.
92:185–187. 2006.PubMed/NCBI
|
|
11
|
Liao QH and Xia K: Small intestine
melanoma: case report and literature review. Chin J Digestion.
26:420–421. 2006.(In Chinese).
|
|
12
|
Green JA, Kirwan JM, Tierney JF, Symonds
P, Fresco L, et al: Survival and recurrence after concomitant
chemotherapy and radiotherapy for cancer of the uterine cervix: a
systematic review and meta-analysis. Lancet. 358:781–786. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Jemal A, Siegel R, Xu J and Ward E: Cancer
statistics, 2010. CA Cancer J Clin. 60:277–300. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Tan LT and Zahra M: Long-term survival and
late toxicity after chemoradiotherapy for cervical cancer - the
Addenbrooke’s experience. Clin Oncol (R Coll Radiol). 20:358–364.
2008. View Article : Google Scholar
|
|
15
|
Ren HB, Wu HY, Bao ZH, et al: Analysis of
curative effect for concurrent chemoradiotherapy versus neoadjuvant
chemotherapy for stage IIB–IIIB cervical cancer. Cancer Research
and Clinic. 21:185–187. 2009.
|
|
16
|
Goncalves A, Fabbro M, Lhommé C, Gladieff
L, Extra JM, et al: A phase II trial to evaluate gefitinib as
second-or third-line treatment in patients with recurring
locoregionally advanced or metastatic cervical cancer. Gynecol
Oncol. 108:42–46. 2008. View Article : Google Scholar
|
|
17
|
Antler AS, Ough Y, Pitchumoni CS, Davidian
M and Thelmo W: Gastrointestinal metastases from malignant tumors
of the lung. Cancer. 49:170–172. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Nishizawa Y, Kobayashi A, Saito N, et al:
Surgical management of small bowel metastases from primary
carcinoma of the lung. Surg Today. 42:233–237. 2012. View Article : Google Scholar
|
|
19
|
McNeill PM, Waqman LD and Neifeid JP:
Small bowel metastases from primary carcinoma of the lung. Cancer.
59:1486–1489. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Rossi G, Marchioni A, Romagnani E,
Bertolini F, Longo L, Cavazza A and Barbieri F: Primary lung cancer
presenting with gastrointestinal tract involvement:
clinicopathologic and immunohistochemical features in a series of
18 consecutive cases. J Thorac Oncol. 2:115–120. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Kim SY, Ha HK, Park SW, Kang J, Kim KW,
Lee SS, Park SH and Kim AY: Gastrointestinal metastasis from
primary lung cancer: CT findings and clinicopathologic features.
AJR Am J Roentgenol. 193:W197–W201. 2009. View Article : Google Scholar : PubMed/NCBI
|