Introduction
Inflammatory fibroid polyps (IFPs) are rare, benign
mesenchymal tumors that can occur throughout the gastrointestinal
tract (1,2). The exact incidence of IFPs remains
unclear. The tumor occurs most frequently in the stomach of adults
and usually presents as a polypoid mass with a size of 1–5 cm.
Although the majority of patients have a nonspecific presentation,
those with small intestine lesions more commonly form a symptomatic
mass causing obstruction by intussusception (1–5). IFPs
are generally considered to be benign tumors with no malignant
potential, and therefore local excision is an adequate treatment.
Small, pedunculated IFPs may be successfully removed by endoscopic
submucosal dissection (1–5). Mutations in platelet-derived growth
factor receptor α (PDGFRA; chromosome 4q12) have been indicated to
be involved in the development of this tumor (2–5). IFPs
are submucosa-based lesions that frequently extend into the
overlying mucosa; however, they rarely spread under the muscularis
propria (1,2,6). The
current study presents an unusual case of a PDGFRA wild-type ileal
IFP that extended into the subserosal layer. Written informed
consent was obtained from the patient.
Case report
A 48-year-old female visited the Department of
Surgery, Chonbuk National University Hospital (Jeonju, Republic of
Korea) for abdominal pain that had persisted for seven days. The
results of routine hematological tests were within normal limits. A
plain abdominal radiographical examination was unremarkable. The
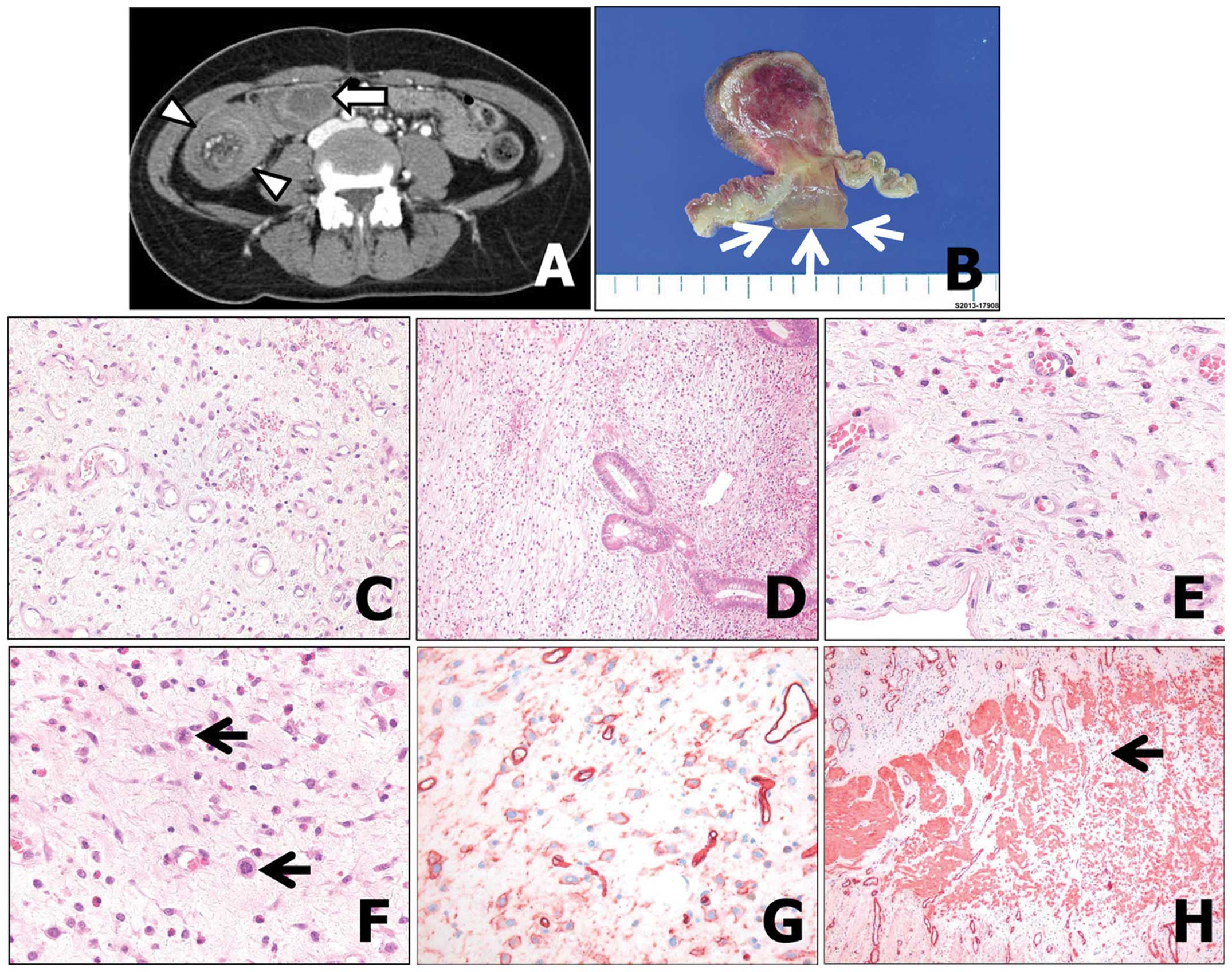
patient underwent contrast-enhanced abdominal computed tomography,
which revealed an ileocecal-type intussusception in the right lower
quadrant of the abdomen (Fig. 1A).
There was an oval-shaped, 3.5-cm mass in the ileum, which was
believed to be the lead point of intussusception. Segmental
resection of the intussuscepted ileum was performed. The excised
bowel segment revealed a 4.0×3.0-cm, luminal, polypoid mass that
extended into the subserosa. The cut surface was myxoid and showed
multiple hemorrhagic foci (Fig.
1B). Histologically, the tumor consisted of a mixture of
bland-looking epithelioid, stellate and spindle cells, loosely
distributed in a fibromyxoid stroma, with an abundant vascular
network (Fig. 2A). The tumor cells were arranged in a random
pattern; there was no so-called onion-like growth arrangement of
the spindle cells around the glands and blood vessels. The tumor
also revealed heavy eosinophilic infiltration with other
inflammatory cells, including plasma cells, lymphocytes,
histiocytes and mast cells. The majority of tumor cells were
composed of epithelioid cells, and individual cells exhibited
smooth, oval nuclei with modest eosinophilic cytoplasm. The
infiltrating tumor cells disrupted the muscularis mucosa above the
tumor cells and the muscularis propria below the tumor cells, and
extended into the subserosa, suggesting a neoplastic nature of this
lesion (Fig. 2B and C). There were 3–5 mitoses per 50 high-power
fields (HPFs) (Fig. 2D). Immunohistochemically, the tumor cells
were positive for vimentin and cluster of differentiation (CD)34,
while they were negative for keratin, PDGFRA, smooth muscle actin,
desmin, S-100 protein, DOG-1 and CD117 (c-kit) (Fig. 3A–C). The
proliferation marker Ki-67 was positive in ~10% of the tumor cells
(Fig. 3D). Sequencing analysis of c-kit exons 9, 11, 13 and 17, and
PDGFRA exons 12 and 18 indicated a wild-type status. The patient
has remained well for 12 months after surgery without treatment,
with no recurrence of the tumor.
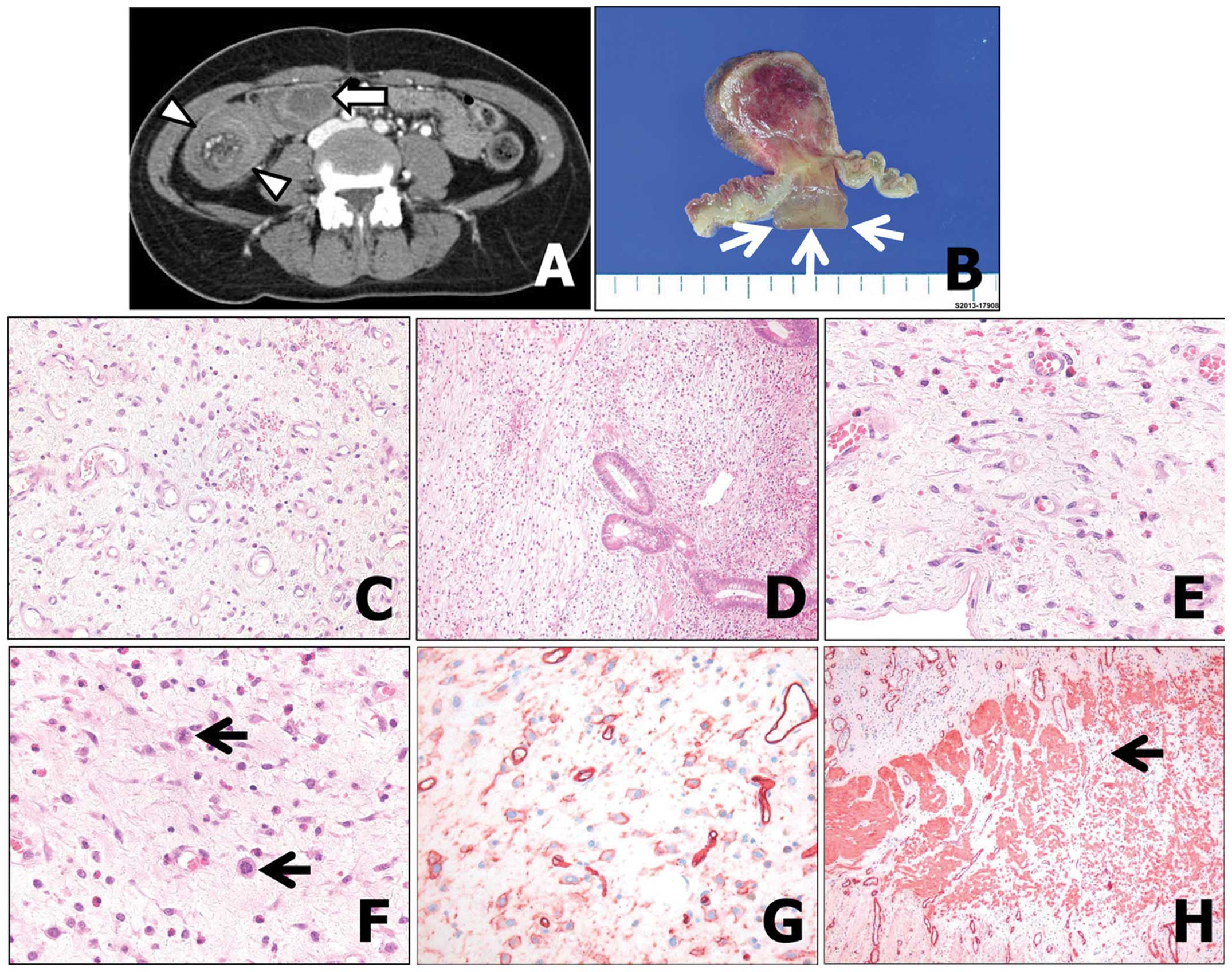 | Figure 1(A) Contrast-enhanced axial computed
tomography image of a 48-year-old female patient with ileocecal
intussusception. An ~3.5-cm oval-shaped mass can be observed as a
lead point (arrow), and mesenteric fat and vessels, as well as
bowel wall thickening of the intussusceptum and intussuscipiens
(arrowhead) are also apparent. (B) The intraluminal polypoid mass
extended into the subserosa (arrows). (C) The epithelioid tumor
cells are embedded in an edematous, fibromyxoid stroma with
prominent vasculature. The absence of concentric tumor cell
proliferation should be noted. (stain, hematoxylin and eosin;
magnification, ×200). (D) The tumor was centered in the submucosa
and extended into the mucosa (magnification, ×100). (E) The spindle
to epithelioid tumor cells were haphazardly arranged in the
edematous subserosa. The heavy inflammatory infiltrate with
eosinophils should be noted. (stain, hematoxylin and eosin;
magnification, ×400). (F) Despite low tumor cellularity, the tumor
cells showed mitotic figures (arrows) (stain, hematoxylin and
eosin; magnification, ×400). (G) The tumor cells were positive for
cluster of differentiation 34 (magnification, ×400). (H) Smooth
muscle actin staining showed a disrupted muscularis propria by
infiltrating tumor cells (arrow) (magnification, ×100). |
Discussion
IFPs are rare mesenchymal lesions of the digestive
system that were originally described by Vanek (7); they are considered reparative
processes. Recent molecular studies of IFPs identified
PDGFRA-activating mutations, suggesting a neoplastic nature to this
lesion (2–5). Histologically, IPFs are characterized
by proliferation of spindle, stellate or epithelioid cells
accompanied by an inflammatory reaction, particularly eosinophilic
granulocytes. The tumor cells are embedded in an edematous,
fibromyxoid stroma, with prominent vasculature. A characteristic
finding is the presence of concentric cuffing of the glands or
vessels by spindle-shaped tumor cells. Concentric cuffing of tumor
cells is more pronounced in gastric IFP than in intestinal IFP.
IFPs tend to arise within the submucosa and often involve the
mucosa (1,2,6).
In the present case, the IFP exhibited the following
unusual features: Firstly, the tumor cells obliterated the
muscularis propria and extended into the subserosa. IFPs are
considered benign tumors without any risk for recurrence or
metastasis following complete excision. The majority of IFPs are
centered within the submucosa and rarely spread to the muscularis
propria (1,2,6). A
study by Makhlouf and Sobin demonstrated that among 45 reported
cases of IFP, none extended into the serosa or subserosa tissue,
although 7% of small intestinal IFPs infiltrated the muscularis
propria (6). A search of the
literature found only one similar case study describing a rectal
IFP that exhibited attachment to the sacral bone, thus mimicking
rectal cancer (8). Secondly,
despite low tumor cellularity, the tumor cells demonstrated
relatively high proliferative activity, as shown by Ki-67 labeling
and mitotic figures. The majority of IFP cases have few or no
mitotic figures, and Ki-67 labeling is <1% (5,6). In
the study by Makhlouf and Sobin, only two out of the 45 IFPs showed
2–4 mitoses/50 HPFs, and no IFPs had more than 5 mitoses/50 HPFs
(6). The present findings of
subserosal extension of the lesion with disruption of the
muscularis propria by infiltrating tumor cells and proliferative
activity of the tumor cells supported a neoplastic nature of the
current IFP. The mutation and activation of PDGFRA contribute to
the development of IFPs (2–5). Huss et al reported that exon 12
PDGFRA mutations are more often associated with small intestinal
IFPs, whereas exon 18 PDGFRA mutations occur frequently in gastric
IFPs (5). A PDGFRA mutation or
PDGFR expression was not identified in the present case. the reason
for the lack of PDGFRA mutation for the current IFP is unclear. A
possible explanation is a false-negative sequence analysis possibly
resulting from the cellularity of these lesions, or the degradation
of tumor DNA in the paraffin blocks, among other factors. This
assumption is less likely in the present case, which showed no
PDGFR expression, as none of the PDGFR-negative IFPs revealed
PDGFRA mutations, although they showed typical histological
features of IFPs (3). It has also
been suggested that certain small intestinal IFPs are caused by
molecular mechanisms other than PDGFRA activation (4). Indeed, previous studies showed that
only 47 of 81 (58.0%) IFPs of the small intestine carried mutations
in the PDGFR gene (2–5). It is difficult at present to elucidate
the underlying mechanisms of this condition; further studies with a
larger number of similar cases will be necessary to characterize
the phenotype and nature of this tumor. After eight months of
follow-up, the patient is in good health and no evident recurrence
of the tumor has been detected.
Acknowledgements
This study was supported by the National Research
Foundation of Korea (NRF) grant funded by the Korean Government
(MSIP) (No. 2008 0062279).
References
|
1
|
Liu TC, Lin MT, Montgomery EA and Singhi
AD: Inflammatory fibroid polyps of the gastrointestinal tract:
spectrum of clinical, morphologic, and immunohistochemistry
features. Am J Surg Pathol. 37:586–592. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Daum O, Hatlova J, Mandys V, et al:
Comparison of morphological, immunohistochemical, and molecular
genetic features of inflammatory fibroid polyps (Vanek’s tumors).
Virchows Arch. 456:491–497. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schildhaus HU, Cavlar T, Binot E, et al:
Inflammatory fibroid polyps harbour mutations in the
platelet-derived growth factor receptor alpha (PDGFRA) gene. J
Pathol. 216:176–182. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lasota J, Wang ZF, Sobin LH and Miettinen
M: Gain-of-function PDGFRA mutations, earlier reported in
gastrointestinal stromal tumors, are common in small intestinal
inflammatory fibroid polyps. A study of 60 cases. Mod Pathol.
22:1049–1056. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Huss S, Wardelmann E, Goltz D, et al:
Activating PDGFRA mutations in inflammatory fibroid polyps occur in
exons 12, 14 and 18 and are associated with tumour localization.
Histopathology. 61:59–68. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Makhlouf HR and Sobin LH: Inflammatory
myofibroblastic tumors (inflammatory pseudotumors) of the
gastrointestinal tract: how closely are they related to
inflammatory fibroid polyps? Hum Pathol. 33:307–315. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Vanek J: Gastric submucosal granuloma with
eosinophilic infiltration. Am J Pathol. 25:397–411. 1949.PubMed/NCBI
|
|
8
|
Jin JS, Wu CS, Yeh CH, Huang BP and Tsao
TY: Inflammatory fibroid polyp of rectum mimicking rectal cancer.
Kaohsiung J Med Sci. 29:460–463. 2013. View Article : Google Scholar : PubMed/NCBI
|