Introduction
Tumors arising from the renal sinus are rare. To the
best of our knowledge, only three cases of tumors arising from the
renal sinus have been reported in the literature to date (1–3). In
1999, Amin et al (1)
reported the first known case of a renal sinus tumor with
pathologogy of a myelolipoma. Hemangiomas, liposarcomas and
myelolipomas have been found originating from the renal sinus. This
report presents three cases of renal sinus tumors: Angioleiomyoma,
angiomyolipoma and lipoma, respectively. Currently they are
difficult to diagnose using imaging alone when they originate in
this location and biopsies may not yield a definitive answer.
Management options include both conservative and surgical
approaches depending upon the certainty of the diagnosis, the
progression of the patient’s symptoms and evidence of growth.
Writted informed consent was obtained from all patients.
Case reports
Case 1
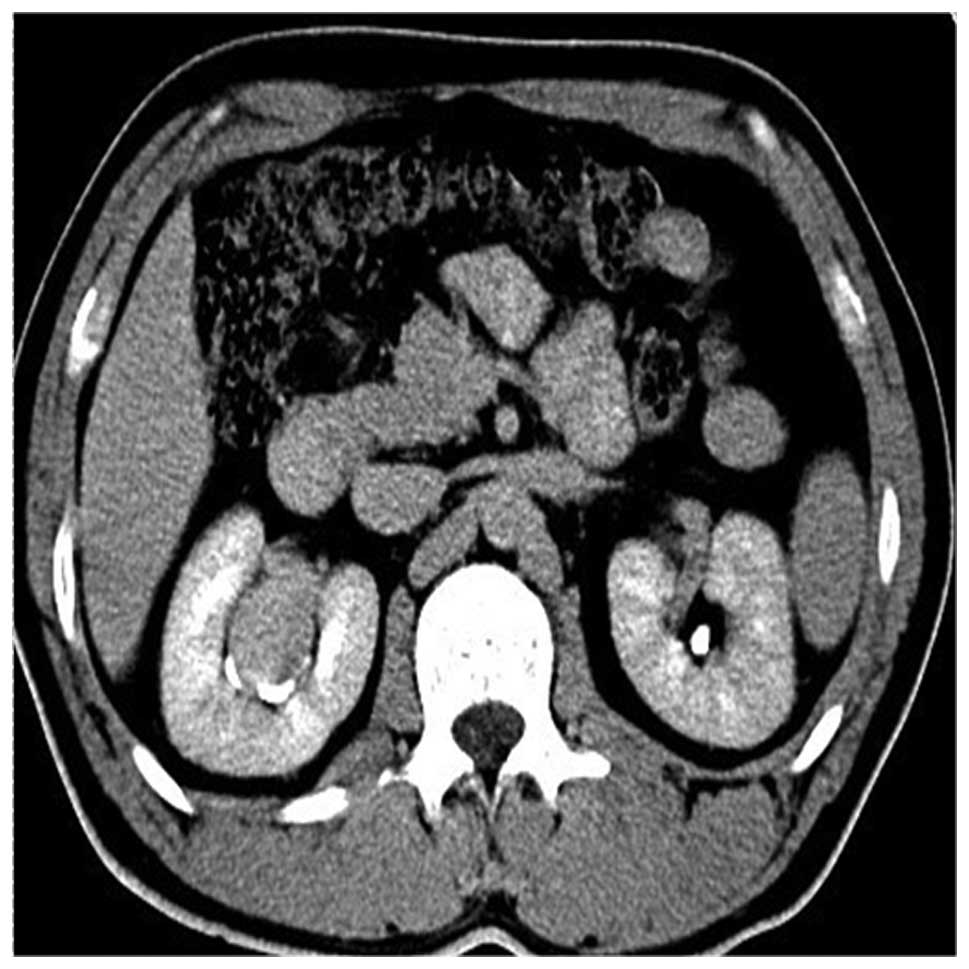
A 33-year-old man presented to the Shengli Oilfield
Central Hospital (Dongying, China) with right flank pain for 6
months. Ultrasonographic observation demonstrated a mass measuring
~3.5 cm in diameter in the right renal sinus. A computerized
tomography (CT) scan of the abdomen revealed a non-enhancing,
homogeneous, smooth and obvious mass, which measured ~3.5×3.7×3.0
cm in size (Fig. 1). Based on the
results of the CT scan, the patient was diagnosed with a pelvic
tumor. Intravenous urography (IVU) showed that the right renal
pelvis and renal calyx were compressed, but the filling defect was
not observed in the renal pelvis. All these changes suggested that
the tumor mass may have arisen from the right renal pelvis.
Surgical exploration of the renal sinus tumor was performed. An
entity mass that was well-circumscribed and ~3.5 cm in diameter was
situated in the renal sinus, and was adherent to the renal capsule
and pelvis. Frozen tissue section examination revealed that the
tumor was benign and originated from the mesenchymal tissue.
Radical resection of the neoplasm was performed and normal renal
tissues remained. Postoperative pathology results revealed that the
tumor was well-circumscribed with well-differentiated smooth muscle
cells and thick-walled vessels. Immunohistochemistry analysis
showed positive staining for vimentin, smooth muscle actin, actin,
CD34 and negative staining for Des, S-100 and neuron-specific
enolase. The patient was diagnosed with angioleiomyoma due to the
pathology results. The patient has been followed up for 3 years and
has demonstrated no recurrences or any other problems associated
with this lesion.
Case 2
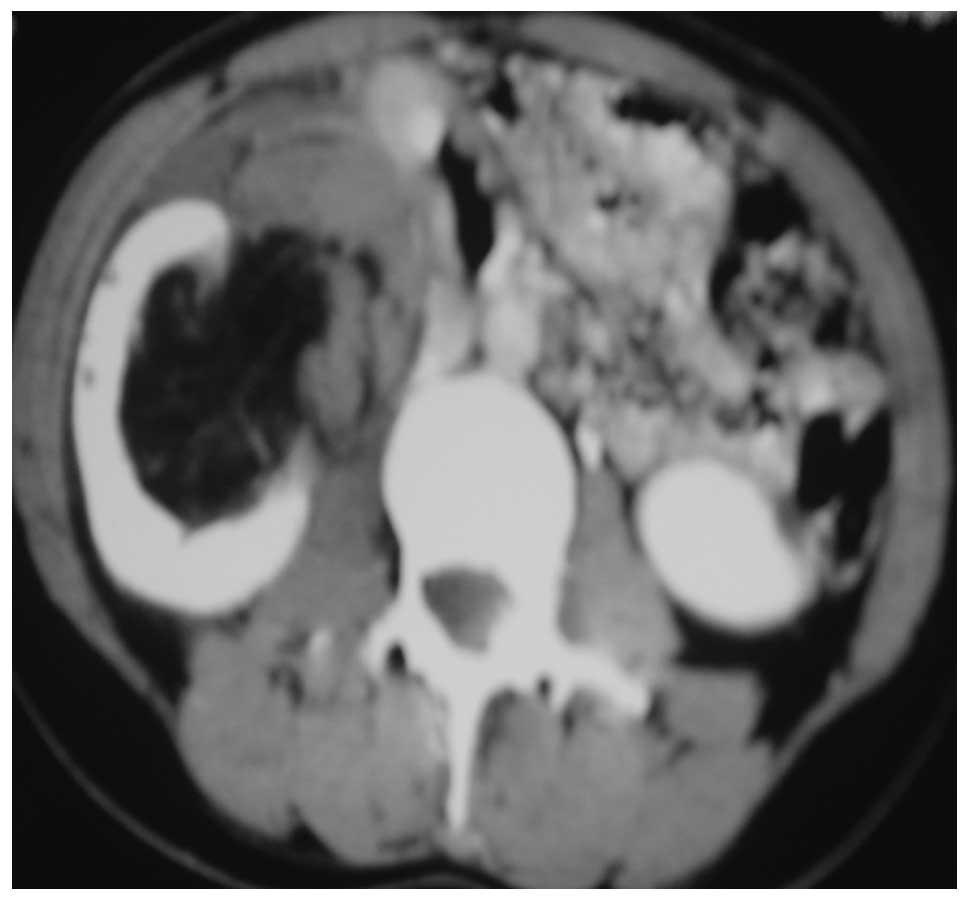
A 34-year-old woman was referred to Shengli Oilfield
Central Hospital due to sudden lumbago in the right flank with
gross hematuria for 3 days on July 25, 2007. Right upper flank
tenderness and percussion pain in the right kidney were observed
during physical examination. The ultrasonography results of the
right kidney demonstrated a hyperechoic mass in the right renal
sinus, which measured ~8.4×5.5×8.5 cm in size. An oval and
low-attenuation mass with a CT value of −70 HU in the right kidney
sinus was identified in the CT scans, which was ~8×6×8 cm in size.
An enhancing heterogeneous mass situated in the right kidney
(Fig. 2), right renal capsular
thickening, low density and subcapsular mass were observed in the
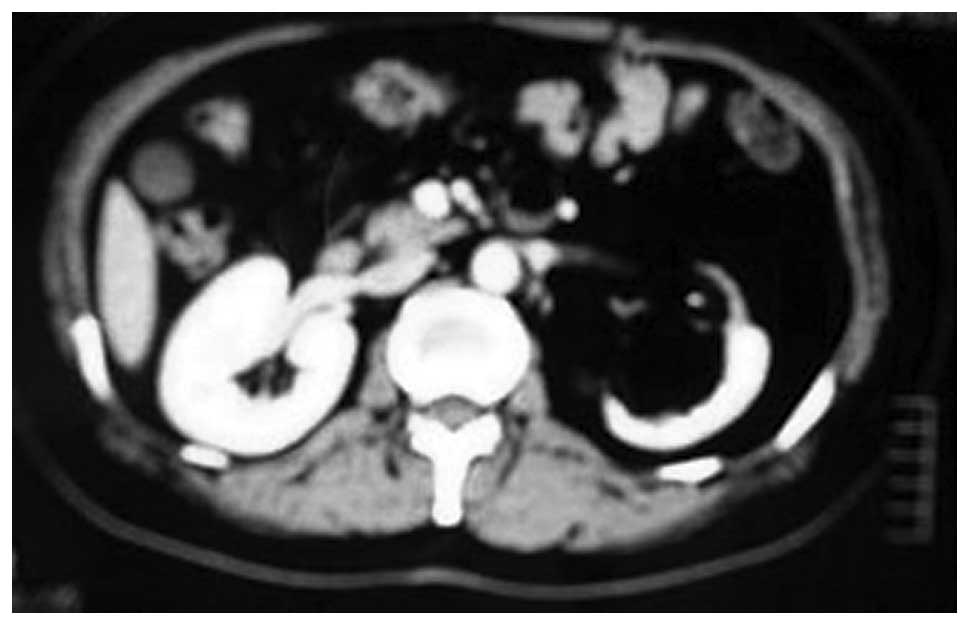
contrast-enhanced CT scans. IVU results showed the lower collective
system was compressed without filling defects in the right renal
pelvis (Fig. 3). The left renal
function was good, although accompanied with delayed right kidney
enhancement. The patient was diagnosed with renal angiomyolipoma of
the right kidney and right renal tumor resection was performed. The
tumor adherent to surrounding tissues was ~8 cm in diameter and was
situated in the right renal sinus. The patient underwent right
kidney excision due to uncontrolled diffuse hemorrhage, and damage
to the right renal pelvis could not be repaired. Postoperative
pathology reports confirmed the diagnosis of angiomyolipoma of the
right kidney. The patient exhibited a good physical condition and
left the hospital after 7 days. The patient has been followed up
for 10 months and has shown no recurrences or metastases.
Case 3
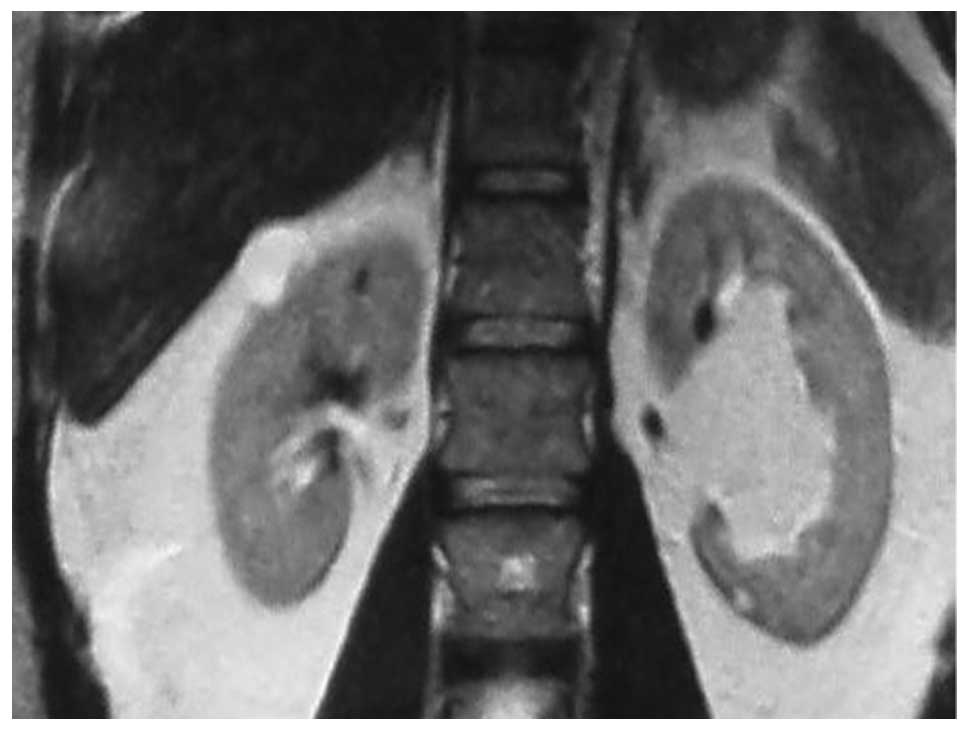
A 55-year-old woman presented to the Second Hospital
of Tianjin Medical University (Tianjin, China) with lumbago in the
left flank, which had persisted for 1 year. Upon physical
examination, tenderness in the left flank was observed. B-mode
ultrasonography showed hyperechoic lesions in the left renal hilum.
Contrast-enhanced CT scan of the abdomen showed a non-enhancing,
homogenous and obvious mass in the left renal sinus, measuring
8×5×5 cm in size with a CT value ranging from −50 HU to −35 HU
(Fig. 4). IVU results showed the
collective system of the left kidney was compressed. Magnetic
resonance imaging (MRI) showed a high signal on T1 weighted image
(T1WI) and T2WI, but a low signal in fat suppression imaging
(Fig. 5). The patient was diagnosed
with lipoma of the left renal sinus. A left radical nephrectomy was
performed. The tumors all formed a solid, large, smooth and evident
mass. The cut surface of the tumor was yellow. Postoperative
pathological reports confirmed the diagnosis of lipoma of the left
renal sinus. The patient has been followed up for 4 years and has
shown no recurrences.
Discussion
The renal sinus is a cavity within the kidney
containing the pelvis and calyces, adipose tissue, kidney vessels,
nerves and lymphatic tissues, and is a continuation of the renal
hilum. The types of tumor tissues in the renal sinus are extensive,
including fat, lymphatic, nerve and vascular tissues. Lipomas and
liposarcomas originate from fat tissue, Castleman’s disease and
lymphoma originate from lymphatic tissue, ganglion cell tumors
originate from nerve tissue, and angioleiomyoma and
hemangiopericytoma originate from vascular tissue (4,5).
Tumors arising from the renal sinus are rare and
two-thirds of such tumors are benign (6). The most common type of tumor arising
from the renal sinus is lipoma (7,8).
Previous studies have identified that the exclusive differential
diagnosis of lesions or those involving the renal hilum includes
hemangioma, angiomyolipomas, leiomyoma, myeloid lipoma, Castleman’s
disease and Masson’s tumors (7,9–11).
Malignant tumors, such as liposarcoma, non-Hodgkin’s lymphoma and
malignant paragangliomas have occasionally been reported (12–14).
By virtue of the association of adipose tissue,
imaging techniques, such as CT and MRI, can exaggerate internal
enhancing or low attenuation and therefore may strongly suggest the
diagnosis of renal sinus tumors. Simultaneously, diagnosis of renal
sinus tumors mainly depends on the imaging results. Ultrasonography
reveals occupying lesions, or blood vessels. CT or MRI scans are
used to evaluate the developing stage and invasive range of the
neoplasm. Multidetector CT offers a faster analysis, due to a
thinner layer of scanning and a higher spatial resolution (15). Furthermore, three-dimensional
reconstructive CT scans can more accurately determine lesions in
the scope of complex renal sinus lesions compared with other
imaging methods. The CT features of primary renal sinus tumors are
as follows: i) commonly located within the renal sinus, and the
renal parenchyma and pelvis may be encroached by a malignant tumor;
ii) an obvious boundary between tumors and the renal collective
system, with frequently compressed pelvis and calyces, and a
lighter renal seeper; iii) enhanced CT scanning demonstrates
compressed vessels situated in the renal hilum and iv) the
excretion period of the enhancing CT scan reveals compressed renal
pelvis and calyceal without filling defects (16–18).
MRI imaging has more advantages than CT in revealing the invasion
of the renal vein and inferior vena cava. This technique may be
used in patients with kidney failure and in those with allergies
using contrast agents. IVU may also be used to assess whether the
tumor has affected the kidney collecting system and kidney
function. Primary renal sinus neoplasms are often accompanied by a
compressed collecting system (19–21).
The absence of filling defects in the pelvis and calyces can be
used to distinguish a primary renal pelvis tumor. It has been
suggested that malignant tumors accompany the renal pelvis
infringement when the kidney collecting system is irregular
(22,23). One patient in the present study was
diagnosed with a renal pelvis tumor, which was thought to have
originated from the renal sinus and without renal pelvis filling
defect. The combined application of IVU, CT and MRI scans may
improve the diagnosis rate (15).
It is difficult to obtain a qualitative diagnosis of renal sinus
tumors, while angioleiomyomas and angiomyolipomas are markedly
enhanced (11). In the present
study, two patients were diagnosed with renal sinus angiomyolipomas
and one was diagnosed with lipoma based on the appearance of
adipose tissues and the CT values (approximately −70 and −50 HU,
respectively).
The clinical manifestations of renal sinus tumors
are nonspecific; a number of patients present with lumbago and a
few patients present with hematuria and urinary tract infections
(24–26). Symptoms present when the diameter of
the tumor is >4 cm. Hematuria was observed to be caused when the
tumor was larger and accompanied with renal pelvis involvement. To
the best of our knowledge, no symptoms for benign tumors have been
observed when the diameter of the tumor is <4 cm; therefore,
surgery is unnecessary before the appearance of renal seeper.
Tumors with apparent symptoms and a diameter >4 cm should be
resected. In the present three cases, we preserved the kidney as
far as possible during surgery of the three reported cases.
Previously reported neoplasms required kidney resection when the
diameter was >7 cm, particularly benign tumors that occupied the
entire kidney sinus (27). In the
present study, two cases demonstrated the same condition; the tumor
diameter was >7 cm and occupied the entire kidney sinus,
involving the renal pelvis or with serious adhesion. Therefore,
nephrectomy was performed. Renal sinus tumors would remain
undiagnosed unless the possibility of hemangioma via percutaneous
or intraoperative biopsy is excluded (2). In the current study, one patient was
diagnosed with a benign tumor based on the intraoperative biopsy
results and underwent excision of the tumor, whilst simultaneously,
preserving the kidney. Therefore, surgical exploration is advocated
before excluding the possibility of a renal sinus tumor, in order
to avoid unnecessary nephrectomy. Renal sinus malignant tumors,
particularly those with renal parenchyma infringement, should
undergo radical nephrectomy where the kidneys are removed
simultaneously with the with tumor emboli (3).
In conclusion, primary tumors in the renal sinus are
rare and the majority are benign, but are often misdiagnosed as
renal pelvic carcinoma. The prognosis of renal sinus tumors is
good. CT, MRI and IVU analysis have great value in orientation and
qualitative diagnosis of renal sinus tumors. The treatment
approaches, however, may be established by correlating the clinical
symptoms, tumor size and nature. Preserving the kidney during
surgery as far as possible is key for the treatment of patients
with renal sinus tumors.
References
|
1
|
Amin MB, Tickoo SK and Schultz D:
Myelolipoma of the renal sinus: an unusual site for a rare
extra-adrenal lesion. Arch Pathol Lab Med. 123:631–634.
1999.PubMed/NCBI
|
|
2
|
Gupta NP, Kumar P, Goel R and Dinda AK:
Renal sinus hemangioma simulating renal mass: a diagnostic
challenge. Int Urol Nephrol. 36:485–487. 2004. View Article : Google Scholar
|
|
3
|
Matsushita M, Ito A, Ishidoya S, Endoh M,
Moriya T and Arai Y: Intravenous extended liposarcoma arising from
renal sinus. Int J Urol. 14:769–770. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Akaza H, Koiso K and Niijima T: Clinical
evaluation of urothelial tumors of the renal pelvis and ureter
based on a new classification system. Cancer. 59:1369–1375. 1987.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Mazairac AH and Joles JA: Renal sinus
adiposity and hypertension. Hypertension. 56:814–815. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Lopez-Beltran A, Scarpelli M, Montironi R
and Kirkali Z: 2004 WHO classification of the renal tumors of the
adults. Eur Urol. 49:798–805. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Metro MJ, Ramchandani P, Banner MP, et al:
Angiomyolipoma of the renal sinus: diagnosis by percutaneous
biopsy. Urology. 55:2862000. View Article : Google Scholar
|
|
8
|
Diamond A, Kodroff M and Ravitz G: Renal
sinus angiomyolipoma. Urology. 9:221–223. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Carcamo Valor P, Martínez-Piñeiro JA,
López-Tello J, Picazo García M and Contreras Rubio F:
Hemangiopericytoma of the renal sinus: report of a case and review
of the literature. Arch Esp Urol. 49:944–949. 1996.(In Spanish).
PubMed/NCBI
|
|
10
|
Yoshida M, Inoue S, Yanagisawa R, Kishi H
and Takahashi M: A case of multiple renal leiomyoma located at
renal sinus and hilus. Hinyokika Kiyo. 36:937–940. 1990.(In
Japanese). PubMed/NCBI
|
|
11
|
Johraku A, Miyanaga N, Sekido N, et al: A
case of intravascular papillary endothelial hyperplasia (Masson’s
tumor) arising from renal sinus. Jpn J Clin Oncol. 27:433–436.
1997. View Article : Google Scholar
|
|
12
|
Shimazui T, Nutahara K, Ishii Y and Horibe
Y: A case of malignant paraganglioma within the renal sinus.
Hinyokika Kiyo. 31:2027–2033. 1985.(In Japanese). PubMed/NCBI
|
|
13
|
Honda H, Lu CC, Franken EA Jr, Bonsib SM,
Yuh WT and Williams RD: Renal sinus malignant lymphoma: a case
report. J Comput Tomogr. 12:190–192. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yaman O, Soygür T, Ozer G, Arikan N and
Yaman LS: Renal liposarcoma of the sinus renalis. Int Urol Nephrol.
28:477–480. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Chaabouni MN and Mhiri MN: Pseudotumoral
lipomatosis of the renal sinus. Ann Urol (Paris). 27:93–96.
1993.(In French).
|
|
16
|
Katabathina VS, Vikram R, Nagar AM,
Tamboli P, Menias CO and Prasad SR: Mesenchymal neoplasms of the
kidney in adults: imaging spectrum with radiologic-pathologic
correlation. Radiographics. 30:1525–1540. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Drewniak T, Rzepecki M, Juszczak K,
Moczulski Z, Reczyńska K and Jakubowska M: Methodology and
evaluation of the renal arterial system. Cent European J Urol.
66:152–157. 2013.
|
|
18
|
Shetty A and Adiyat KT: Comparison between
helical computed tomography angiography and intraoperative
findings. Urol Ann. 6:192–197. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Carvalho JC, Thomas DG, McHugh JB, Shah RB
and Kunju LP: p63, CK7, PAX8 and INI-1: an optimal
immunohistochemical panel to distinguish poorly differentiated
urothelial cell carcinoma from high-grade tumours of the renal
collecting system. Histopathology. 60:597–608. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kamath A, Rosenkrantz AB and Bosniak MA:
MRI findings of angiomyolipoma of the renal sinus in 5 cases. J
Comput Assist Tomogr. 34:915–920. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Moch H, Artibani W, Delahunt B, Ficarra V,
Knuechel R, Montorsi F, Patard JJ, Stief CG, Sulser T and Wild PJ:
Reassessing the current UICC/AJCC TNM staging for renal cell
carcinoma. Eur Urol. 56:636–643. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Kuzaka P, Pastewka K, Faryna J, Kuzaka B,
Pypno W and Wejman J: Nested variant of urothelial carcinoma of
renal pelvis-a case report. Pol J Pathol. 65:74–77. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lin Z, Chng JK, Chong TT and Soo KC: Renal
pelvis squamous cell carcinoma with inferior vena cava
infiltration: Case report and review of the literature. Int J Surg
Case Rep. 5:444–447. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
He YF, Chen J, Xu WQ, Ji CS, Du JP, Luo HQ
and Hu B: Case report. Metastatic renal cell carcinoma to the left
maxillary sinus. Genet Mol Res. 13:7465–7469. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Ambrosio MR, Rocca BJ, Onorati M, Bellan
C, Barbanti G, del Vecchio MT and Tripodi S: Renal sinus
pseudolymphoma in a patient with multiple carcinomas: a case report
and a brief review of the literature. Histol Histopathol.
27:1327–1332. 2012.PubMed/NCBI
|
|
26
|
Shirotake S, Yoshimura I, Kosaka T and
Matsuzaki S: A case of angiomyolipoma of the renal sinus. Clin Exp
Nephrol. 15:953–956. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Choi YJ, Hwang TK, Kang SJ, Kim BK and
Shim SI: Hemangiopericytoma of renal sinus expanding to the renal
hilum: an unusual presentation causes misinterpretation as
transitional cell carcinoma. J Korean Med Sci. 11:351–355. 1996.
View Article : Google Scholar : PubMed/NCBI
|