Introduction
The endoscopic transsphenoidal route is considered
the standard approach for the surgical resection of sellar tumors
(1), which represent ~10% of all
intracranial tumors, with a mortality rate of ~4.4% and a
recurrence rate that varies between 6 and 21% (2). All of the various routes to the sella
(transethmoidal, transnasal and transseptal), whether microscopic
or endoscopic, pass through the sphenoid sinus to reach the sella.
However, the presence of a conchal sphenoid sinus is typically
considered to be one of the contraindications for the use of
transsphenoidal route due to the difficulties of intraoperative
localization and exposure of the sellar floor (3,4). The
current study presents two cases of resection of sellar tumors with
conchal sphenoid sinus via the endoscopic transsphenoidal route.
Written informed consent was obtained from the patient’s family and
the patient for case one and two, respectively.
Case reports
Case one
A 60-year-old female was admitted to the Department
of Otolaryngology - Head and Neck Surgery of the Third Xiangya
Hospital (Changsha, China) on August 28, 2011, presenting with a
two-day history of a severe headaches, projectile vomiting and
blepharoptosis of the left eye.
Nasal examination was normal. The right pupil size
was 2.5 mm (normal range, 2.5–5.0 mm) with normal papillary reflex
and the left pupil size was 4.0 mm with no papillary reflex. Visual
acuity and visual field of the two eyes were normal. No strabismus
or diplopia were observed and the eye movement was normal.
Endocrinological investigations demonstrated decreased
adrenocorticotropic hormone (ACTH; 1.10 pg/ml, normal range,
7.20–63.60 pg/ml) and luteinizing hormone (LH; 2.78 mIU/ml, normal
range, 15.90–54.00 mIU/ml), normal thyroid stimulating hormone
(TSH; 1.56 mIU/ml, normal range, 0.40–4.78 mIU/ml),
follicle-stimulating hormone (FSH; 15.96 mIU/ml, normal range,
23.00–116.30 mIU/ml), growth hormone (GH; 0.43 ng/ml, normal range,
0.12–9.88 ng/ml) and prolactin (PRL; 2.48 ng/ml, normal range,
1.80–20.30 ng/ml) (Table I).
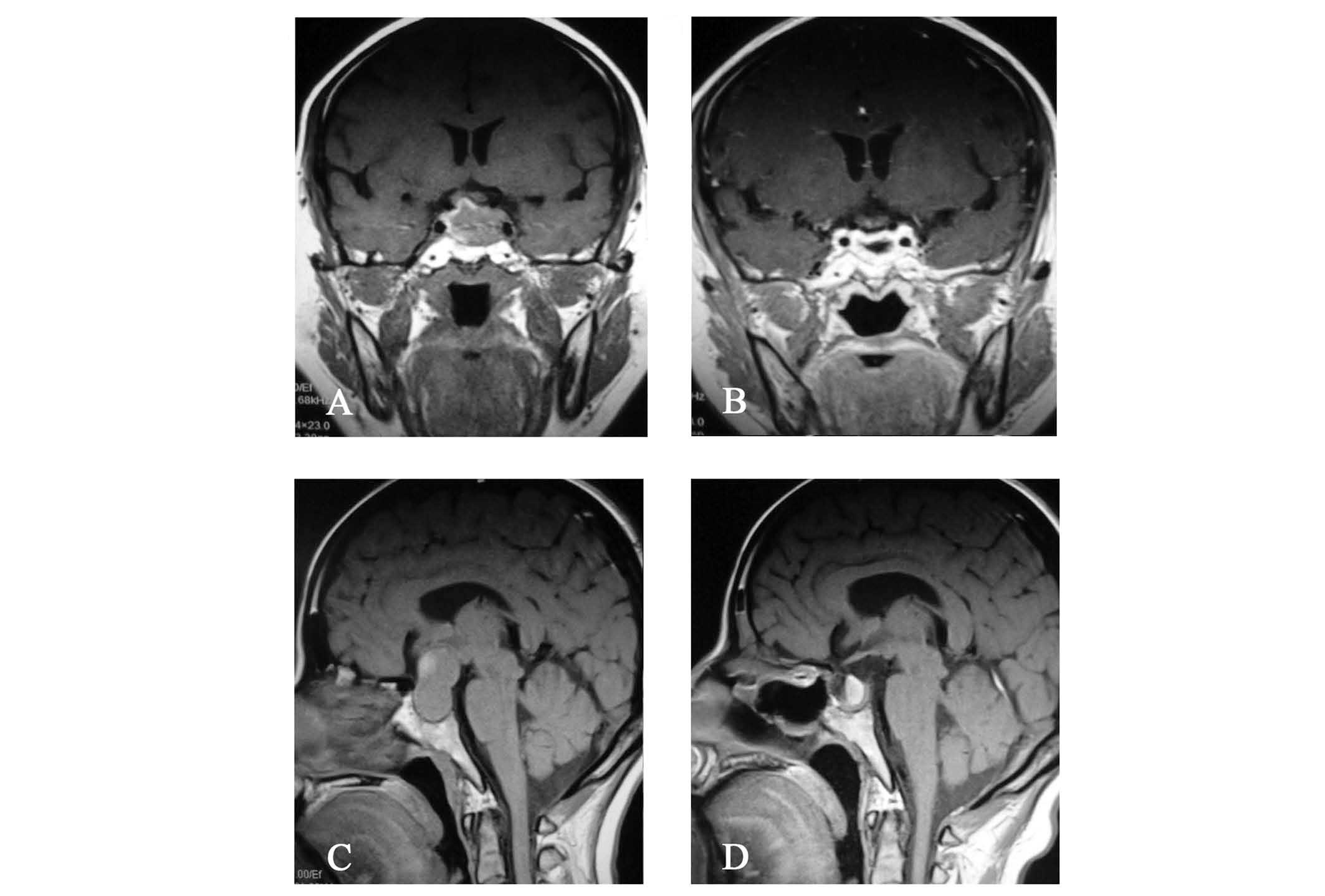
Magnetic resonance imaging indicated a sellar tumor extended into
the left cavernous sinus and a non-pneumatized sphenoid sinus
(Fig. 1A). Following the
aforementioned physical and clinical examinations, the tumor was
excised under general anesthesia via the endoscopic transsphenoidal
route. Skull base closure was achieved with a combination of
autologous fascia lata grafts, fibrin glue and nasoseptal flap(s).
The excised tumor was subjected to histopathology, which indicated
a diagnosis of pituitary adenoma.
 | Table IPreoperative endocrinological
investigations of the two cases. |
Table I
Preoperative endocrinological
investigations of the two cases.
| Endocrinological
investigation | Normal range | Case one | Case two |
|---|
| FSH | 23.00–116.30
mIU/ml | 15.96 mIU/ml | 4.09 mIU/ml |
| GH | 0.12–9.88 ng/ml | 0.43 ng/ml | 0.31 ng/ml |
| LH | 15.90–54.00
mIU/ml | 2.78 mIU/ml | 0.39 mIU/ml |
| ACTH | 7.20–63.60 pg/ml | 1.10 pg/ml | 21.09 pg/ml |
| PRL | 1.80–20.30 ng/ml | 2.48 ng/ml | 70.43 ng/ml |
| TSH | 0.40–4.78 mIU/ml | 1.56 mIU/ml | 3.29 mIU/ml |
Postoperatively, the patient developed transient
diabetes insipidus for six days, however no other complications,
such as intracranial infection, cerebrospinal fluid leakage,
intracerebral hemorrhage or cranial nerve palsies, were observed.
Blepharoptosis recovered on day 13 after surgery. A magnetic
resonance image captured one year following the surgery
demonstrated that total resection was achieved (Fig. 1B). No recurrence was observed prior
to the termination of follow-up, two years after the surgery was
performed.
Case two
A 45-year-old female presented with a three-month
history of vision loss and was treated in the Department of
Otolaryngology - Head and Neck Surgery of the Third Xiangya
Hospital on December 3, 2013.
The nasal examination was normal. The patient’s
visual acuity (normal range, >1.0) was measured at 4 m using a
retroilluminated logarithm of the minimum angle of resolution chart
with tumbling-E optotypes (Precision Vision, La Salle, IL, USA),
which revealed that the [visio oculus sinister (VOS)] in the left
eye was counting fingers/30 cm and the [visio oculus dexter (VOD)]
in the right eye was 0.3. Additionally, a visual field defect of
bitemporal hemianopia was observed. Endocrinological investigations
demonstrated elevated PRL (70.43 ng/ml, normal range, 1.80–20.30
ng/ml), decreased FSH (4.09 mIU/ml, normal range, 23.00–116.30
mIU/ml) and LH (0.39 mIU/ml, normal range, 15.90–54.00 mIU/ml), and
normal TSH (3.29 mIU/ml, normal range, 0.40–4.78 mIU/ml), GH (0.31
ng/ml, normal range, 0.12–9.88 ng/ml) and ACTH levels (21.09 pg/ml,
normal range, 7.20–63.60 pg/ml) (Table
I). Magnetic resonance imaging indicated the presence of a
sellar tumor, which had extended into the suprasellar cistern and
caused compression of the optic nerves and optic chiasma, as well
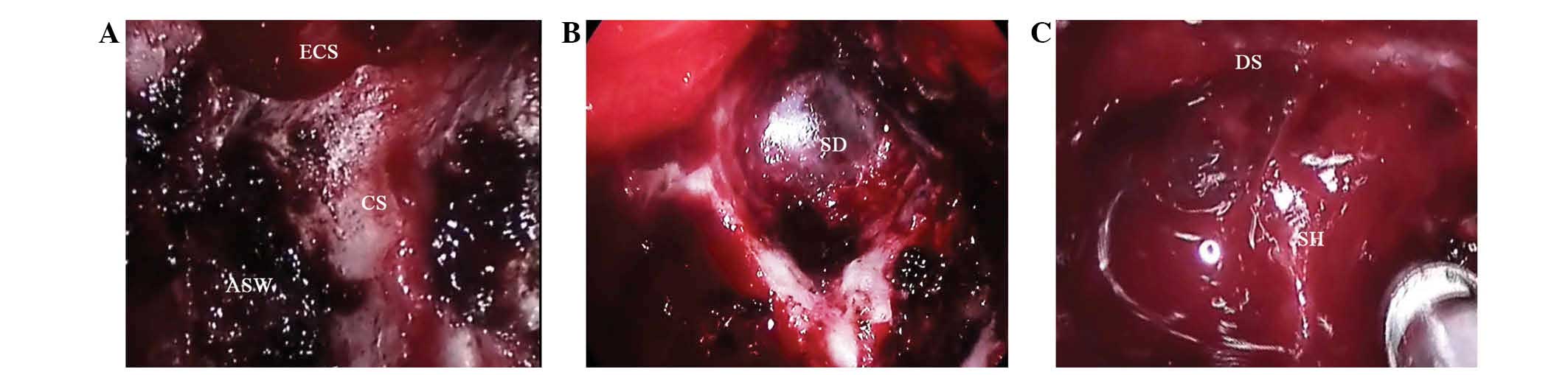
as a non-pneumatized sphenoid sinus (Fig. 1C). The surgical technique utilized
in case two was identical to that used in case one; the
intraoperative view is shown in Fig.
2. Subsequent histopathological examination of the lesion
indicated a diagnosis of pituitary adenoma.
Postoperatively, the patient developed transient
diabetes insipidus for 11 days. Prior to discharge (13 days
following surgery), visual acuity was determined to be 0.8 VOS and
1.0 VOD, and visual field was fully recovered. Magnetic resonance
imaging indicated that total resection of the tumor had been
achieved, however, a hematoma was observed in the posterior
pituitary fossa with no clinical symptoms (Fig. 1D). No additional complications were
observed at the most recent follow-up examination in February
2014.
Discussion
Sphenoid sinuses develop within the sphenoidal
concha from the third embryonic month and may result in varying
degrees of pneumatization in the corpora ossis sphenoidalis by the
age of 14 years (5). According to
the commonly used classification system proposed by Hammer and
Radberg (6), the pneumatization of
the sphenoid sinus is divided into three types: Conchal, presellar
and sellar. The conchal type accounts for ~2% of patients who
undergo surgery for sellar tumors (7) and the conchal non-pneumatized sphenoid
was previously considered to be a contraindication to the
transsphenoidal route to the sella due to its small sellar floor
and poor anatomical landmarks, such as the optic nerve canal,
opticocarotid recess and internal carotid arteries canal. Thus, the
transsphenoidal approach is typically considered to be less
favorable in cases of conchal non-pneumatized sphenoid sinus. In
the present report, the two conchal sphenoid sinuses were accessed
safely.
As determined in the present study, the key points
with regard to the surgical procedure were as follows: i) Full use
must be made of the preoperative imaging data, and the
surgery-associated anatomical characteristics, as well as the depth
and width of the sellar tumor requiring removal, must be
determined; ii) the rostrum sphenoidale and posterior sections of
the nasal septum must be used as the reference point for the
midline, at which a position 2 cm above the choana atresia should
be selected as the hypothetical position of the ostium of the
sphenoidal sinus. Subsequently, the sphenoidal sinus should be
entered via the hypothetical ostium; iii) a high-speed drill may be
considered as an alternative to the osteotome and rongeur as it
appeared to confer a number of advantages in the present case,
including exerting a hemostatic effect on a small amount of
bleeding from the sellar tumor, a clean surgical view and improved
surgical safety; iv) lastly, in the event of bleeding, conventional
procedures, such as curettage and suction, are often ineffective,
and resection of the tumor may be achieved using a minimally
invasive suction-dissection instrument, which was key in the
success of the present surgical procedure (8).
In conclusion, for sellar tumors with
non-pneumatized sphenoid, transcranial approaches are usually
preferred by neurosurgeons, however, brain retraction and
manipulation of neurovascular structures during the procedure may
induce severe trauma and postoperative reactions, in addition to
numerous complications which may increase the duration of the
patient’s hospital stay. In the present study, a conchal
non-pneumatized sphenoid does not appear to be an absolute
contraindication for endoscopic transsphenoidal route in the
resection of sellar tumors; endoscopic transsphenoidal surgery has
a number of advantages when compared with other surgical
approaches, including decreased morbidity, improved panoramic
visualization and increased illumination and magnification.
Furthermore, a positive outcome may be achieved, in particular when
the surgery is performed by an experienced otolaryngologist.
However, due to the small sample size used in the present study,
future studies are required to confirm the efficacy and safety of
the endoscopic route in the resection of sellar tumors with
non-pneumatized sphenoid.
Acknowledgements
The present study was supported by the Hunan
Provincial Innovation Foundation for Postgraduate (China; grant no.
CX2013B125). The authors would like to thank Dr Yexun Song for
aiding with the data collection, Dr Tiansheng Wang for facilitating
the performance of the statistical analyses, and Professor Jiangbo
Chen and Professor Guolin Tan for assisting in the writing of the
manuscript.
References
|
1
|
Cavallo LM, Messina A, Cappabianca P, et
al: Endoscopic endonasal surgery of the midline skull base:
anatomical study and clinical considerations. Neurosurg Focus.
19:E22005.PubMed/NCBI
|
|
2
|
Cavallo LM, Solari D, Tasiou A, et al:
Endoscopic endonasal transsphenoidal removal of recurrent and
regrowing pituitary adenomas: experience on a 59-patient series.
World Neurosurg. 80:342–350. 2013. View Article : Google Scholar
|
|
3
|
Nomikos P, Fahlbusch R and Buchfelder M:
Recent developments in transsphenoidal surgery of pituitary tumors.
Hormones (Athens). 3:85–91. 2004. View Article : Google Scholar
|
|
4
|
Hamid O, EI Fiky L, Hassan O, et al:
Anatomic various of the sphenoid sinus and their impact on
trans-sphenoid pituitary surgery. Skull Base. 18:9–15. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Scuderi AJ, Harnsberger HR and Boyer RS:
Pneumatization of the paranasal sinuses: normal features of
importance to the accurate interpretation of CT scans and MR
images. AJR Am J Roentgenol. 160:1101–1104. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hammer G and Radberg C: The sphenoidal
sinus. An anatomical and roentgenologic study with reference to
transsphenoid hypophysectomy. Acta Radiol. 56:401–422. 1961.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kirnman J: Surgical aspects of the anatomy
of the sphenoidal sinuses and the sella turcica. J Anat.
124:541–553. 1977.
|
|
8
|
Song Y, Li H, Liu H, et al: Endoscopic
endonasal transsphenoidal approach for sellar tumors beyond the
sellar turcica. Acta Otolaryngol. 134:326–330. 2014. View Article : Google Scholar
|