Introduction
Scenarios designed in accordance with the World
Health Organization analgesic ladder are frequently used in
palliative medicine (1). Although
preliminary diagnoses are based on clinical signs, the
pathophysiology of pain is not always sufficiently examined in
palliative patients, thus, the diagnosis of acute chest or
epigastric pain may be a challenge. Furthermore, the diagnosis and
how a patient perceives their symptoms determine the efficacy of
the treatment (2). Acute chest pain
may be of cardiac origin, the most life-threatening type, or
non-cardiac origin, which includes gastrointestinal (GI) and non-GI
causes, for example bone, articular, muscular or pulmonary
conditions, herpetic, esophageal or psychiatric sources.
Non-cardiac acute chest pain may also be caused by drugs including
local anaesthetic (for example cocaine or thyroid hormone
preparation, such as levothyroxine), anticancer drugs (for example
doxorubicine, 5-fluorouracil, trastazumab and paclitaxel),
non-steroidal anti-inflammatory drugs (for example naproxen and
celecoxib) and antimigraine preparations (for example sumatriptan)
(3).
Sixty percent of cases of non-cardiac chest pain are
of esophageal origin, resulting from three predominant causes:
Gastroesophageal reflux disease, esophageal spasms caused by a
disturbed progression of the peristaltic wave or esophageal
hypersensitivity (abnormal sensory function) (4). In addition, retrosternal, chest or
epigastric pain may stem from inflammation involving the esophagus
(5,6) or a dysfunction of visceral sensory
neurons (7).
Proton pump inhibitors (PPIs) are used in the
treatment of gastroesophageal reflux disease. However, partial
responders to PPIs and patients with the other two abovementioned
causes of esophageal-induced chest/epigastric pain are treated with
pain modulators, including low-dose antidepressants such as,
imipramine, sertraline, trazodone, citalopram (5,8–10),
theophylline (11,12), nifedipine, diltiazem (5,8,9,13),
nitroglycerin, isosorbide nitrate, amyl nitrite (14) and botulinum toxin type A (5,8,9).
The vagus nerve and sympathetic trunk are sources of
esophageal plexus (5), and
gastrectomy (GE) is associated with the risk of non-selective
vagotomy (VT). Vagotomy may result in disturbed, receptive
relaxation reflexes and accommodation, causing hypertonic food to
rapidly reach the intestine, possibly triggering distension of the
intestinal wall (via increased water secretion) and resulting in
enzyme and bile salt dilution (15,16).
This dilution may generate a defect in heme-iron liberation,
impairment of vitamin A, D, E and K absorption, diarrhea and
hypovolemia. In addition, this reflex may act via hormones and
neurotransmitters to induce nausea or regurgitation, cramps, pain
and vasomotor reactions involving tachycardia, palpitations,
dysfunctional orthostatic regulation and cutaneous vascular
dilation (17). These symptoms,
observed 30–60 min following food consumption, are termed early
gastric emptying (18,19).
Furthermore, hypertonic food in the intestine
contains large quantities of carbohydrates, which are absorbed
quickly, causing a fast and high hyperglycemic peak followed by
reactive hypoglycemia, which may manifest as confusion, anxiety,
nervousness and activation of the sympathetic nervous system, for
example vasomotor reactions may cause flushing and tachycardia
(20). These symptoms, observed
90–180 min following food consumption, are termed late gastric
emptying (19).
Upon swallowing, the vagovagal reflex causes the
lower esophageal sphincter to open, however, in case of GI passage
disturbances (i.e., due to the presence of a tumor), the
peristaltic waves of the esophagus and the sphincter function are
disturbed. Food, fluid and mucous are accumulated in the dilated
esophagus (undigested food trapping), distending and irritating the
esophagus, and causing partially opioid-resistant spasmodic pain.
Thus, the process of emptying the esophagus is impaired and
regurgitation of food occurs, accompanied by retrosternal pain and
salivation. Furthermore, a concurrent dysfunction of the lower
esophageal sphincter results in no protection against gastric juice
and bile.
The current study presents the case of acute chest
and epigastrium pain in a male patient diagnosed with stomach
cancer and exhibiting metastases to the lungs, liver and lymph
nodes. Written informed consent for the publication of this study
was obtained from the patient’s wife.
Case report
Scoring systems
Pain was rated by the patient by means of a 0–10
Verbal Rating Scale (VRS) where 0/10 represents no pain and 10/10
represents the worst imaginable pain (21). In addition, a questionnaire
concerning symptoms and their intensity was conducted; the patient
estimated the intensity of their own pain using a scale of 0–3
(Likert scale), where 0/3 represented no symptoms and 3/3
represented very intense symptoms (21). The patient’s general health status
was assessed using the Karnofsky performance status scale (score
range, 0–100%) and the Eastern Cooperative Oncology Group (ECOG)
scale (score range, 0–5) (21).
Case presentation
A 41-old male patient diagnosed with stomach cancer,
with metastases to the lymph nodes, lungs and liver, who underwent
a subsequent GE and postoperative chemotherapy, was admitted to the
Palliative Medicine In-patient Unit of the University Hospital of
Lord’s Transfiguration (Poznan, Poland). The patient was admitted
to the hospice three months following the final chemotherapy
course, due to acute chest and epigastrium pain, which had lasted
for a number of hours (since morning the same day). The patient
complained of a clenching, smothering chest pain (VRS, 10/10),
permanent, diffused epigastrium pain (VRS, 10/10) and non-colic
left intra-abdominal pain (VRS, 10/10), accompanied by saliva
overproduction, nausea (Likert scale, 1/3), regurgitation (Likert
scale, 1/3) anorexia (Likert scale, 1/3), fatigue (Likert scale,
1/3), weakness (Likert scale, 1/3), worrying (Likert scale, 2/3),
nervousness (Likert scale, 1/3), hopelessness (Likert scale, 2/3),
internal tension (2/3) and anxiety (Likert scale, 1/3). In
addition, the patient reported a poor quality of life. The patient
received the following therapeutic agents prior to admission:
Tramadol, 100 mg orally (p.o.) every 4 h; metoclopramide, 10 mg
p.o. 3 times/day; diazepam, 5 mg/day p.o.; clorazepate, 10 mg/day
p.o.; megestrol, 20 ml/day p.o.; and enoxaparine, 0.4 ml/day (40
mg/day) subcutaneously. The patient refused to undergo the
continuous administration of analgesics; instead, the patient only
used these agents in the case of severe pain. On the day of
admission, prior to arriving at the hospital, the patient
self-administered a single dose of morphine sulfate (MF; 20 mg
subcutaneously) and immediate-release formulation MF (30 mg
p.o.).
The initial examination conducted upon admission
revealed that the patient was conscious and coherent, of lean build
and capable of walking unaided. The patient was identified to have
a Karnofsky score of 50, an ECOG score of three and a pulse
oximeter oxygen saturation of 95%. Additional examinations revealed
impaired resonance and vesicular murmur at the base of the two
lungs, as well as tenderness of the left intra-abdomen and a
7×10-cm diameter intra-abdominal resistance, as determined by
palpation. Furthermore, the patient demonstrated signs of
peripheral neuropathy. The preceding day’s stool and flatulence
were normal, and the patient declared no allergies. Table I presents the patient’s abnormal
laboratory test results upon admission.
 | Table IAbnormalities in laboratory analyses
in the patient upon presentation. |
Table I
Abnormalities in laboratory analyses
in the patient upon presentation.
| Variable | Value (reference
value) |
|---|
| White blood cells,
10E9/l | 12.81
(4.00–10.00) |
| Hemoglobin, mM | 7.50
(7.45–10.00) |
| Hematocrit l/l | 0.37 (0.36–0.47) |
| Platelets,
10E9/l | 465.00 (130–390) |
| Serum glucose,
mM | 13.21
(3.90–5.60) |
| Serum magnesium,
mM | 0.70 (0.74–0.99) |
| γ-glutamyl
transpeptidase, U/l | 124.00 (<55) |
| Lactate
dehydrogenase, U/l | 600.00 (105–330) |
Pertinent medical history
The primary site of the cancer was the stomach,
which was diagnosed as adenocarcinoma 11 months prior to admission
to the University Hospital of Lord’s Transfiguration. Subsequently,
cancer esophageal infiltration and metastases to the lungs, liver
and lymph nodes were detected. The patient had previously undergone
a GE, splenectomy, removal of the greater and lesser omentum,
lymphadenotomy followed by chemotherapy and second-line palliative
chemotherapy. The final chemotherapy course was conducted three
months prior to admission and resulted in the side effect of
peripheral polineuropathy. Additionally, one month prior to
admission, a control esophagoduodenoscopy revealed no recurrence
within anastomosis. The patient, being aware of the diagnosis and
prognosis, asked not to be informed of the disease progress by his
wife or the medical staff.
Treatment of the patient upon admission
(day 0)
The patient was administered with fractioned rescue
doses of MF [3×2 mg, intravenously, every 5 min] and
Spasmalgon® [1 5-ml ampule (amp.) contains 2,500 mg
etamizole sodium, 0.1 mg fenpiverine bromide and 10 mg pitofenone
hydrochloride; Solpharma, Sofia, Bulgaria]. The administration of 1
amp. Intravenous (i.v.) administration of Spasmalgon caused a
decrease in pain of 75% (VRS, 3/10). Subsequently, 30 mg/24 h MF
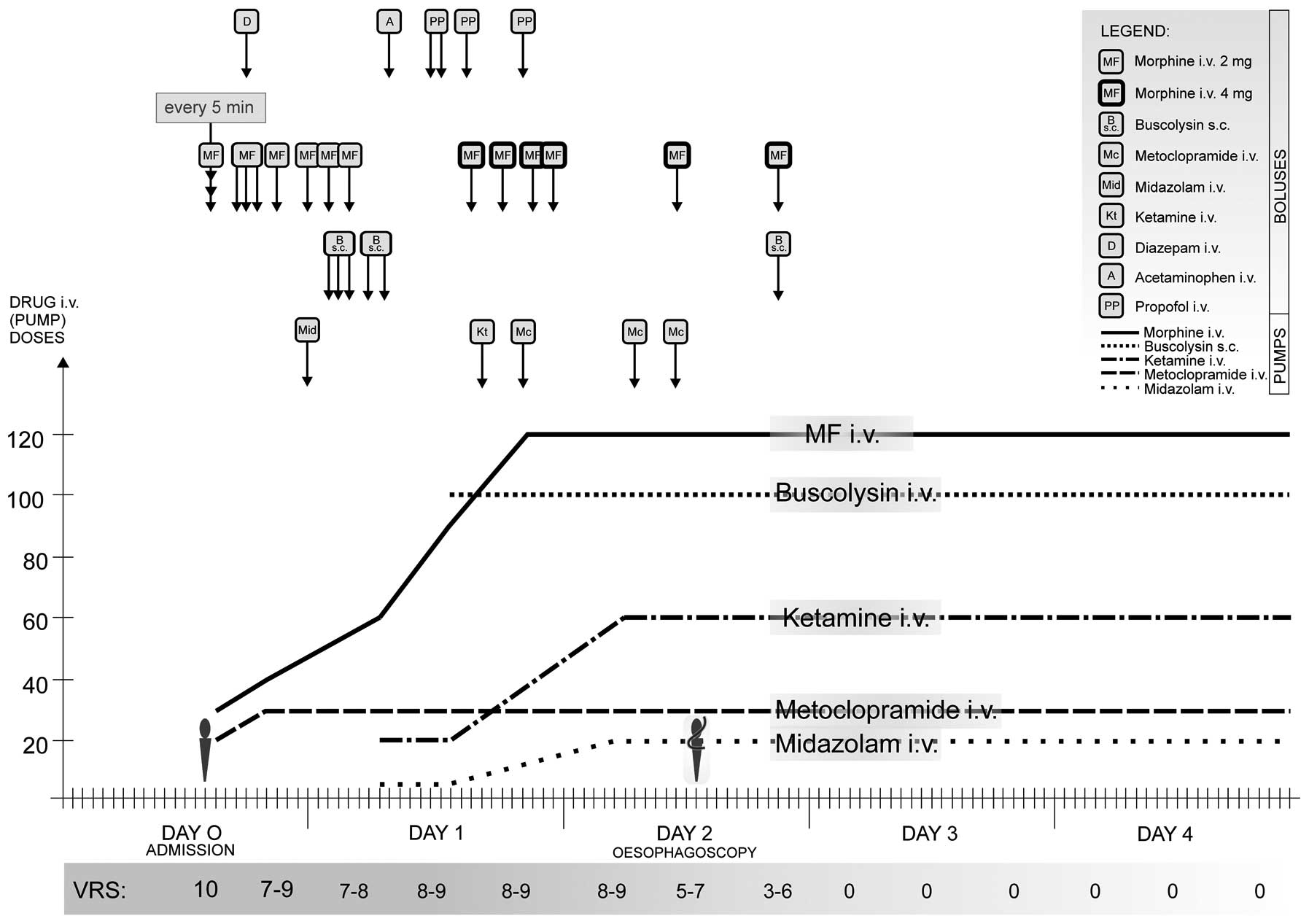
was, continuously infused, intravenously, using a pump (Fig. 1).
Symptoms, examination and treatment of
the patient during hospitalization
On day one, the patient complained of acute chest
and epigastrium pain, predominantly paroxysmal, clenching and
spasmodic, accompanied by saliva overproduction, dysphagia, nausea
and spontaneous or swallowing-induced return of undigested food.
The pain was partially refractory to MF administration (Fig. 1). As the symptoms were severe and no
malignant recurrence in the anastomosis was observed one month
prior to admission, the pain was considered to be of cardiac
origin. However, no pathological changes were detected in the
electrocardiogram examination and cardiac enzyme levels appeared
normal; therefore, acute heart muscle ischemia was excluded as a
potential diagnosis.
On day two, esophagoscopy was performed, which
considerably improved the pain control (Fig. 1). At midday, the patient was able to
walk unaided and use their laptop. The esophagoscopy revealed
masses of undigested food moving backwards in the esophagus, which
were removed by the examiner. In addition, external pressure was
identified on the esophagus. The esophagus, esophagoduodenostomy
and jejunum were difficult to assess due to semifluid food remains
(despite a previous aspiration of food masses) and small food
portions were trapped in the bronchial tree. Following the
esophagoscopy, a decompressing tube was installed in the esophagus;
due to technical reasons and patient tolerance levels, a
decompressing tube of only 5 mm in diameter was installed.
Parenteral nutrition (PN; i.v.) and antibiotics [Augmentin
(amoxicillin with clavulanic acid), 3×1.2 g/day, i.v.;
GlaxoSmithKline, Brentford, UK] were introduced as part of the
treatment strategy, due to the development of leukocytosis and
interstitial lung changes observed in examinations (Fig. 1). The decompressing tube was not
fully successful in removing food and saliva from the esophagus,
possibly due to its small diameter. However, the patient’s pain
control was sufficient to allow for further examination.
Abnormalities were detected in the echocardiogram
examination, including the presence of periaortic masses, which
moderately pressed on the left atrium, moving the descending aorta,
as was visible in the mediastinum. In addition, abnormalities were
detected in the chest computerized tomography (CT) scan, for
example sparse, interstitial densities were visible in the basal
segments of the two lungs. Abnormalities in the abdominal CT scan
included homogenous hepatomegaly (craniocaudal dimension, 20 cm),
with numerous sparse, solid, hypotensive focal lesions, which were
possibly metastatic lesions. Following splenectomy, enlarged
pockets of lymph nodes (24×26 cm; 27×19 cm) were visible in the
periaortic space between the celiac trunk and the superior
mesenteric artery.
A second esophagoscopy was recommended to clarify
the source of the pain and revealed trapped masses of liquid-pulp
consistency (of which the majority was removed), no changes in the
esophagus, esophagoenterostomy (depth, 43 cm) without pathological
changes, possible irregularities in the mucous membrane below the
Roux-en-Y anastomosis (detailed assessment impossible due to food
remains), 10 cm of intestine with no pathological changes and an
irregular mucous membrane at the end of this section. Tissue
samples were obtained and used to determine a diagnosis of
suspected intestinal cancer recurrence or infiltration to the
intestine.
On day three, the patient was able to walk unaided,
and personal computer use and pain control were satisfactory
(Fig. 1). On day four, the
decompressing tube was removed on the patient’s demand, due to the
complaint of a sore throat. However, chest and epigastrium pain
were satisfactorily controlled (Fig.
1) and intravenous feeding was introduced as an alternative.
The patient was discharged from the hospital at his request, and
received home hospice care. The patient’s condition gradually
deteriorated and the patient succumbed to the disease five days
following the in-patient unit stay.
Discussion
In the present case, the disease dynamics,
progression and symptoms were acute. Therefore, investigating the
cause of the pain was crucial for satisfactory symptom control,
particularly for pain management. Esophageal diseases and/or
dysfunctions are the most common causes of angina-like chest pain
(22), and the development of
esophageal and cardiac pains may overlap (23) and, thus, cardiac and esophageal
chest pains frequently cannot be differentiated in the case
history. Among cancer patients, ≤50% experience pain that they
perceive as moderate or severe, while 30% experience severe pain.
Furthermore, 25% of cancer patients approach mortality in pain
(24). The present case
demonstrates that diagnostic procedures are essential in the
end-of-life period. A radical improvement was observed subsequent
to esophagoscopy, due to the removal of the food masses from the
esophagus. As the patient examination conducted one month prior to
hospital admission revealed no recurrence of malignancy, the acute
chest and epigastrium pain was considered to be of cardiac origin.
However, once this source of pain was excluded, the metastases were
considered to have caused the pain. Finally, esophagitis and
esophageal wall distention were identified to be the true source of
the patient’s angina-like, spasmodic pain.
We aimed to respond to the patient’s needs, while
controlling the condition and anticipating possible drug-drug
interactions; thus, the drug doses had to be meticulously adjusted
and titrated. Calcium channel blockers and nitrates were excluded
from the treatment strategy of the present patient due to the
patient experiencing problems swallowing calcium channel blocker
pills and having a blood pressure too low for nitroglycerin
administration (i.v. or in aerosol), respectively, as well as
unwanted effects (dizziness due to hypertension, headache and
flushing). The treatment required a balance between controlling the
symptoms and maintaining therapeutic safety. The patient was
provided with an optimal quality of life.
In the conclusion, the present study determined that
a cancer patient in palliative care, approaching mortality, may
require a secondary diagnosis to provide an appropriate quality of
life and preserve the patient’s dignity. Additionally, pain
treatment should be adjusted according to anatomical,
pathophysiological and pharmacological factors. In the present
case, the treatment of acute epigastric and chest pain originating
from cancer was posed risks due to the parenteral co-administration
of multiple strong-acting agents, however, the therapy was
unavoidable. Careful drug titration and treatment monitoring is,
therefore, essential for the safe administration of multidrug pain
control. It was also concluded that a patient exhibiting
regurgitation of food and experiencing severe pain requires
constant monitoring and nursing care, for example due to the risk
of developing aspiration pneumonia. For the present patient,
esophagoduodenoscopy proved to be both diagnostic and therapeuticas
it allowed for emptying the esophagus and satisfactory pain
control. The second esophagoduodenoscopy was also diagnostic as it
revealed changes accounting for intestinal cancer recurrence or
infiltration to intestine.
References
|
1
|
World Health Organisation. Cancer Pain
Relief. Second Edition. World Health Organisationl; Geneva: 1996,
Available from: http://whqlibdoc.who.int/publications/9241544821.pdf.
Accessed March 9, 2014
|
|
2
|
Baldi F and Ferrarini F: Non-cardiac chest
pain: a real clinical problem. Eur J gastroenterol Hepatol.
7:1136–1140. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fass R and Dickman R: Non-cardiac chest
pain: an update. Neurogastroenterol Motil. 18:408–417. 2006.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Rao SS: Diagnosis and management of
esophageal chest pain. Gastroenterol Hepatol (NY). 7:50–52.
2011.
|
|
5
|
Hong SJ: Diagnosis and management of
esophageal chest pain. Korean J Gastroenterol. 55:217–224. 2010.(In
Korean). View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Noffsinger AE: Update on esophagitis:
controversial and underdiagnosed causes. Arch Pathol Lab Med.
133:1087–1095. 2009.PubMed/NCBI
|
|
7
|
Lemire S: Assesement of clinical severity
and investigation of uncomplication gastresophageal reflux disease
and non-cardiac angina-like chest pain. Can J Gastroenterol.
11(Suppl B): 37B–40B. 1997.
|
|
8
|
Hershcovici T, Achem SR, Jha LK and Fass
R: Systematic review: the treatment of non-cardiac chest pain.
Aliment Pharmacol Ther. 35:5–14. 2012. View Article : Google Scholar
|
|
9
|
Fass R and Navarro-Rodriguez T: Noncardiac
chest pain. J Clin Gastroenterol. 42:636–646. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Cannon RO III, Quyyumi AA, Mincemoyer R,
et al: Imipramine in patients with chest pain despite normal
coronary angiograms. N Engl J Med. 330:1411–1417. 1994. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Remes-Troche JM, Chahal P, Mudipalli R and
Rao SS: Adenosine modulates esophageal sensorimotor functions in
humans. Gut. 58:1049–1055. 2009. View Article : Google Scholar
|
|
12
|
Rao SS, Mudipalli RS, Remes-Troche JM,
Utech CL and Zimmerman B: Theophylline improves esophageal chest
pain - a randomized, placebo-controlled study. Am J Gastroenterol.
102:930–938. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Drenth JP, Bos LP and Engels LG: Efficacy
of diltiazem in the treatment of diffuse esophageal spasm. Aliment
Pharmacol Ther. 4:411–416. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Swamy N: Esophageal spasm: clinical and
manometric response to nitroglycerine and long acting nitrites.
Gastroenterology. 72:23–27. 1977.PubMed/NCBI
|
|
15
|
Azpiroz F and Malagelada JR: Gastric tone
measured by an electronic barostat in health and postsurgical
gastroparesis. Gastroenterology. 92:934–943. 1987.PubMed/NCBI
|
|
16
|
Rivera I, Ochoa-Martinez CI,
Hermosillo-Sandoval JM, et al: Dumping syndrome in patients
submitted to gastric resection. Cir Cir. 75:429–434. 2007.(In
Spanish).
|
|
17
|
Spiller R: Role of motility in chronic
diarrhoea. Neurogastroenterol Motil. 18:1045–1055. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hinshaw DB, Joergerson EJ, Davis HA and
Stafford CE: Peripheral blood flow and blood volume studies in the
dumping syndrome. AMA Arch Surg. 74:686–693. 1957. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Ukleja A: Dumping syndrome:
pathophysiology and treatment. Nutr Clin Pract. 20:517–525. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Deitel M: The change in the dumping
syndrome concept. Obes Surg. 18:1622–1624. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Likert R: A technique for the measurement
of attitudes. Arch Psych. 140:1–55. 1932.
|
|
22
|
Fass R, Malagon I and Schmulson M: Chest
pain of esophageal origin. Curr Opin Gastroenterol. 17:376–380.
2001. View Article : Google Scholar
|
|
23
|
Mellow MH, Simpson AG, Watt L,
Schoolmeester L and Haye OL: Esophageal acid perfusion in coronary
artery disease. Induction of myocardial ischemia. Gastroenterology.
85:306–312. 1983.PubMed/NCBI
|
|
24
|
Saunders CM: The challenge of terminal
care. Scientific Foundations of Oncology. Symington T and Carter
RL: Heinemann; London: pp. 673–679. 1976
|