Introduction
Lymphedema is the chronic and progressive
engorgement of tissues caused by deficient lymphatic drainage
(1). Vulvar lymphedema is one of
the most disabling side-effects of treatment for gynecological
cancers involving systematic pelvic, or pelvic and aortic, lymph
node dissection associated with adjuvant or neoadjuvant radiation
therapy (1). Lymphorrhea may occur
as a complication of lymphedema (1,2). The
incidence of genital lymphedema is unknown, as it is frequently
undiagnosed (2). As with other
types of lymphedema, the condition typically occurs in the first
three to four years after cancer treatment, however, it may develop
up to 30 years later (1). Genital
lymphedema is typically combined with lower limb lymphedema;
systematic pelvic lymph node dissection damages the lower limb
lymphatic system, leading to a reduced capacity to absorb excess
water and cells from the interstitial space (2). Treatment using compressive pump (or
bandaging) therapy may subsequently lead to an increase in vulvar
lymphatic load, followed by the appearance of dilated lymphatic
vessels and vulvar lymphedema. In addition to skin alterations, a
significant symptom is lymphorrhea, which occurs following
increases in tissue pressure, causing fluid to leak from the thin
layer of skin. Furthermore, edematous skin is an ideal medium for
bacteria and can lead to a high risk of developing skin infections,
particularly erysipelas (3).
Lymphorrhea may be extremely distressing for patients due to the
requirement to wear sanitary towels, and as the pain and loss of
elasticity of the vulvar skin and mucosa can make coitus
uncomfortable, with altered vulvar/vaginal sensation (4).
Few previous studies have been published with regard
to the management of vulvar lymphorrhea and lymphedema secondary to
radical treatment for gynecological cancer. The current study
reports two cases involving the development of late symptoms of
vulvar lymphedema in females who had previously undergone treatment
for gynecological cancers. The condition was refractory to standard
therapies in these cases and thus, laser CO2 surgery was
performed. Laser CO2 surgery is a technique used for the
excisional conservative treatment of preinvasive and initially
invasive neoplasia of the lower female genital tract (5). In the current study, this surgical
technique acted to induce a coagulative sclerosis in order to
obliterate the subcutaneous and submucosal lymphatic channels, and
create a fibrous layer capable of preventing the lymphorrhea.
Written informed consent was obtained from both patients.
Case report
Case one
In 1986, a 29-year-old female underwent a Piver type
III radical hysterectomy, systematic pelvic lymphadenectomy,
adjuvant pelvic radiotherapy (50.60 Gy) and vaginal brachitherapy
(20.34 Gy) for the treatment of International Federation of
Gynecology and Obstetrics (FIGO) stage IB1 pN1 cervical cancer
(6). At six months post-treatment,
bilateral lower-limb lymphedema developed. Lymph drainage and
elastic bandaging were performed with limited efficacy. In 1988,
the patient experienced difficulties due to chronic lower-limb
lymphedema.
In 2003, a painful vulvar edema developed, followed
by vulvar lymphorrhea. In 2004, the patient was referred to the
Department of Gynecological Oncology of the Aviano National Cancer
Institute (Pordenone, Italy), due to a worsening in vulvar pain,
classified as a score of 9 according to the Visual Analog Scale
(VAS) for pain evaluation (7). The
patient reported a dragging, heavy and bursting sensation,
resulting in the loss of sexual function and difficulties in
urination, with no evidence of urinary infection.
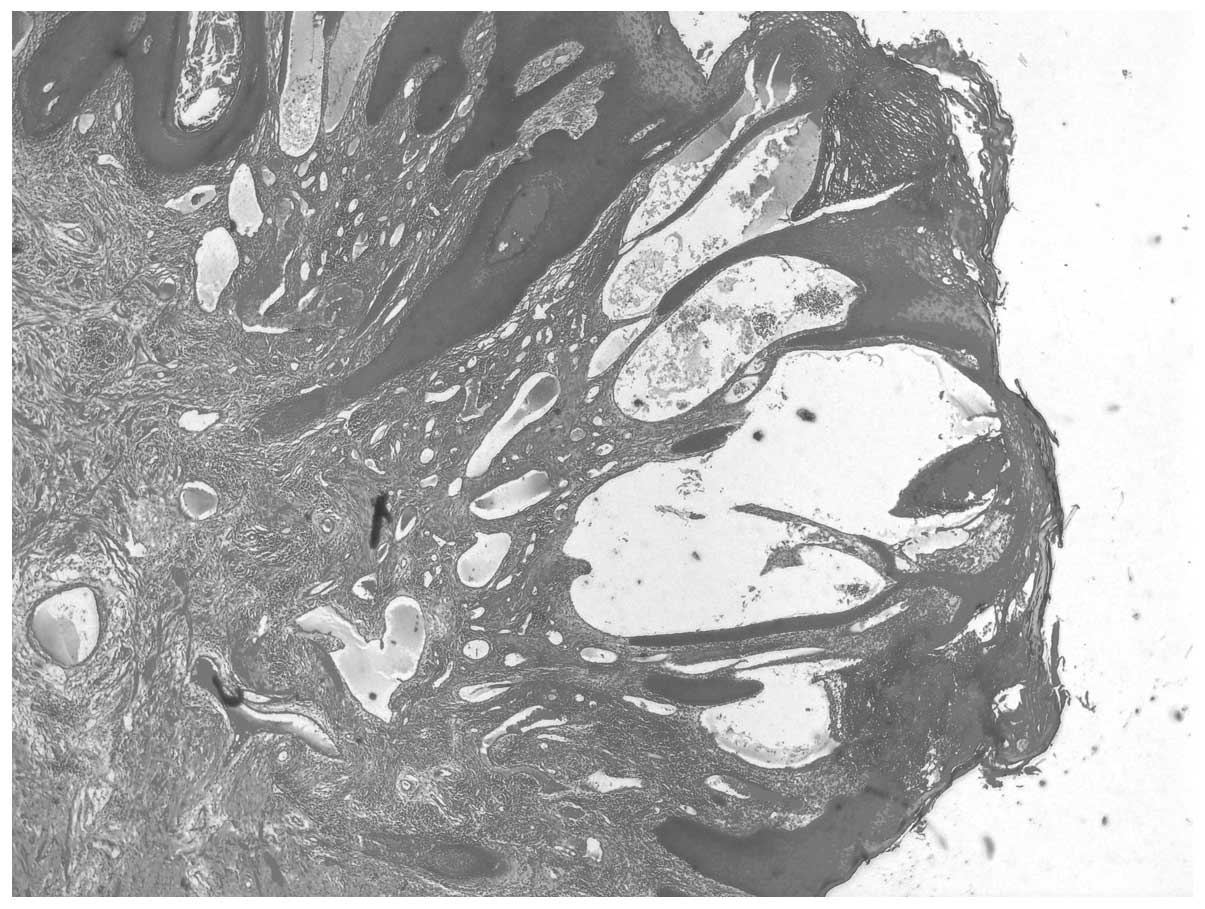
A vulvar examination revealed swollen inner and
outer labia and vulvar edema, with associated fibrosis and skin
changes, including thickening, dryness and hyperkeratosis. A vulvar
specimen measuring 2.0×0.7×0.2 cm was excised, and a clinical
diagnosis of vulvar lymphedema was confirmed by histological
examination of the lesion, which revealed acanthosis, multiple
dilated lymph vessels lined by a single layer of endothelium in the
upper dermis, downward growth of the epidermis, a lymphoplasmacytic
inflammatory infiltrate and an absence of giant or atypical cells
(Fig. 1). Computed tomography and
ultrasound scans of the abdomen were conducted, revealing no
evidence of associated lymphoceles or recurrence of pelvic or
retroperitoneal disease.
Vulvar excisional and vaporization treatment was
performed in four sessions using a colposcopy-guided CO2
laser, with a constant emission power of 20 W/cm2 and a
beam diameter of <0.2 and 0.5–1 mm for resection and
vaporization, respectively, under local anesthesia with 2%
mepivacaine. Excisional treatment was performed to obtain
additional specimens in order to further investigate potential
concurrent causes of vulvar edema. The depth of
excision/vaporization was 0.3 cm, up to the sub-epithelial tissue.
The procedures were performed as day surgery without antibiotic
prophylaxis, and no complications occurred. Following recovery from
the treatment, the patient experienced relief from the
aforementioned pain and heaviness, subsequent to the resolution of
the lymphorrhea. A pain assessment was performed every six months
during follow-up gynecological examinations, with VAS scores
(7) ranging from 0–2. A vulvar
biopsy performed six months after vaporization treatment revealed
multiple dilated lymph vessels without edema. The patient
experienced a recurrence of vulvar lymphorrhea seven years after
the treatment, which was again treated by laser CO2
vaporization, as previously described, resulting in a reduction of
the persistent symptoms.
Case two
In 1997, a 49-year-old female underwent a Piver type
III radical hysterectomy with systematic pelvic lymphadenectomy and
adjuvant pelvic radiotherapy (45 Gy) for the treatment of FIGO
stage II, pN0, G3 endometrial adenocarcinoma (6).
Beginning in 2002, the patient suffered with
recurrent vulvar erysipelas and chronic vulvar edema, secondary to
lower-limb lymphedema, which was partially treated by combined
decongestive therapy consisting of compressive bandaging and manual
lymph drainage.
In 2012, the patient was referred to the Department
of Gynecological Oncology of Aviano National Cancer Institute due
to gradually increasing swelling of the vulva over a period of six
months, associated with a genital pain score of 4–5 according to a
VAS evaluation (7); the symptoms
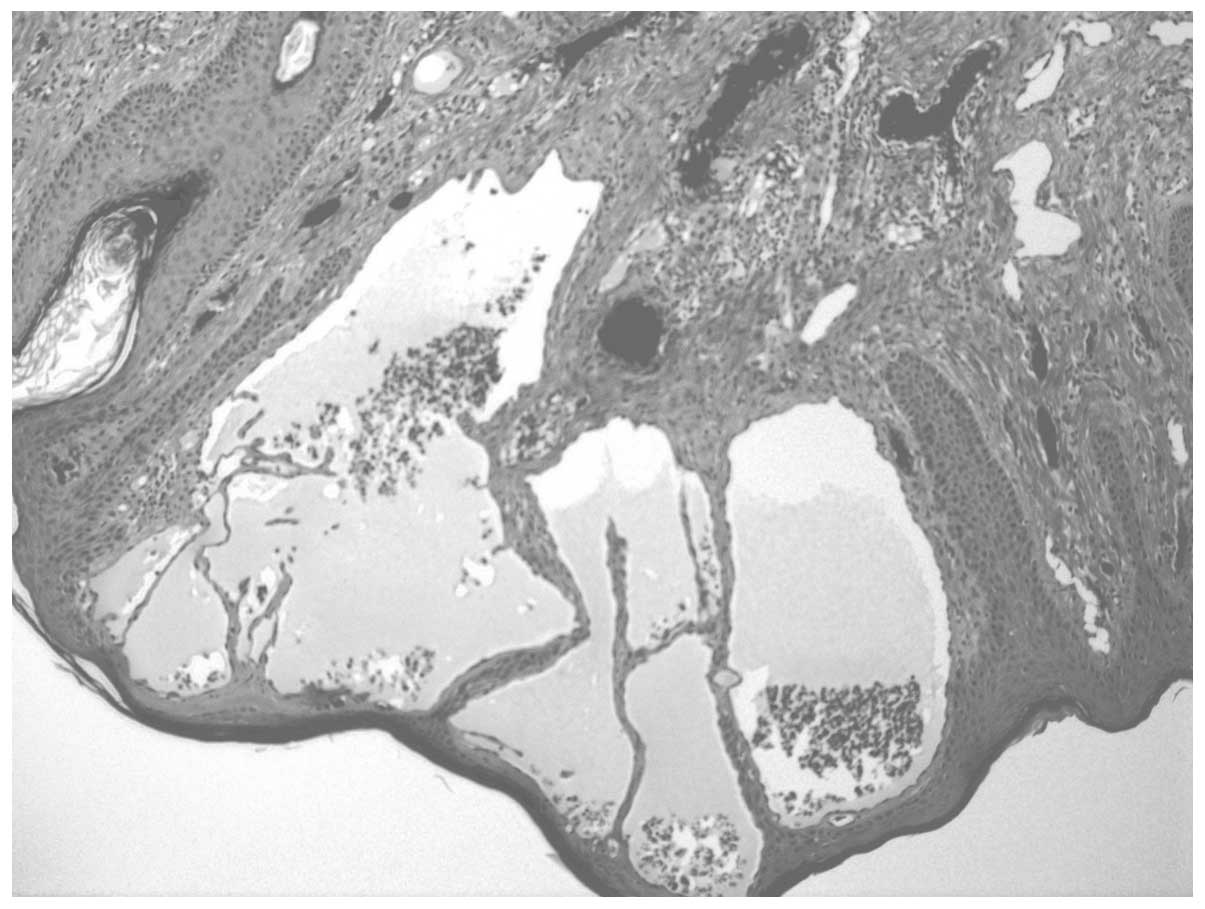
prohibited regular physical and sexual activity. A gynecological
examination revealed multiple, firm, hyperkeratotic glossy papules
and swelling of the vulva associated with changes in skin texture
and leakage of serous fluid through the skin (lymphorrhea). A
vulvar biopsy measuring 1.0×0.8×0.3 cm was used to determine a
diagnosis of vulvar lymphedema (Fig.
2). As the standard treatments for lower-limb lymphedema were
ineffective in improving the vulvar symptoms, vulvar excisional and
vaporization treatments (three sessions) were performed using
colposcopy-guided laser CO2 (as described in case one).
Due to the patient’s history of erysipelas, a three-day regimen of
the antibiotic azithromycin (500 mg/day) was administered. No
complications were experienced, and the symptoms of pain and
heaviness were relieved following reduction of the edema. During
the 24-month follow-up examination, the patient presented with mild
vulvar lymphedema without symptoms (VAS score, 0) and without
lymphorrhea.
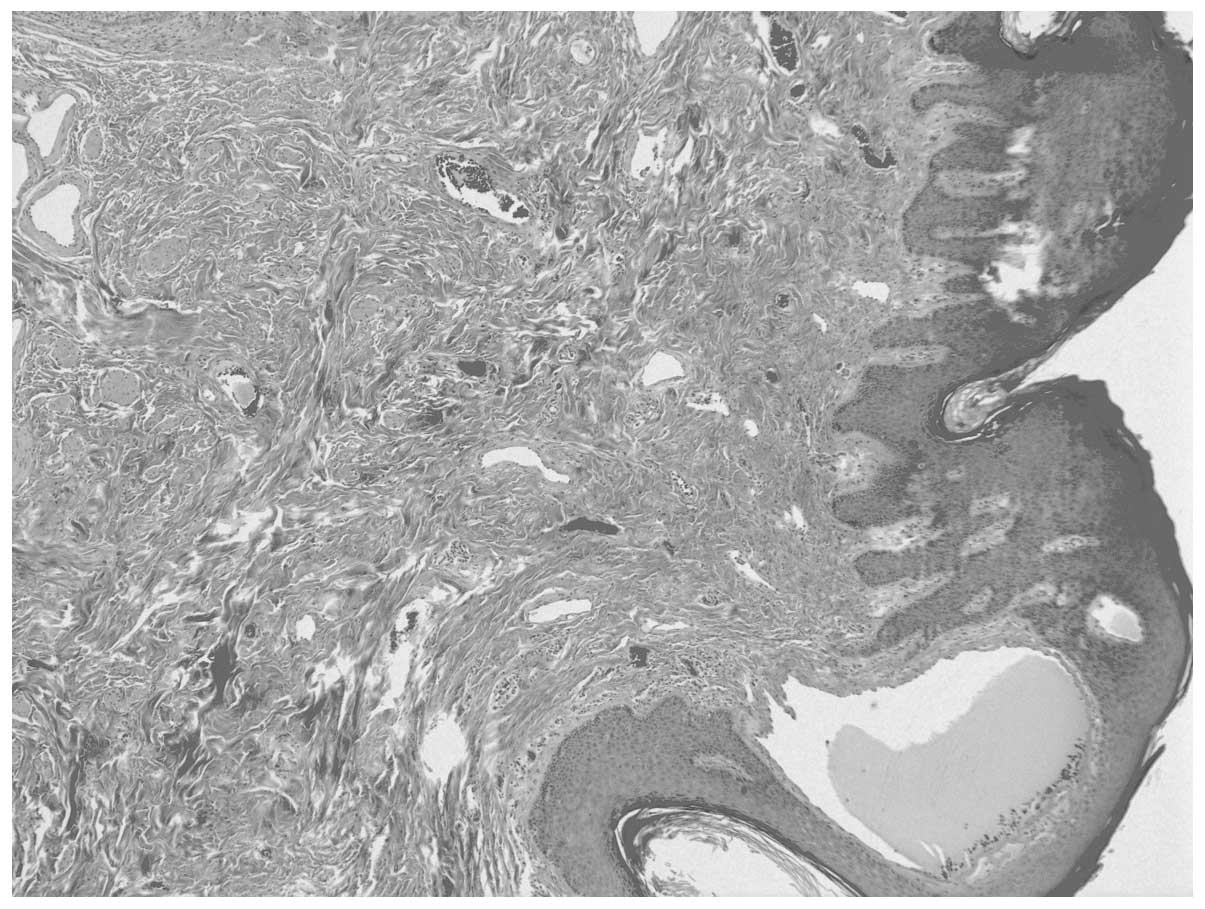
A biopsy performed in 2013 revealed a reduction in
the dilatation of the dermal vessels, associated with moderate
fibrosis (Fig. 3).
Discussion
Lymphedema is a chronic and frequently incurable
condition that may occur following therapeutic interventions
affecting lymphatic drainage mechanisms, such as the surgical
treatment of cancer (8).
Histological examination may be used to determine the diagnosis of
lymphedema, which is characterized by dilated and tortuous
lymphatic vessels lined by a single layer of flat endothelial
cells. Secondary changes (primarily atrophic) are typically
observable in the overlying epidermis, in addition to inflammatory
infiltrates, with slight fibrosis of the dermis. A number of
histological features of vulvar lymphedema may mimic aggressive
angiomyxoma; therefore this differential diagnosis must be
considered, along with other myxedematous tumors of the
vulvovaginal region (9). Vulvar
lymphedema is typically secondary to lower limb lymphedema,
following lymphadenectomy for the treatment of gynecological cancer
(2). Although lower limb lymphedema
has been extensively investigated, few studies are available with
regard to vulvar lymphedema. Lymphedema of the female external
genitalia following lymphadenectomy may be initially asymptomatic,
or characterized by minimal symptoms that are often not reported by
the patient. Later, the condition may severely impair the quality
of life of affected patients, inducing aesthetic alteration and,
particularly when associated with lymphorrhea, causing discomfort
and pain during walking, sexual activity or when lying down, as
well as recurrent erysipelas (3,4).
Lymphatic physiopathology is poorly understood; it
has been hypothesized that the combination of surgery and adjuvant
treatment may lead to fibrosis, with a subsequent obliteration of
the lymphatic vessels and failure of lymph drainage, resulting in
chronic and progressive tissue engorgement (10). This condition is exacerbated by
lower-limb lymphedema as a consequence of a prior defect in lymph
drainage. The proper management of lymphedema involves patient
education to detect symptoms that are indicative of early disease
onset, including heaviness, skin tightness, aching, numbness,
weakness, impaired limb function or pain; no definitive effective
therapy has been determined, and there are few studies available
with regard to the treatment of female genital lymphedema and
vulvar lymphorrhea (1).
A number of surgical approaches for the treatment of
limb lymphedema refractory to conservative decongestive methods
have been proposed. Lymphaticovenular anastomosis using an
autologous interposition vein graft has been reported to be
effective, simple to perform and minimally invasive for the
treatment of secondary lymphedema of the upper and lower
extremities (11). This
supermicrosurgery technique facilitates bypassing the region of
lymph flow obstruction, providing an alternative route for
lymphatic fluid recirculation into the venous system through
multiple lymphatic-venous or lymphatic-venous-lymphatic anastomoses
(11,12).
Autologous or heterologous transplantation of
vascularized lymph nodes has also been proposed (11); this tissue may prevent
retroperitoneal fibrosis following lymphadenectomy, and allows
neuromatous structure reconstitution, with pain relief. The nodes
appear to survive well, and establish connections with locally
situated lymph vessels, which assists in lymphatic return if the
vasculature is microsurgically connected (13). Microsurgery and reconstructive
surgery have also been proposed to treat lymphedema of the external
male genitalia, a frequent complication of pelvic radical surgery
following pelvic lymphadenectomy (14,15).
Lymphangiography has been demonstrated to be a
valuable tool in the treatment of lymphedema, and acts to induce an
inflammatory reaction that closes the leak (16). One previous study reported three
cases of groin nodal ultrasound-guided lymphangiography for the
diagnosis and treatment of genital lymphedema (16). Transnodal Lipiodol injection
facilitates the visualization of nodal and lymphatic vessels. It
has been hypothesized that Lipiodol accumulation at the leak point
may cause an inflammatory reaction, leading to fibrosis and
elimination of the leak (16).
In the current cases, it was not possible to treat
the mechanisms causing the failure of lymph drainage, therefore,
the selected therapies focused on the peripheral manifestation of
the pathological process, treating the lymphorrhea. Dioxide light
amplification by the stimulated emission of radiation
(CO2 laser) was selected, as it is a safe, minimally
invasive and repeatable technique, which acts to induce coagulative
sclerosis in order to obliterate the subcutaneous and submucosal
lymphatic channels, and create a fibrous layer capable of
preventing lymphorrhea. Following therapy, a marked reduction in
lymphangiectasia associated with increased dermal fibrosis was
observed (Fig. 3). This treatment
resulted in a decrease in lymphorrhea and pain. The relief of pain
may be a consequence of decreased lymphorrhea and damage to the
nerve endings near to the treated areas. In the current case,
long-term advantages were observed in the two patients, for whom
previous lymph drainage and elastic bandaging treatments had been
unsuccessful. Quality of life was improved in the patients by
reducing the disabling effects of lymphorrhea and its
complications; the treatment eliminated the requirement to wear
sanitary pads daily, and each patient was able to have sexual
intercourse due to the relief from pain. In addition, the second
patient experienced no further erysipelas.
Surgical treatment of vulvar lymphorrhea and
lymphedema secondary to gynecological cancer treatments remains
controversial, and is not currently accepted as standard therapy.
The current study utilized laser surgery, a minimally invasive
surgical approach to this pathology, which resulted in effective
symptomatic treatment. Although this therapy may not be regarded as
definitive, as the underlying mechanisms causing the clinical
manifestation of lymphedema are not treated, it may provide a
valuable long-term treatment strategy. In the present study, the
first patient presented with a recurrence of vulvar lymphedema and
associated lymphorrhea seven years after the initial laser
CO2 treatment, and as the treatment is repeatable,
further laser CO2 surgery could be successfully
performed. Therefore, laser CO2 surgery has the
advantage of being a repeatable technique, which at present has not
been reported to have any side effects. The present study indicated
that laser CO2 surgery is a successful treatment for
lymphorrhea, a complication of vulvar lymphedema, however, further
studies are required to confirm these findings, using a larger
number of patients.
References
|
1
|
Beesley V, Janda M, Eakin E, Obermair A
and Battistutta D: Lymphedema after gynecological cancer treatment:
Prevalence, correlates, and supportive care needs. Cancer.
109:2607–2614. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Rockson SG: Lymphedema. Am J Med.
110:288–295. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Zvonik M, Földi E and Felmerer G: The
effects of reduction operation with genital lymphedema on the
frequency of erysipelas and the quality of life. Lymphology.
44:121–130. 2011.PubMed/NCBI
|
|
4
|
Barton DP: The prevention and management
of treatment related morbidity in vulval cancer. Best Pract Res
Clin Obstet Gynaecol. 17:683–701. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Adelman MR, Tsai LJ, Tangchitnob EP and
Kahn BS: Laser technology and applications in gynaecology. J Obstet
Gynaecol. 33:225–231. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Pecorelli S: Revised FIGO staging for
carcinoma of the vulva, cervix, and endometrium. Int J Gynaecol
Obstet. 105:103–104. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kliger M, Stahl S, Haddad M, Suzan E,
Adler R and Eisenberg E: Measuring the Intensity of Chronic Pain:
Are the Visual Analogue Scale and the Verbal Rating Scale
Interchangeable. Pain Pract. Apr 16–2014.(Epub ahead of print).
View Article : Google Scholar
|
|
8
|
Newman ML, Brennan M and Passik S:
Lymphedema complicated by pain and psychological distress: A case
with complex treatment needs. J Pain Symptom Manage. 12:376–379.
1996. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Vang R, Connelly JH, Hammill HA and
Shannon RL: Vulvar hypertrophy with lymphedema. A mimicker of
aggressive angiomyxoma. Arch Pathol Lab Med. 124:1697–1699.
2000.PubMed/NCBI
|
|
10
|
Gothard L, Stanton A, MacLaren J, et al:
Non-randomised phase II trial of hyperbaric oxygen therapy in
patients with chronic arm lymphoedema and tissue fibrosis after
radiotherapy for early breast cancer. Radiother Oncol. 70:217–224.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Todokoro T, Furniss D, Oda K, Kawana K,
Narushima M, Mihara M, Kikuchi K, Hara H, Yano T and Koshima I:
Effective treatment of pelvic lymphocele by lymphaticovenular
anastomosis. Gynecol Oncol. 128:209–214. 2013. View Article : Google Scholar
|
|
12
|
Mihara M, Hara H, Kikuchi K, et al:
Scarless lymphatic venous anastomosis for latent and early-stage
lymphoedema using indocyanine green lymphography and non-invasive
instruments for visualising subcutaneous vein. J Plast Reconstr
Aesthet Surg. 65:1551–1558. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Felmerer G, Sattler T, Lohrmann C and
Tobbia D: Treatment of various secondary lymphedemas by
microsurgical lymph vessel transplantation. Microsurgery.
32:171–177. 2012. View Article : Google Scholar
|
|
14
|
Mukenge SM, Catena M, Negrini D, Ratti F,
Moriondo A, Briganti A, Rigatti P, Cipriani F and Ferla G:
Assessment and follow-up of patency after lymphovenous microsurgery
for treatment of secondary lymphedema in external male genital
organs. Eur Urol. 60:1114–1119. 2011. View Article : Google Scholar
|
|
15
|
Baumeister RG, Siuda S, Bohmert H and
Moser E: A microsurgical method for reconstruction of interrupted
lymphatic pathways: Autologous lymph-vessel transplantation for
treatment of lymphedemas. Scand J Plast Reconstr Surg. 20:141–146.
1986. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gómez FM, Martínez-Rodrigo J,
Martí-Bonmatí L, Santos E, Forner I, Lloret M, Pérez-Enguix D and
García-Marcos R: Transnodal lymphangiography in the diagnosis and
treatment of genital lymphedema. Cardiovasc Intervent Radiol.
35:1488–1491. 2012. View Article : Google Scholar : PubMed/NCBI
|