Introduction
Non-small cell lung cancer (NSCLC) accounts for ∼85%
of all lung cancers, worldwide (1).
In total, ∼40% of newly diagnosed NSCLC cases are classified as
stage-IV disease, with distant metastasis already present. However,
even in patients with early-stage disease, the recurrence rate is
high. Metastasis to any organ in the body may occur, but the
adrenal glands, liver, brain and bones are the most common sites
(2). Pancreatic involvement secondary
to lung cancer is not uncommon (3–5), however,
metastasis of tumors to the pancreas rarely becomes clinically
evident, and is usually incidentally identified during abdominal
imaging in the follow-up period. Gastrointestinal (GI) bleeding as
a clinical presentation of the pancreatic metastasis of lung cancer
has rarely been reported (6).
In the present study, two cases of lung cancer
metastasis to the pancreas that presented with upper GI bleeding
are reported. To the best of our knowledge, this is the second
study concerning GI bleeding caused by the pancreatic metastasis of
lung cancer. The present study may increase the awareness of GI
hemorrhage as a manifestation of this relatively rare condition.
This study was approved by the Ethics Committee of The First
Affiliated Hospital of Zhejiang University. Written informed
consent was obtained from the patients' family for both
patients.
Case report
Case one
In June 2013, a 56-year-old male was diagnosed with
right upper lung adenocarcinoma [pT2aN0M0; stage IB, according to
the American Joint Committee on Cancer (AJCC) TNM staging system
(7)] and underwent thoracoscopic
lobectomy at The First Affiliated Hospital of Zhejiang University
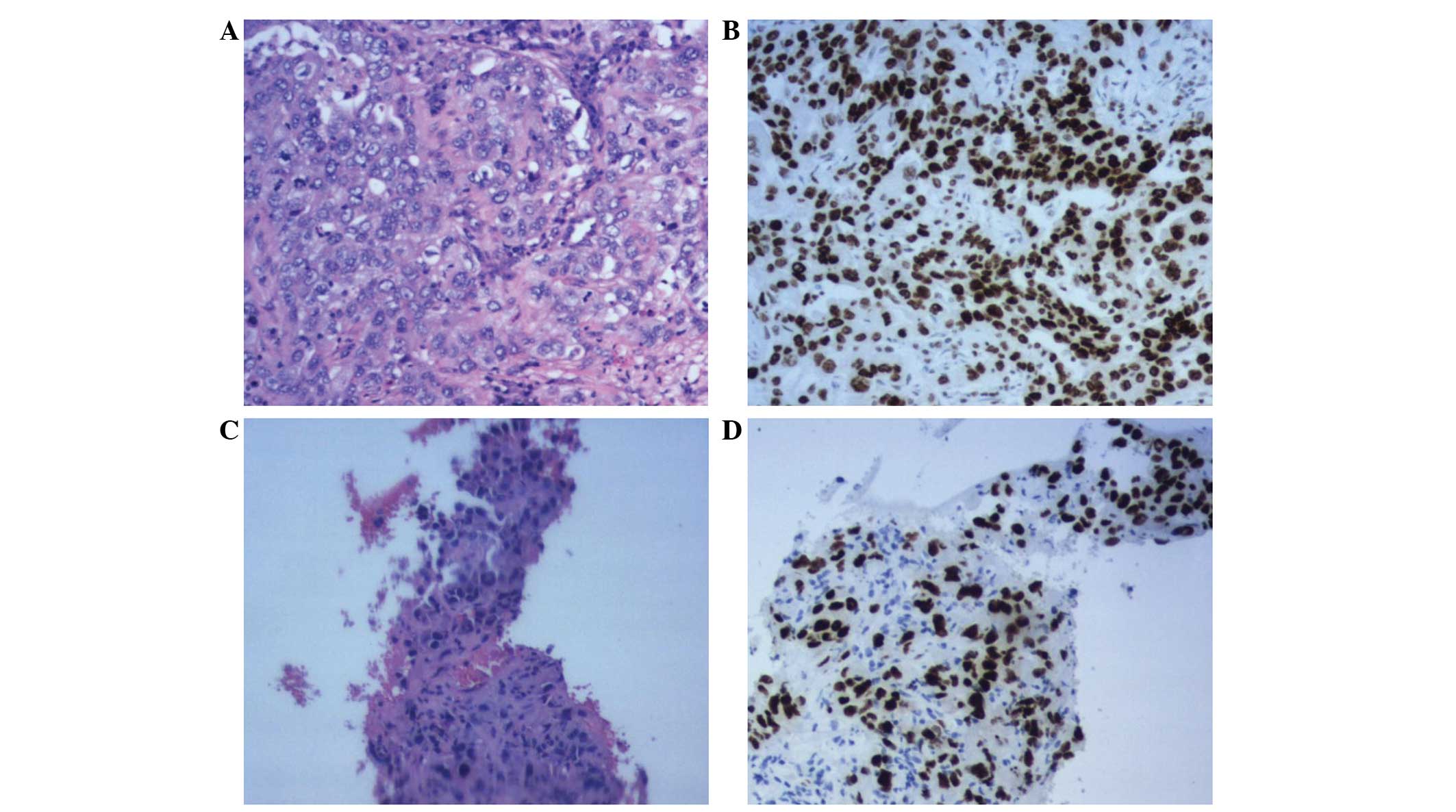
(Hangzhou, China). Pathological examination revealed high-grade
adenocarcinoma (Fig. 1A), with clear
surgical margins and negative lymph nodes. Immunostaining revealed
positivity for thyroid transcription factor-1 (TTF-1) (Fig. 1B) and cytokeratin (CK)7, and
negativity for p63 and CK5/6. No evidence of distant metastasis was
detected. The patient was treated with adjuvant chemotherapy using
a platinum-based combined regimen, which was administered at
another hospital.
The patient presented again to The First Affiliated
Hospital of Zhejiang University four months later (October, 2013)
with melena, epigastric pain and weight loss of 5 kg. The patient
had no history of pulmonary distress or dizziness, and the medical
history was unremarkable, with no additional smoking history. The
patient's performance status was 1, according to The Eastern
Cooperative Oncology Group (8). A
physical examination revealed anemia and upper abdominal
tenderness. The patient's blood pressure was 137/83 mmHg and the
pulse rate was 76 beats per minute (bpm). Laboratory tests revealed
the following: Red blood cell (RBC) count, 2.58×1012/l
(normal range, 3.68–5.13×1012/l); hemoglobin
concentration, 56 g/l (normal range, 114–151 g/l); hematocrit,
19.7% (normal range, 33.5–45.0%). White blood cell (WBC) count
(5.9×109/l), platelet count (304×109/l),
blood urea nitrogen (BUN) levels (5.7 mmol/l) and creatinine (Cr)
levels (68 µmol/l) were all normal. Furthermore, the serum alanine
aminotransferase (ALT; 103 U/l; normal range, 5–40 U/l), serum
aspartate aminotransferase (AST; 61 U/l; normal range, 8–40 IU/l),
serum γ-glutamyl transpeptidase (γ-GT; 508 U/l; normal range, 11–50
IU/l) and serum alkaline phosphatase (AKP; 320 U/l; normal range,
40–150 U/l) levels were elevated. In addition, the general
bilirubin (40 µmol/l; normal range, 9–21 µmol/l), direct bilirubin
(22 µmol/l; normal range, 0–5 µmol/l) and total bile acid (41 µmol;
normal range, 1–12 µmol/l) levels were elevated. Tumor markers,
including α-fetoprotein (α-FP), carcinoembryonic antigen (CEA),
carcinoma antigen (CA)19-9, CA-125 and prostate-specific antigen
(PSA) were all within normal limits. Coagulation tests were also
normal. In addition, the fecal occult blood test was strongly
positive.
GI bleeding and obstructive jaundice was suspected.
A small bowel endoscopy revealed a large amount of blood in the
upper jejunum, however, no active bleeding sites were identified.
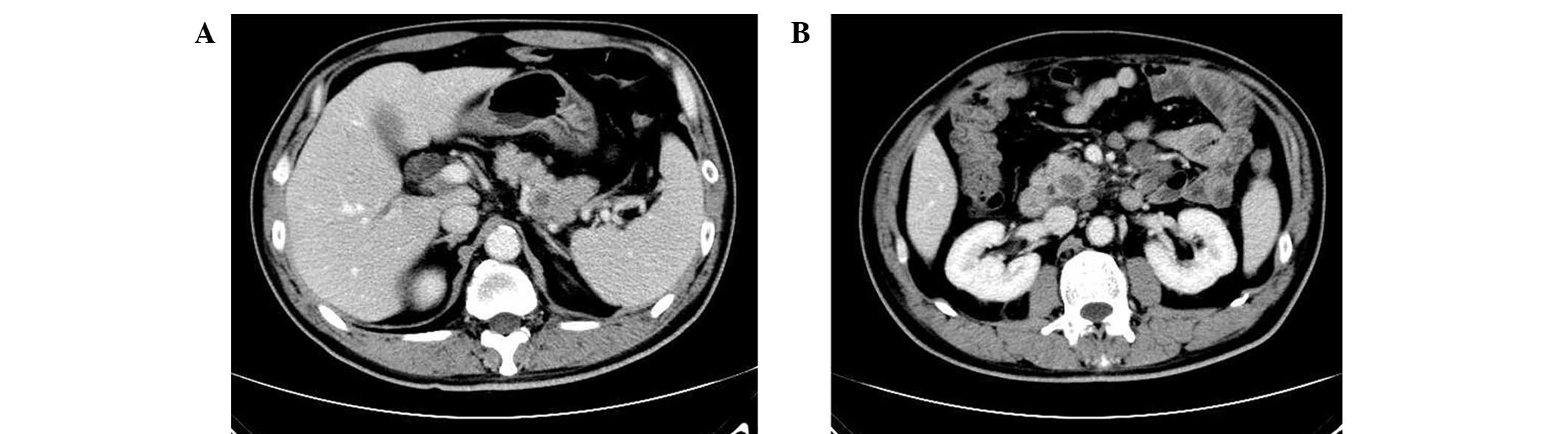
Abdominal contrast-enhanced computed tomography (CT) revealed
multiple lesions in the pancreas (Fig.
2A and B), and distention of the intra- and extrabiliary ducts.
Enlarged peripancreatic lymph nodes were also detected. A
subsequent endoscopic retrograde cholangiopancreatography revealed
stenosis of the distal common bile duct and thus, a plastic stent
was inserted into the common bile duct. A week after the insertion
procedure, the AST, ALT, AKP, γ-GT, bilirubin and total bile acid
levels were normal. However, the patient's WBC count was elevated
to 20.5×109/l and the hemoglobin level was 68 g/l, even
after multiple RBC blood transfusions.
In October 2013, ultrasonography-guided biopsy of
one lesion surrounding the pancreas confirmed a diagnosis of
adenocarcinoma (Fig. 1C), and the
immunohistochemistry results were consistent with primary lung
cancer [TTF-1+ (Fig. 1D),
CK7+, p63−, CK5− and
CK6−]. The epidermal growth factor receptor (EGFR)
mutation test revealed no mutation of the tumor. The diagnosis of
lung adenocarcinoma with metastasis to the pancreas was confirmed.
As the tumor was not resectable, surgeons recommended conservative
treatment. The patient survived for six months following the
resection of the primary lung cancer and six weeks after the
diagnosis of metastatic pancreatic cancer from NSCLC. However, in
December 2013, the patient succumbed to respiratory failure.
Case two
In July 2013, a 63-year-old male presented to The
First Affiliated Hospital of Zhejiang University, with melena and
weight loss of 2 kg over a two-month period. The patient had no
history of smoking. In May 2010, the patient was diagnosed with
early-stage lung adenocarcinoma and subsequently underwent right
upper lung lobectomy via a thoracotomy. The patient received no
adjuvant chemotherapy or radiotherapy. In July 2011, a craniotomy
was performed for the resection of a solitary brain metastasis from
NSCLC. No detailed medical data is available for the two surgical
procedures, as they were performed at another hospital.
The patient was referred to the Hepatobiliary and
Pancreatic Unit of The First Affiliated Hospital of Zhejiang
University (July, 2013). Upon physical examination, the patient was
pale with no apparent pulmonary distress or dizziness. Epigastric
tenderness was noted and a stool sample was found to be strongly
positive in a fecal occult blood test. The patient's blood pressure
was 99/54 mmHg, with a pulse rate of 87 bpm. Laboratory
examinations revealed a blood hemoglobin level of 66 g/l and a
hematocrit level of 21.6%. Other tests, including ALT, AST, AKP,
γ-GT, bilirubin, total bile acid, BUN, Cr, WBC count, platelet,
CEA, α-FP, CA19-9, CA-125, PSA and coagulation tests, were
unremarkable. Upper GI bleeding was suspected.
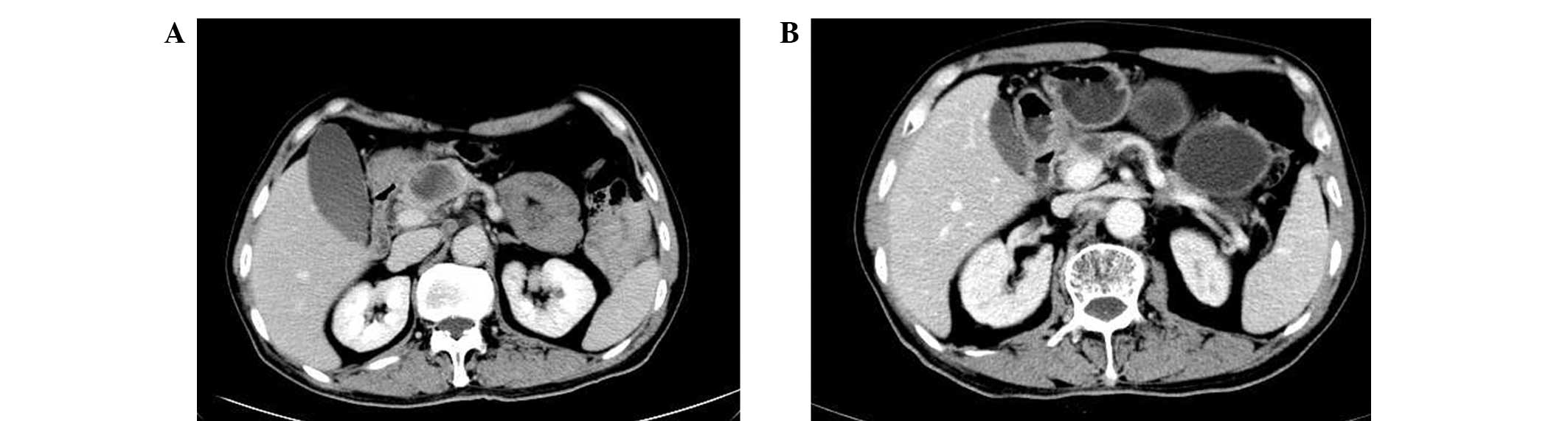
An enhanced abdominal CT scan revealed a mass that
was located in the head of the pancreas (Fig. 3A), with enlargement of the
retroperitoneal lymph nodes, which indicated malignancy. Biliary
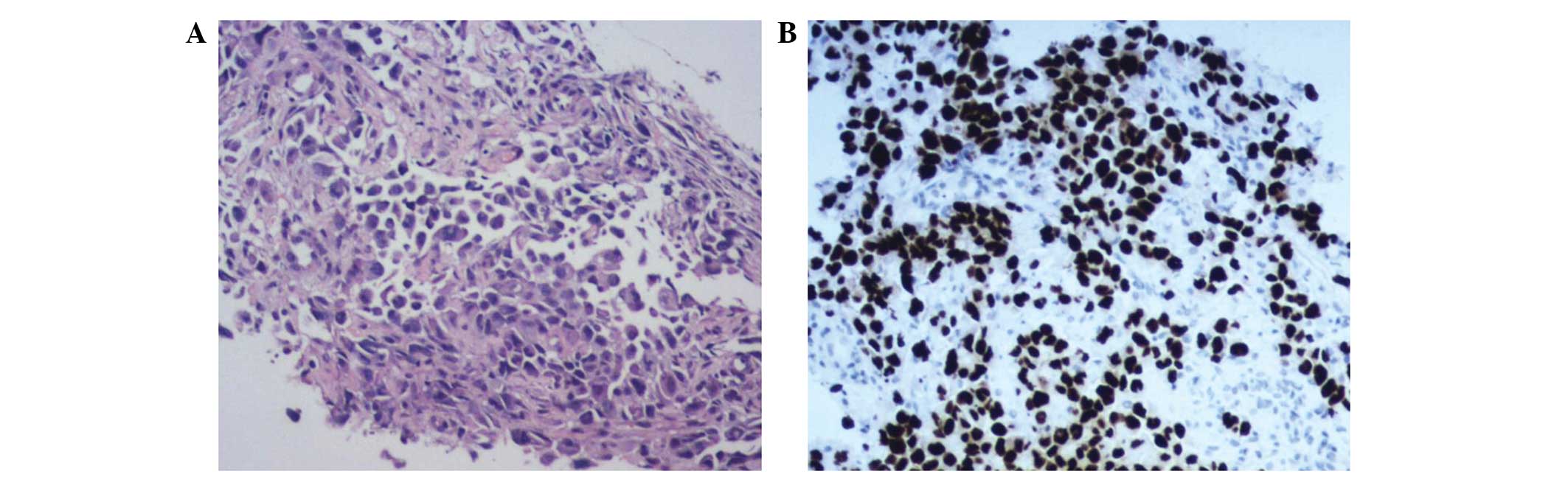
tract dilation was not detected. In August 2013, a fine-needle
ultrasonography-guided biopsy of the pancreatic head lesion
revealed adenocarcinoma (Fig. 4A).
Immunostaining confirmed that the tumor originated from the lung,
as staining was positive for CK, TTF-1 (Fig. 4B) and NapsinA, but negative for CK7,
CDX2 and CK5/6. A EGFR mutation test confirmed that the tumor was
wild-type EGFR. Subsequently, the patient was administered systemic
chemotherapy with paclitaxel (175 mg/m2, day 1) and
cisplatin (25 mg/m2, days 1–3) every three weeks for
four cycles. After two cycles of chemotherapy, an additional
abdominal CT scan revealed shrinkage of the pancreatic lesion
(Fig. 3B). Melena was no longer
present and a repeated fecal occult blood test was negative.
Furthermore, the blood hemoglobin level had increased to 79 g/l.
The patient continued chemotherapy (175 mg/m2
paclitaxel, day 1; and 25 mg/m2 cisplatin, days 1–3,
every 3 weeks) for an additional two cycles. However, treatment was
interrupted when the patient suffered a stroke. Subsequently,
chemotherapy was stopped. The patient succumbed to NSCLC in
December, 2014.
Discussion
Overall, >50% of cases of pancreatic metastases
are asymptomatic and thus, are detected during follow-up
investigations after the diagnosis of the primary lesion (9). Symptomatic metastatic lesions of the
pancreas from lung cancer are rare (10). Pancreatic metastatic lesions may
directly invade the pancreatic duct epithelium, mimicking primary
pancreatic cancer clinically. Similar to primary pancreatic
carcinoma, the majority of symptoms caused by metastatic pancreatic
lesions are not organ-specific, including weight loss, fatigue,
abdominal or back pain, nausea and jaundice (11). In the current study, the two patients
presented with weight loss. The most common symptoms of pancreatic
metastasis from lung cancer that have been reported in the
literature are obstructive jaundice and acute pancreatitis
(12,13). Z'Graggen et al (6) reported the first case of GI bleeding
following solitary metastasis from lung carcinoma in the head of
the pancreas in 1998 (6). At present,
only three cases, including the present two cases and that reported
by Z'Graggen et al (6), of GI
bleeding due to pancreatic metastasis from lung cancer have been
reported in the English literature. Metastatic lesions of the
pancreas from lung cancer that cause GI bleeding are much less
common. GI bleeding may cause anemia, as well as occult blood in
the stool, which was identified in the two cases presented in the
current study.
The clinical diagnosis of metastatic pancreatic
tumors is difficult. Imaging studies may aid with the differential
diagnosis between lung cancer and pancreatic cancer in patients
with a pancreatic mass and a history of malignant lung neoplasm
(14–16). A history of lung cancer may lead to
the diagnosis of pancreatic metastasis. As was observed in the two
cases of the present study, peripancreatic lymph node involvement
and multiple tumors may result from metastatic lung carcinoma
(17). By contrast to primary
pancreatic cancers, which are usually relatively hypo-vascular,
highly vascular tumors identified in imaging studies are more
likely to be metastases (6), which
was not indicated in the present two patients. However, patient
medical history and imaging alone cannot lead to a definitive
diagnosis, which requires pathological examination of tissue
samples. Immunohistochemical techniques provide an improved method
of distinction. TTF-1 is positive in ∼76% of lung adenocarcinomas
and CK7 is frequently reactive in both lung and pancreatic cancers
(18). In the present study, the two
patients were each positive for TTF-1, but case one was positive
for CK7 and case two was negative. The majority of pancreatic
cancers stain positively for CK20, which may provide valuable
delineation (14). Therefore,
immunostaining of TTF-1 and/or CK20 must be performed in these
patients.
NSCLC with pancreatic metastasis is classified as
stage IV disease according to the AJCC TNM staging system (7) and has a poor prognosis. However, when
patients with solitary metastasis to the pancreas are carefully
evaluated and selected, they become candidates for pancreatic
resection, with certain patients achieving long-term survival
(6,12,19). As in
the present cases, the majority of lung cancer patients suffer from
widespread disease that is unresectable (20). Platinum-based chemotherapy has been
shown to improve survival and quality of life. Chemotherapy is most
suitable for patients with a good performance status. Liu et
al (13) studied 20 patients with
lung cancer metastasis-induced acute pancreatitis, of which 15
cases were from NSCLC and five were from small cell lung cancer
(13). It was found that the group
treated with chemotherapy exhibited a longer mean survival time
(161.9 days) than those without chemotherapy treatment (25.0 days)
(P<0.01). The study hypothesized that chemotherapy may prolong
survival time of select patients with metastasis-induced acute
pancreatitis from lung cancer (13).
In the present study, the second patient received chemotherapy with
paclitaxel and carboplatin; the GI bleeding subsequently stopped
and the patient's blood hemoglobin level increased. By contrast,
the first patient did not receive chemotherapy and succumbed soon
after. We hypothesize that appropriate patients with advanced NSCLC
involving the pancreas must receive chemotherapy or other effective
treatments. Recently, newly developed target agents have shown
efficacy in certain subtypes of lung cancer. For example, patients
with sensitive EGFR gene mutations may benefit from treatment with
EGFR tyrosine-kinase inhibitors, including gefitinib and erlotinib
(21). Furthermore, the anaplastic
lymphoma kinase (ALK) tyrosine-kinase inhibitor, crizotinib,
exhibited marked antitumor activity in patients with advanced NSCLC
with ALK gene rearrangements (22).
However, in the present study, both patients were wild-type EGFR
and the ALK gene test was not performed. Thus, the patients did not
receive treatment with EGFR or ALK tyrosine-kinase inhibitors.
In conclusion, upper GI bleeding caused by
pancreatic metastasis of lung cancer is extremely rare.
Chemotherapy may stop GI bleeding and prolong patient survival, and
clinicians must consequently be aware of this manifestation. When
patients are resistant to conservative therapies, surgery is
recommended.
Acknowledgements
This study was supported by grants from the Zhejiang
Provincial Natural Science Fund (grant no. LY13H160007) and the
Zhejiang Medicines and Health Science and Technology Project (grant
no. 201348801). The authors would like to thank the patients
involved and their family members.
References
|
1
|
Breathnach OS, Freidlin B, Conley B, et
al: Twenty-two years of phase III trials for patients with advanced
non-small-cell lung cancer: sobering results. J Clin Oncol.
19:1734–1742. 2001.PubMed/NCBI
|
|
2
|
Quint LE, Tummala S, Brisson LJ, et al:
Distribution of distant metastases from newly diagnosed non-small
cell lung cancer. Ann Thorac Surg. 62:246–250. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Line DH and Deeley TJ: The necropsy
findings in carcinoma of the bronchus. Br J Dis Chest. 65:238–242.
1971. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nakamura E, Shimizu M, Itoh T and Manabe
T: Secondary tumors of the pancreas: clinicopathological study of
103 autopsy cases of Japanese patients. Pathol Int. 51:686–690.
2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Adsay NV, Andea A, Basturk O, Kilinc N,
Nassar H and Cheng JD: Secondary tumors of the pancreas: an
analysis of asurgical and autopsydatabase and review of the
literature. Virchows Arch. 444:527–535. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Z'Graggen K, Fernández-del Castillo C,
Rattner DW, Sigala H and Warshaw AL: Metastases to thepancreas and
their surgical extirpation. Arch Surg. 133:413–417. discussion
418-4191998. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Edge SB, Byrd DR, Compton CC, Fritz AG,
Greene FL and Trotti A: American Joint Committee on Cancer (AJCC)
Cancer Staging Manual. 7th. Springer, Inc.; Chicago, IL: 2010
|
|
8
|
Oken MM, Creech RH, Tormey DC, et al:
Toxicity and response criteria of the Eastern Cooperative Oncology
Group. Am J Clin Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Zerbi A and Pecorelli N: Pancreatic
metastases: An increasing clinical entity. World J Gastrointest
Surg. 2:255–259. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bestari MB and Agustanti N: Obstructive
jaundice due to pancreatic metastasis from non-small cell lung
cancer. Acta Med Indones. 45:216–219. 2013.PubMed/NCBI
|
|
11
|
Merkle EM, Boaz T, Kolokythas O, Haaga JR,
Lewin JS and Brambs HJ: Metastases to the pancreas. Br J Radiol.
71:1208–1214. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Pericleous S, Mukherjee S and Hutchins RR:
Lung adenocarcinoma presenting as obstructive jaundice: a
casereport and review of literature. World J Surg Oncol. 6:1202008.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Liu SF, Zhang S, Chen YC, et al:
Experience of cancer care for metastasis-induced acute pancreatitis
patients with lung cancer. J Thorac Oncol. 4:1231–1235. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Schwarz RE, Chu PG and Grannis FW Jr:
Pancreatic tumors in patients with lung malignancies: a spectrum of
clinicopathologic considerations. South Med J. 97:811–815. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sato M, Okumura T, Kaito K, et al:
Usefulness of FDG-PET/CT in the detection of pancreatic metastases
from lung cancer. Ann Nucl Med. 23:49–57. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Xi-wen S and Shu-zhen C: Characterization
of pancreatic metastases from primary lung cancer using magnetic
resonance imaging. Clin Imaging. 34:351–354. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Onuigbo WI: Lung cancer metastasis to
thepancreas and its surrounding lymph nodes. Br J Dis Chest.
60:152–155. 1966. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Harlamert HA, Mira J, Bejarano PA, et al:
Thyroid transcription factor-1 and cytokeratins 7 and 20
inpulmonary and breast carcinoma. Acta Cytol. 42:1382–1388. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Mori N, Sawada T, Satoh H, Kawaguchi M,
Hara H and Matsushita K: A resected case of solitary pancreatic
metastasis from adenocarcinoma of the lung. JOP. 9:698–703.
2008.PubMed/NCBI
|
|
20
|
Maeno T, Satoh H, Ishikawa H, et al:
Patterns of pancreatic metastasis from lung cancer. Anticancer Res.
18:2881–2884. 1998.PubMed/NCBI
|
|
21
|
Mok T, Yang JJ and Lam KC: Treating
patients with EGFR-sensitizing mutations: first line or second line
- is there a difference? J Clin Oncol. 31:1081–1088. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shaw AT, Yeap BY, Solomon BJ, et al:
Effect of crizotinib on overall survival in patients with advanced
non-small-cell lung cancer harbouring ALK gene rearrangement: a
retrospective analysis. Lancet Oncol. 12:1004–1012. 2011.
View Article : Google Scholar : PubMed/NCBI
|