Introduction
Pulmonary sarcomatoid carcinoma (PSC) is a rare and
heterogeneous pulmonary tumor in which carcinomatous and
sarcomatous elements occur, and accounts for 0.1–0.4% of all
pulmonary malignant tumors (1). PSC
predominantly affects males and smokers, with a median age of 51.4
years and a male to female ratio of 2.12–6:1 (2–4).
Erlotinib, which is one of the highly promising epidermal growth
factor receptor tyrosine kinase inhibitors (EGFR-TKIs), is
administered orally once daily for the treatment of patients with
non-small cell lung cancer (NSCLC). The present study reports the
first case of PSC successfully treated with erlotinib. The
spatio-temporal evolution of EGFR mutation heterogeneity between
the primary lesion and metastasis, as well as between metastases,
was also analyzed in the present study. Written informed consent
was obtained from the patient's family.
Case report
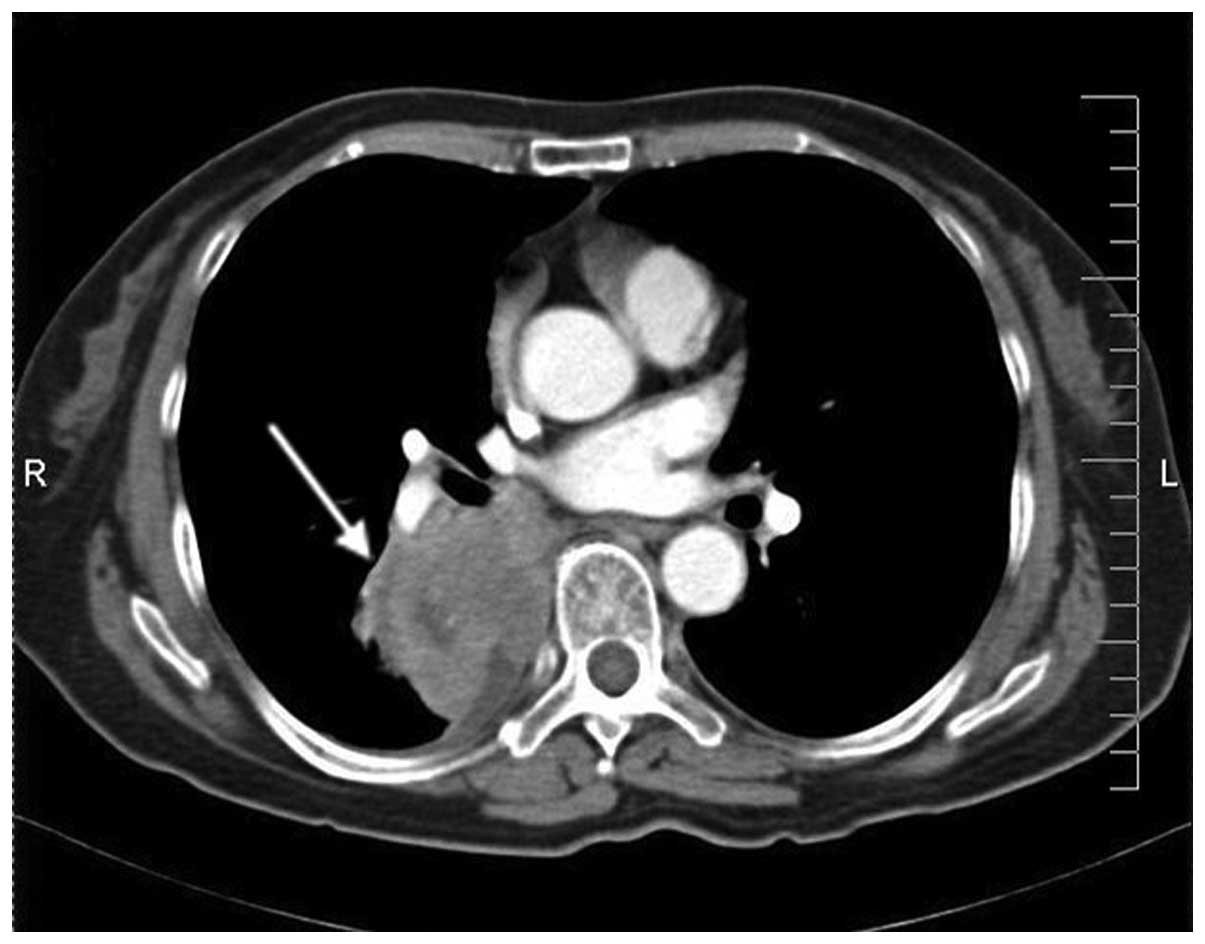
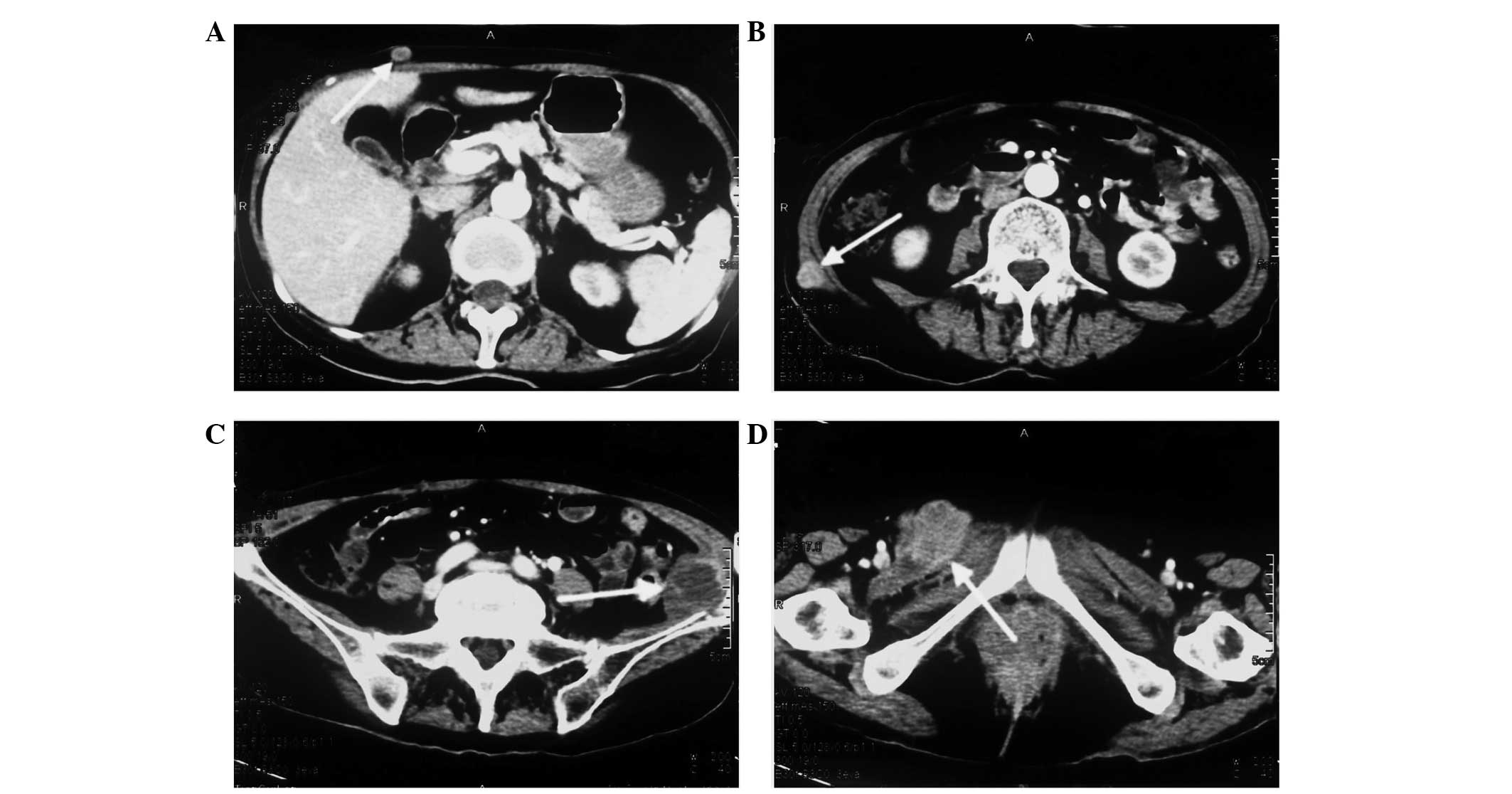
A 73-year-old female was admitted to the Department
of Oncology at Xiangya Second Hospital of Central South University
(Changsha, China) in November 2012 due to violent coughing for 1
month. A computed tomography (CT) scan revealed a 5.2×4.5 cm mass
in the lower right lung (Fig. 1), and
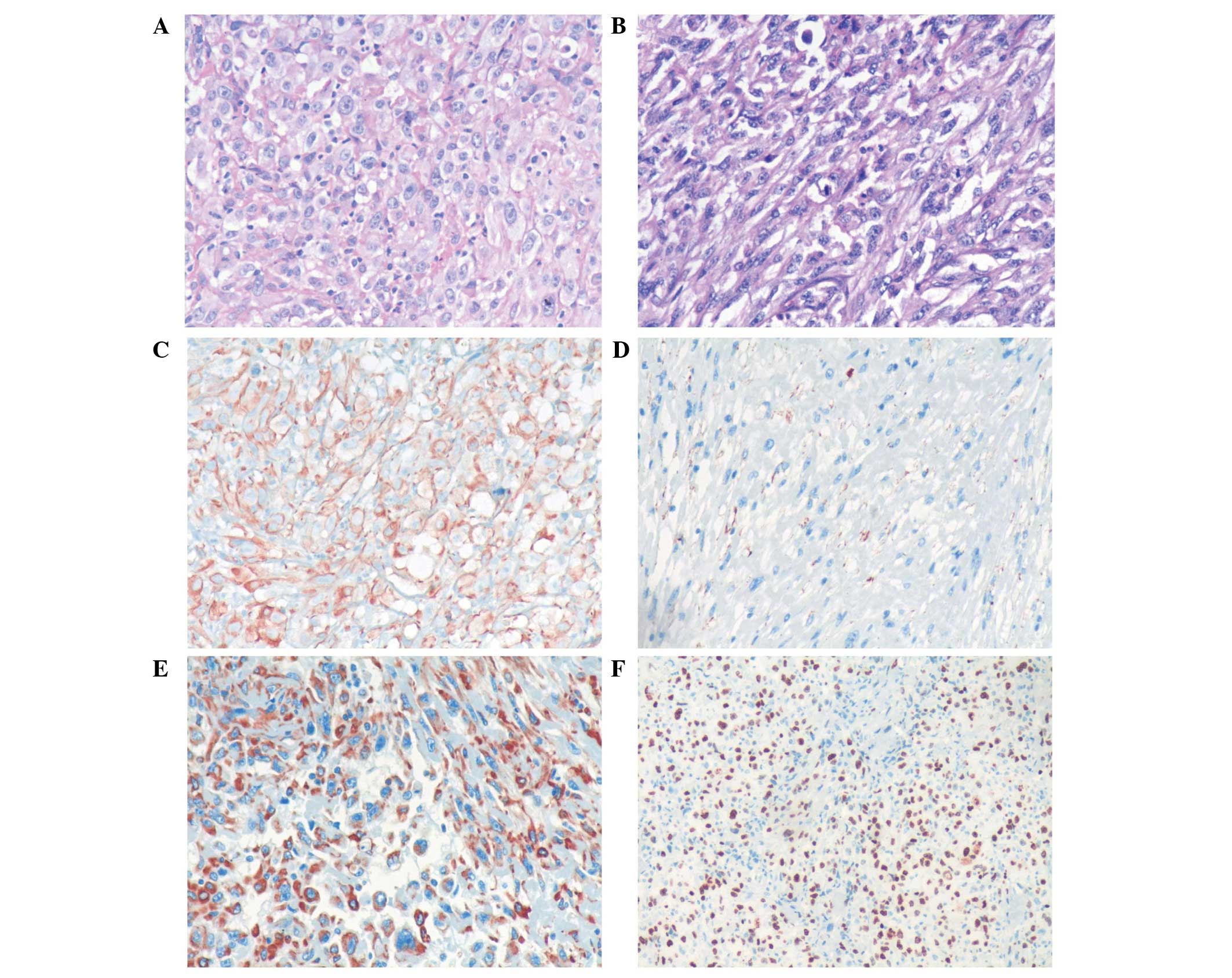
a pulmonary needle biopsy revealed carcinomatous and sarcomatous
components within the lesion (Fig. 2A and
B). Immunohistochemically, the tumor cells were positive for
the expression of creatine kinase (CK; Fig. 2C), epithelial membrane antigen (EMA;
Fig. 2D), vimentin (Fig. 2E) and Ki-67 (Fig. 2F), and did not express thyroid
transcription factor-1 (TTF-1), smooth muscle actin (SMA) or S100.
An amplification-refractory mutation system (ARMS) test revealed
that the lesion possessed the wild-type EGFR gene. These findings
were consistent with the features of PSC and clinical
tumor-node-metastasis (cTNM) stage IIIa (cT3N2M0). The patient
refused surgery and underwent four 21-day cycles of chemotherapy,
comprising a regimen of gemcitabine (1,600 mg, days 1 and 8) and
cisplatin (30 mg, days 1–3) combined with intensity-modulated
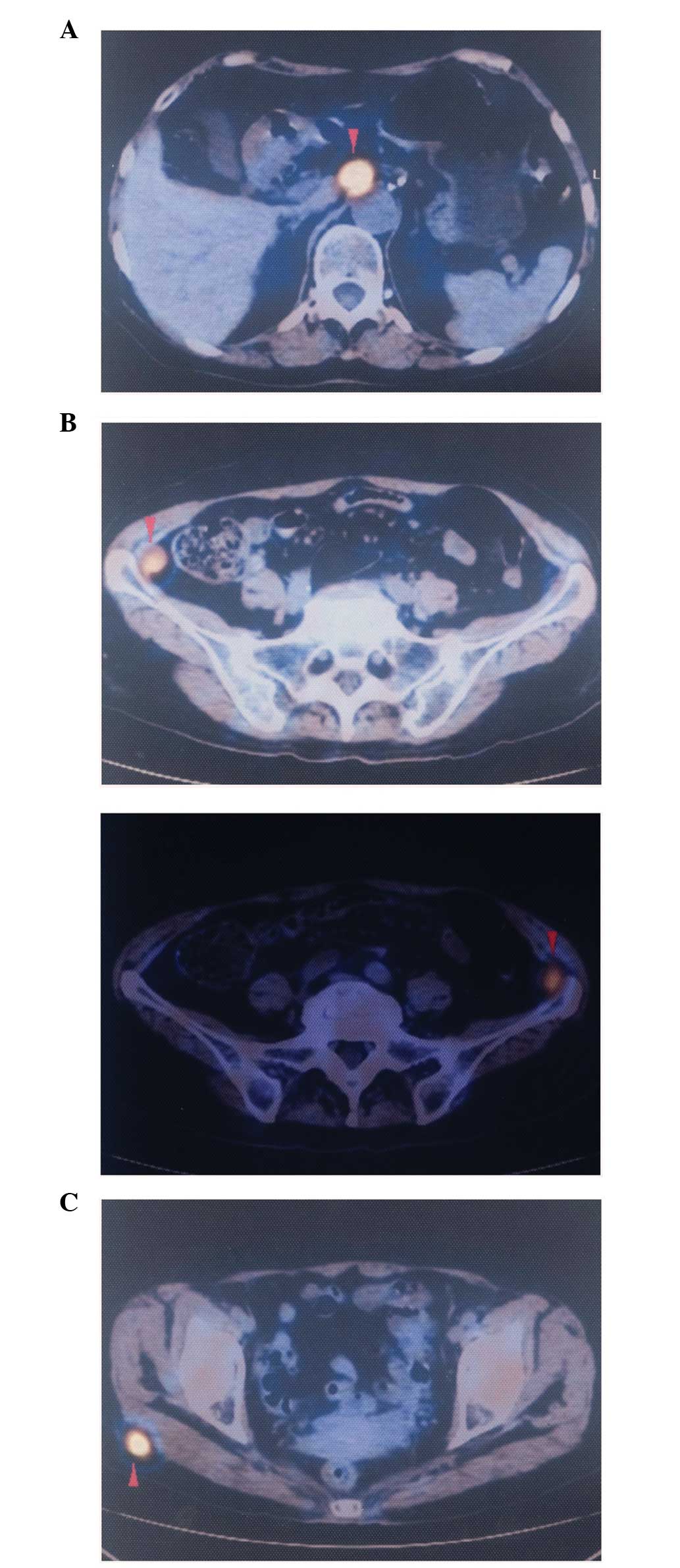
radiotherapy (2 Gy/30 fractions). In December 2012, positron
emission tomography/CT (Fig. 3)
revealed that the right lower mass of the lung was in complete
remission, but metastases had arisen in the paraaortic lymph node,
bilateral iliac fossa and the right gluteal region. Notably, an
EGFR exon 21 L858R mutation was identified in the right gluteal
metastatic lesion using the ARMS test. Therefore, treatment with
150 mg of erlotinib once daily was initiated. However, six months
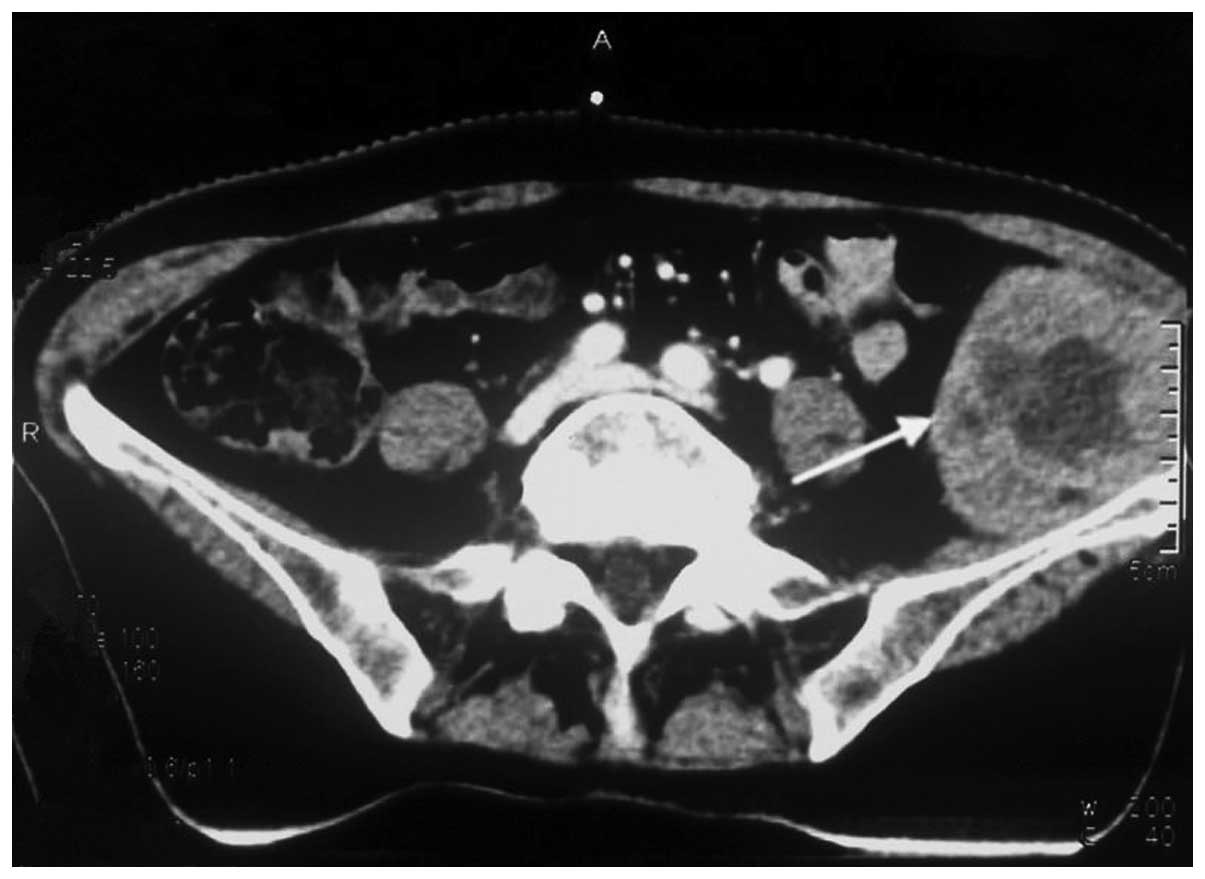
subsequent to targeted therapy, CT (Fig.
4) revealed that the right iliac fossa metastases had decreased
in size and the paraaortic lymph node metastasis had disappeared,
but the left iliac fossa metastases had increased in size.
Erlotinib was administered continually in combination with
radiotherapy to treat the left iliac fossa metastasis. Two months
later, a repeat CT (Fig. 5) revealed
that the left iliac fossa mass had decreased in size, but
metastases were identified in the right gluteal region, right groin
and the right chest wall of the right-lower abdomen. Biopsy of the
right iliac fossa, right gluteal tumor and the right chest wall,
the right abdominal subcutaneous nodules were all revealed to be
metastatic sarcomatoid carcinoma, and all were revealed to also
possess wild-type EGFR without the T790M mutation by performing an
ARMS test (Fig. 6). The patient was
therefore treated with two 21-day cycles of pemetrexed (800 mg, day
1), instead of erlotinib. In September 2013, CT re-examination
revealed multiple organ metastases to the liver, pancreas and left
adrenal gland. The patient received nutritional support, but
succumbed to the disease in October 2013.
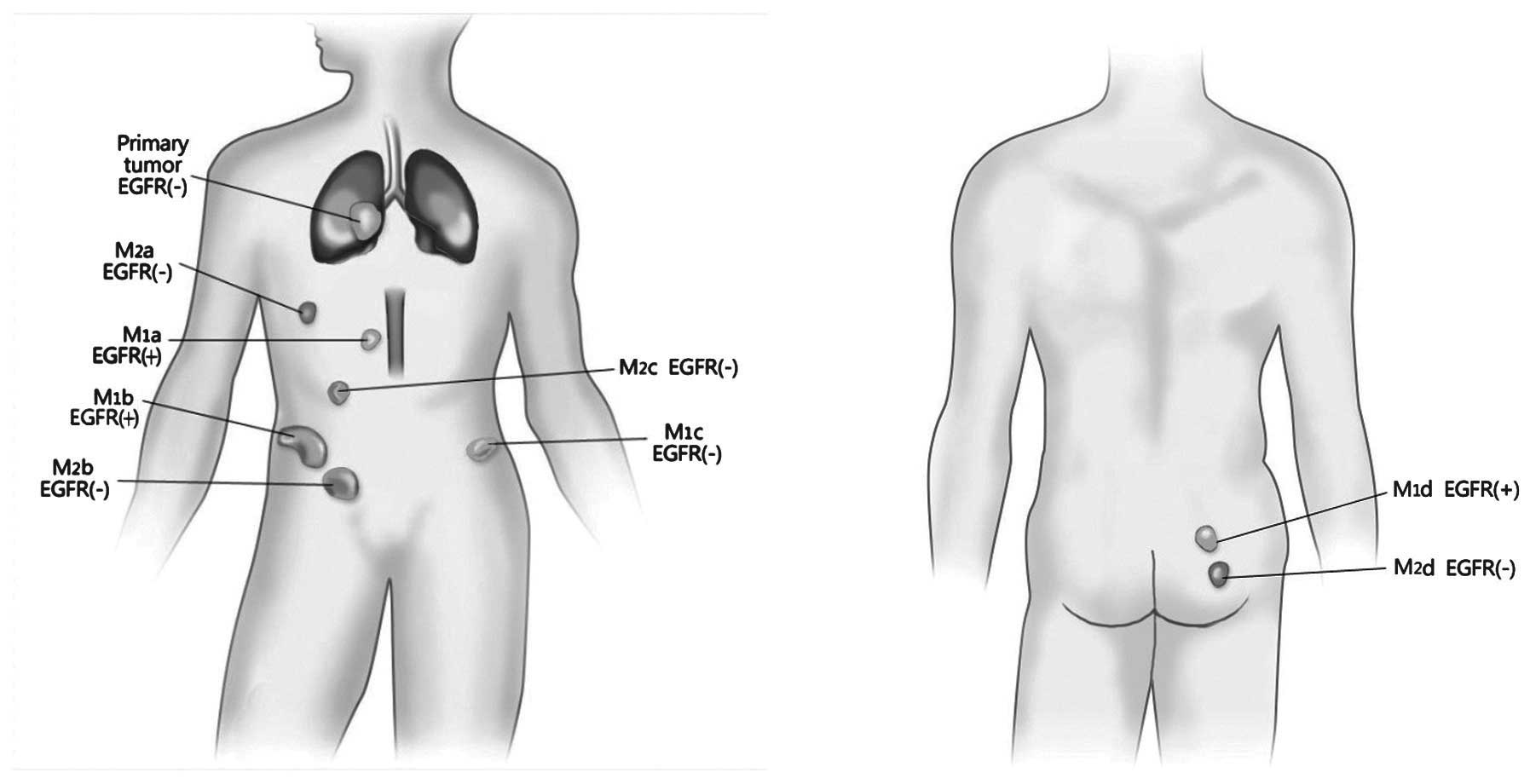
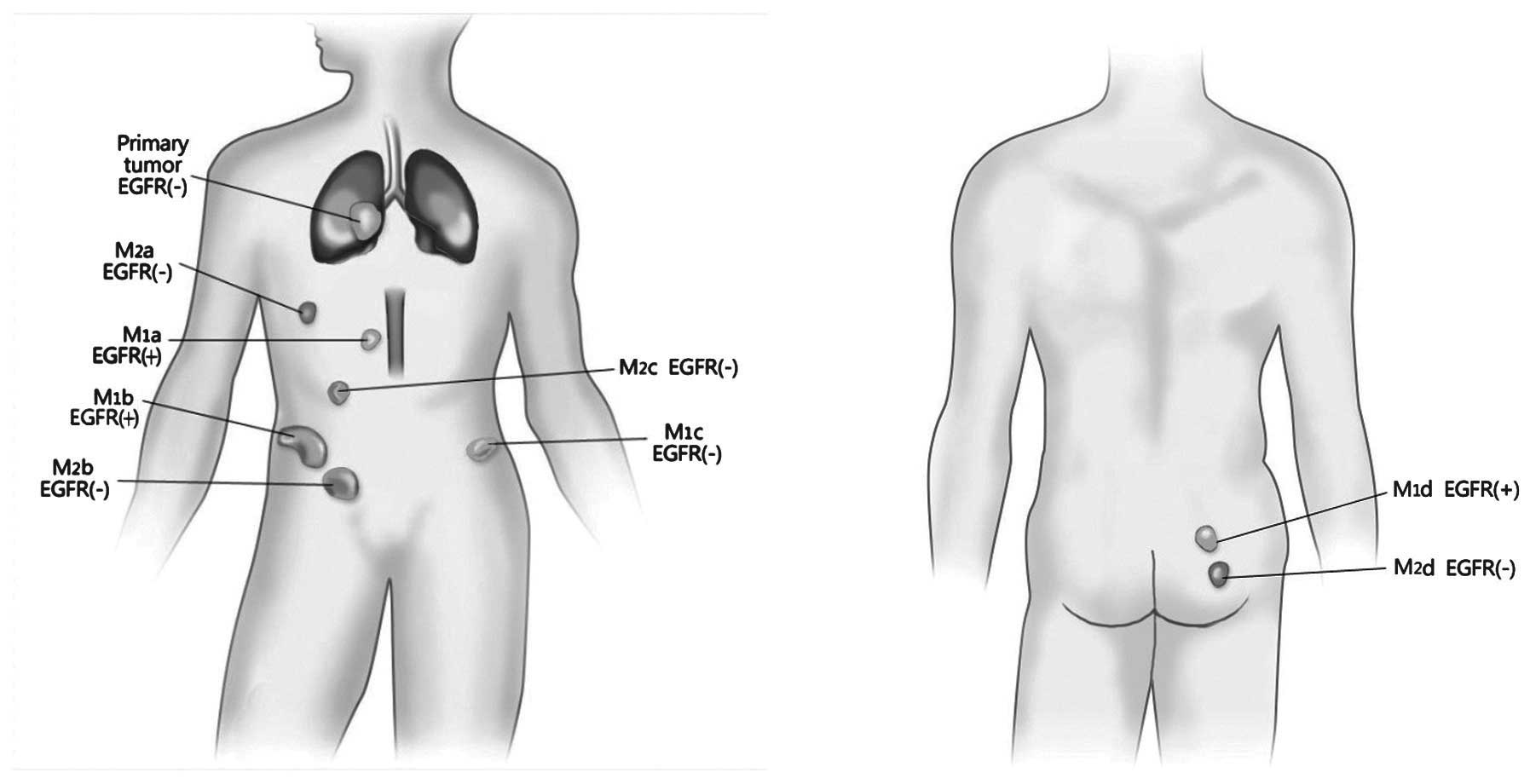 | Figure 6.Diagram demonstrating the
spatio-temporal evolution of the EGFR mutation. M1a,
clinically-diagnosed EGFR(+) paraaortic lymph node lesion; M1b,
clinicallay-diagnosed EGFR(+) lesion in the right iliohypogastric
region; M1c, EGFR(-) lesion in the left iliohypogastric region,
assessed by ARMS testing; and M1d, EGFR(+) lesion in the right
gluteal region, assessed by ARMS testing. M2a, EGFR(-) lesion in
the right chest wall, assessed by ARMS testing; M2b, EGFR(-) lesion
in the right abdominal wall, assessed by ARMS testing; M2c, EGFR(-)
lesion in the right groin, assessed by ARMS testing; and M2d,
EGFR(-) lesion in the right gluteal region, assessed by ARMS
testing. M1, inital group of metastatic lesions; M2, second group
of metastatic lesions; EGFR, epidermal growth factor receptor;
ARMS, amplification-refractory mutation system. |
Discussion
According to the 2004 World Health Organization
classification (5), PSC can be
divided into five subtypes, consisting of pleomorphic carcinoma,
spindle cell carcinoma, giant cell carcinoma, carcinosarcoma and
pneumoblastoma. Overall, PSC runs an aggressive clinical course,
with the five-year survival rate for patients with PSC being only
24.5%, which is a worse rate compared with other forms of NSCLC
(6,7).
In addition, distant metastasis can be identified in the early
stages of the disease (8).
Surgery is currently considered to be the best
option for the treatment of PSC (9)
alongside chemoradiotherapy, which mainly refers to the
chemotherapy regimens for NSCLC treatment (10). The effect of EGFR-TKIs on PSC remains
unclear, and the available studies on the expression of EGFR are
also limited. Italiano et al (11) tested the EGFR status of 22 PSC
patients and the results revealed that none presented with EGFR
mutation. However, Leone et al (12) retrospectively tested the EGFR status
of 23 patients and the results revealed an EGFR exon 19 deletion in
two patients. Ushiki et al (13) reported one patient who did not receive
therapeutic effect from the administration of gefitinib. However,
the autopsy of this patient revealed an EGFR exon 19 deletion, and
a T790M drug-resistant mutation. In this case, the patient was a
female with no smoking history. An EGFR exon 21 L858R mutation was
identified in the metastatic lesion. In the present study, the
patient experienced progression-free survival for the six months
following the initiation of erlotinib therapy. However, resistance
emerged finally, which may have been caused by EGFR mutational
heterogeneity.
EGFR mutation heterogeneity is a common phenomenon
in pulmonary carcinoma tissue (14,15).
Numerous studies have supported that the NSCLC primary and
metastatic lesions also exhibit EGFR mutation heterogeneity
(16–19). However, no study has yet reported EGFR
mutation heterogeneity in PSC lesions. The present patient was
identified as possessing EGFR mutation heterogeneity between the
primary and metastatic lesions, as well as between the metastases,
which demonstrated the double characteristics of temporal and
spatial evolution. In the present study, the pulmonary primary
lesion was EGFR wild-type, but in the first group of metastases,
the lesion in the right gluteal region possessed a EGFR mutation
and the lesion in the left iliac fossa was wild-type. Within the
second group of metastases, the paraaortic lymph node and right
iliac fossa metastases possessed EGFR mutations, according to the
clinical response. Among the second array of metastases, all four
lesions were wild type. With the exception of the pulmonary primary
lesion, which was able to be well-controlled
post-chemoradiotherapy, the therapeutic response of the metastatic
lesions overall conformed to that expected due to the EGFR status.
To the best of our knowledge, the spatio-temporal heterogeneous
evolution of tumors has only been previously reported by Gerlinger
et al (20) and Sequist et
al (21).
In summary, the present study is the first case
report of PSC successfully treated using erlotinib. The findings
suggest that erlotinib is a viable therapeutic option for patients
with PSC that possesses an EGFR mutation. However, the
spatio-temporal evolution of EGFR mutational heterogeneity in PSC
may result in drug-resistance, which challenges EGFR-TKI therapy
and the diagnosis of EGFR gene mutation. Therefore, multiple
biopsies may be necessary in cases exhibiting EGFR mutational
heterogeneity.
References
|
1
|
Park JS, Lee Y, Han J, et al:
Clinicopathologic outcomes of curative resection for sarcomatoid
carcinoma of the lung. Oncology. 11:206–213. 2011. View Article : Google Scholar
|
|
2
|
Zhou Z, Jiang GN, Yang TS, et al: Analysis
for the prognosis of patients with pulmonary carcinosarcoma. Zhong
Guo Ai Zheng Za Zhi. 20:59–61. 2010.
|
|
3
|
Fishback NF, Travis WD, Moran CA, et al:
Pleomorphic (spindle/giant cell) carcinoma of the lung. A
clinicopathologic correlation of 78 cases. Cancer. 73:2936–2945.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Nakajima M, Kasai T, Hashimoto H, et al:
Sarcomatoid carcinoma of the lung: a clinicopathologic study of 37
cases. Cancer. 86:608–616. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Beasley MB, Brambilla E and Travis WD: The
2004 World Health Organization classification of lung tumors. Semin
Roentgenol. 40:90–97. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Venissac N, Pop D, Lassalle S, et al:
Sarcomatoid lung cancer (spindle/giant cells): an aggressive
disease? J Thorac Cardiovasc Surg. 134:619–623. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Brambilla E, Travis WD, Colby TV, Corrin B
and Shimosato Y: The new World Health Organization classification
of lung tumours. Eur Respir J. 18:1059–1068. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Homman T, Doki Y, Tsuda M, et al:
Uncontrollable midbrain hemorrhage due to brain metastasis of
pulmonary pleomorphic carcinoma. Kyobu Geka. 61:335–339. 2008.[(In
Japanese)]. PubMed/NCBI
|
|
9
|
Petrov DB, Vlassov VI, Kalaydjiev GT,
Plochev MA, Obretenov ED, Stanoev VI and Danon SE: Primary
pulmonary sarcomas and carcinosarcomas - postoperative results and
comparative survival analysis. Eur J Cardiothorac Surg. 23:461–466.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shi YK: NCCN clinical practice guidelines
in non-small cell lung cancer V.2.2008. Zhong Hua Zhong Liu Za Zhi.
30:397–400. 2008.
|
|
11
|
Italiano A, Cortot AB, Ilie M, et al: EGFR
and KRAS status of primary sarcomatoid carcinomas of the lung:
implications for anti-EGFR treatment of a rare lung malignancy. Int
J Cancer. 125:2479–2482. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Leone A, Graziano P, Gasbarra R, et al:
Identification of EGFR mutations in lung sarcomatoid carcinoma. Int
J Cancer. 128:732–735. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Ushiki A, Koizumi T, Kobayashi N, et al:
Genetic heterogeneity of EGFR mutation in pleomorphic carcinoma of
the lung: response to gefitinib and clinical outcome. Jpn J Clin
Oncol. 39:267–270. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Taniguchi K, Okami J, Kodama K, et al:
Intratumor heterogeneity of epidermal growth factor receptor
mutations in lung cancer and its correlation to the response to
gefitinib. Cancer Sci. 99:929–935. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Tomonaga N, Nakamura Y, Yamaguchi H, et
al: Analysis of intratumor heterogeneity of EGFR mutations in
mixed-type lung adenocarcinoma. Clin Lung Cancer. 14:521–526. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Gow CH, Chang YL, Hsu YC, et al:
Comparison of epidermal growth factor receptor mutations between
primary and corresponding metastatic tumors in tyrosine kinase
inhibitor-naive non-small-cell lung cancer. Ann Oncol. 20:696–702.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Schmid K, Oehl N, Wrba F, et al:
EGFR/KRAS/BRAF mutations in primary lung adenocarcinomas and
corresponding locoregional lymph node metastases. Clin Cancer Res.
15:4554–4560. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Sun L, Zhang Q, Luan H, et al: Comparison
of KRAS and EGFR gene status between primary non-small cell lung
cancer and local lymph node metastases: implications for clinical
practice. J Exp Clin Cancer Res. 30:302011. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Fang Q, Zhang L, Wang S and Ou W:
Discordance of epidermal growth factor receptor mutations between
primary and corresponding metastatic tumors in non-small cell lung
cancer. Zhongguo Fei Ai Za Zhi. 14:518–522. 2011.[(In Chinese)].
PubMed/NCBI
|
|
20
|
Gerlinger M, Rowan AJ, Horswell S, et al:
Intratumor heterogeneity and branched evolution revealed by
multiregion sequencing. N Engl J Med. 366:883–892. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Sequist LV, Waltman BA, Dias-Santagata D,
et al: Genotypic and histological evolution of lung cancers
acquiring resistance to EGFR inhibitors. Sci Transl Med.
3:75ra262011. View Article : Google Scholar : PubMed/NCBI
|