Introduction
Lymphangioma, also known as angioma lymphaticum, is
a congenital malformation of the vascular system, comprising
newly-formed lymph spaces and channels (1). Landing and Farber (2) classified this benign malformation in
four categories, including capillary, cavernous and cystic
(hygroma) lymphangioma, and hemolymphangioma, which is a
combination of hemangioma and lymphangioma.
Hemolymphangioma is a congenital malformation that
may be asymptomatic for a long period of time (3). This lesion is typically considered to be
a benign and noninvasive disorder, characterized by the presence of
dilated lymphatic spaces, extravasation of red blood cells,
hemosiderin deposition and fibrosis (4). Hemolymphangioma formation may be due to
venolymphatic communication obstruction between the
dysembrioplastic vascular tissue and systemic circulation (5).
The incidence of hemolymphangioma is 1.2–2.8 per
1,000 newborn infants (6).
Hemolymphangioma has been previously detected at the pancreas
(5,7–12), spleen
(13–16), stomach (1,17), rectum
(18), mediastinum (19–21), chest
wall (22–25), small intestine (26), extremities (3,27,28), cervix (29,30),
pericardium (31), oral region
(32), esophagus (33), axilla (34), retroperitoneal space (35,36),
adrenal gland (37), abdomen
(38), duodenum (4) and hepatica (39), as well as on the tongue (40,41) and
orbit (42,43). However, to the best of our knowledge,
no studies have reported this type of tumor in the waist region, as
determined by a review of the medical literature until June 2014
using the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed; accessed on 9th
June 2014). Complete excision is considered the optimal treatment
for hemolymphangioma, which exhibits a low recurrence rate.
Non-surgical treatments are also used, including aspiration and
drainage, cryotherapy, injection of sclerotic agents, laser therapy
and radiotherapy, however, to date, the outcomes of such treatments
have been unsatisfactory (3,22). In cases of tumor recurrence,
conservative treatment methods such as laser therapy, may be
applied (3,44). Generally, the prognosis of
hemolymphangioma is good (3,4,13,17,18),
however, careful follow-up is required.
The present study reported the case of a 17-year-old
male patient with hemolymphangioma on the waist and reviewed the
characteristics of this disease based on the existing
literature.
Case report
A 17-year-old male was admitted at the General
Hospital of Armed Police Force (Beijing, China) in September 2013,
complaining of a mass on the right side of the waist and back pain
for approximately four months. The back pain was significantly
increased when the patient was sedentary and was slightly
alleviated by rest. On admission, the patient was well, with no
symptoms of lower extremity numbness and pain, or abdominal pain.
Upon physical examination, the lesion was identified to be oval in
shape, soft and compressible, with mild tenderness. No
abnormalities were detected in the results of laboratory
examinations. An ultrasound (Doppler sonography) detected a cystic
lesion (15.0×10.0 cm) with blood flow, and revealed multiple echo
and irregular cavities in the subcutaneous fat layer of the right
waist. The most likely diagnosis was hemolymphangioma.
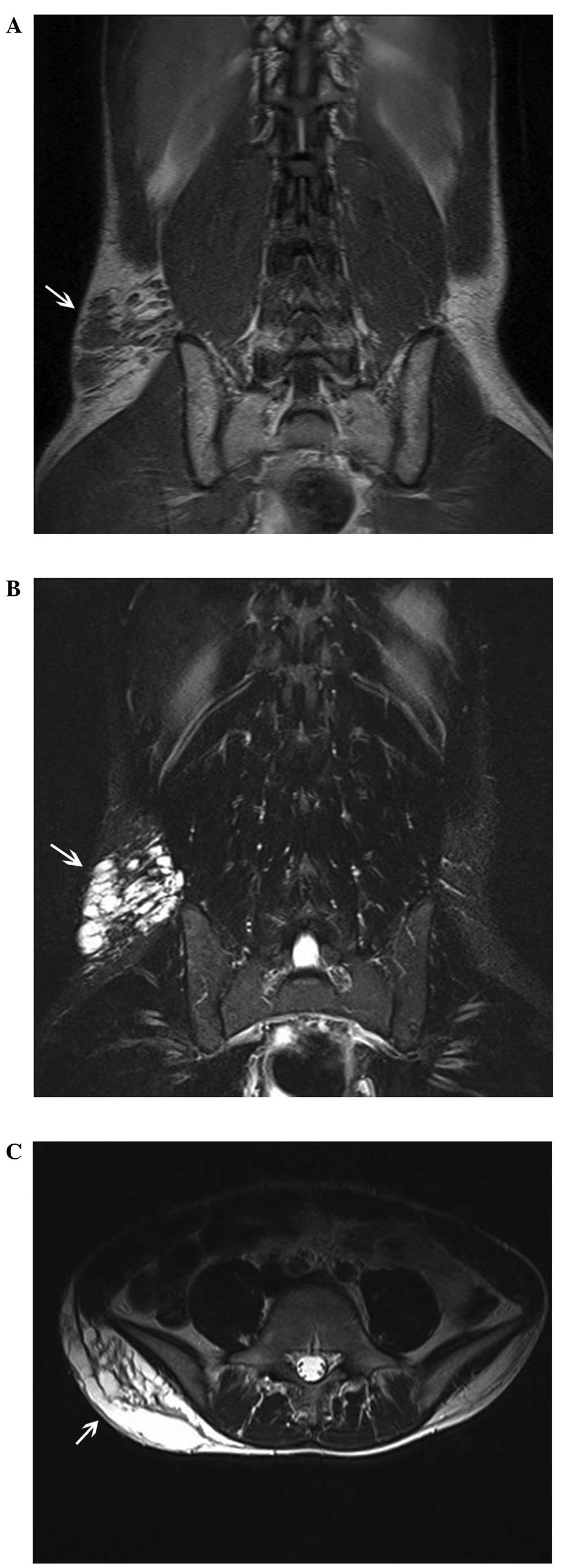
Magnetic resonance imaging (MRI) examination was
performed preoperatively, in order to establish the extent of the
tumor and define its association with the surrounding tissues. A
waist MRI scan (Fig. 1) revealed a
12.6×9.7-cm mass, with low signal intensity on T1-weighted imaging
(WI) and high signal intensity on T2-WI in the right side of the
waist subcutaneous tissue with the fifth lumbar level parallel.
Upon performing a tumor biopsy with a 5-ml syringe, 10-ml yellow,
clear liquid was extracted and laboratory examinations were
performed. Preoperatively, no abnormalities were revealed in the
laboratory data, including the levels of tumor markers
[α-fetoprotein, carcinoembryonic antigen, carbohydrate antigen (CA)
19-9, and CA-125] and concentrated mycobacterium tuberculosis.
Due to the patient experiencing back pain that was
increased upon sitting, surgical excision was decided as the
treatment strategy. During surgery, the boundary of the mass was
unclear and a bloody yellow exudate was observed. Macroscopically,
the mass measured approximately 12.0×6.0×6.0 cm, and was oval and
soft. Multiloculated cystic masses filled with blood and yellow
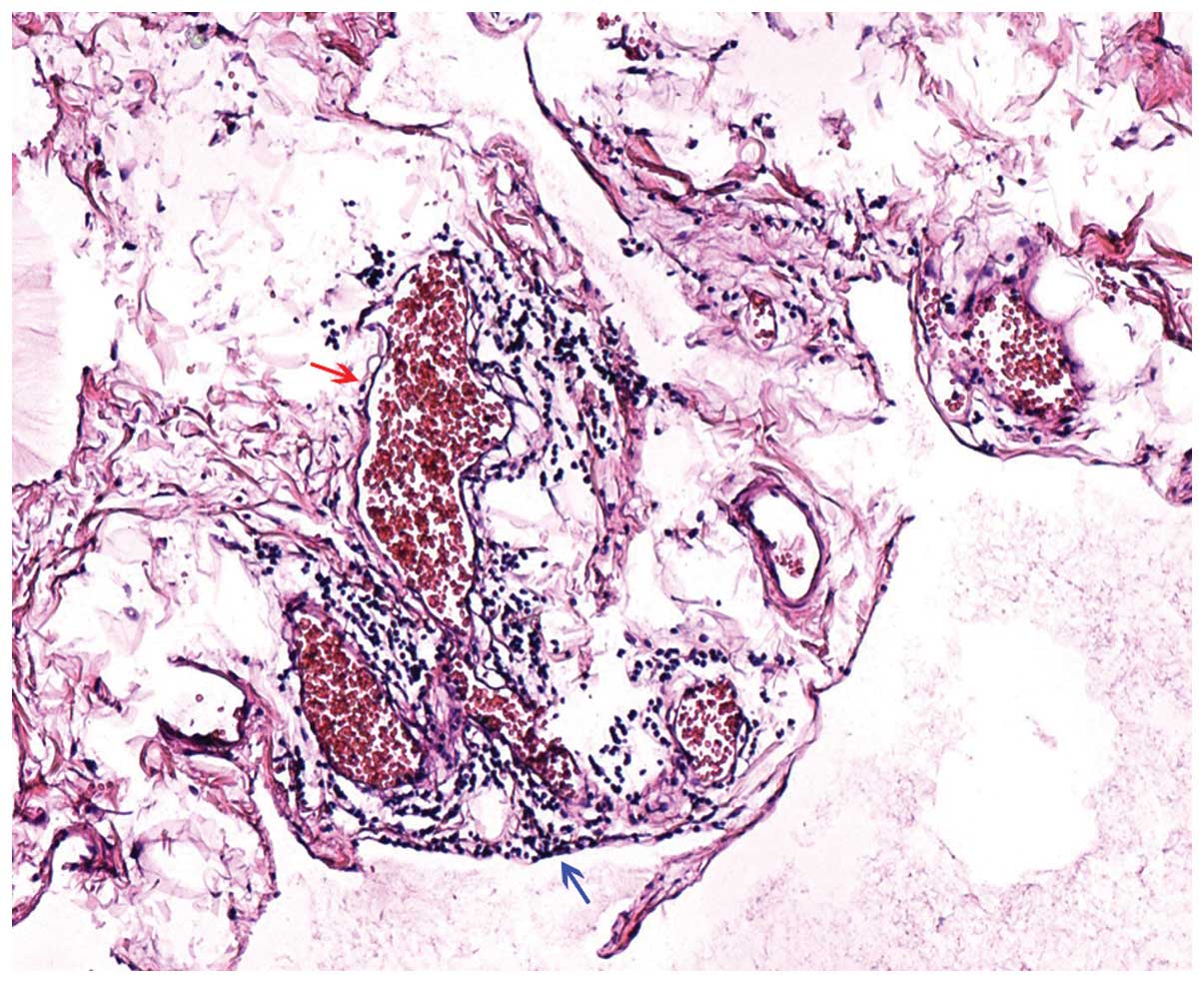
fluid were extracted. Histologically, the tumor was composed of
lymphatic and blood vessels with polycystic spaces (Fig. 2). Considering these observations, the
definitive histological diagnosis was hemolymphangioma of the
waist. The postoperative course of the patient was uneventful. In
the course of a seven-month follow-up period, no recurrence of
hemolymphangioma was observed. This study was approved by the
ethics committee of General Hospital of Armed Police Force
(Beijing, China) and written informed consent was obtained from the
patient's family.
Discussion
Hemolymphangiomas, a congenital malformation of the
vascular system, can be classified into primary and secondary
lymphatic vascular tumors. Primary tumors are congenital
malformations of the lymphatic vascular system, possibly formed due
to obstruction of the venolymphatic communication between the
dysembryoplastic vascular tissue and the systemic circulation. By
contrast, secondary tumors are likely to be caused by poor lymph
drainage and lymphatic damage resulting from surgery or trauma
(43). Hemolymphangioma mainly
presents as cystic or cavernous lesions. Histologically,
hemolymphangioma is composed of dense fibrous tissue that develops
in bands between the numerous vascular spaces, invading the
subcutaneous fat and involving the blood or lymphatic vessels
(3).
The incidence of hemolymphangioma is 1.2–2.8 per
1,000 newborns (45), and the two
genders are equally affected. In the present study, a review of the
literature up to June 2014 was performed using the PubMed database.
The search strategy to identify all possible studies involved use
of the word ‘hemolymphangioma’. In total, 47 previous studies
concerning this type of tumor were identified (1,3–42,44,46–50).
However, to the best of our knowledge, no studies have reported
hemolymphangioma of the waist. In the current case, the patient was
a 17-year-old male, and the tumor occurred on the waist and
appeared as a cystic lesion.
Clinically, the onset of hemolymphangioma can vary
between a slow-growing cyst over a period of years and an
aggressive enlarging tumor without invasive ability (3). The size of these tumors varies due to
the different anatomical location and association with the
neighboring tissues. In clinical examinations, they are usually
described as soft and compressible masses, loculated in pattern.
The most common complications are random or traumatic hemorrhage,
rupture and infection (3). However,
no abnormal laboratory findings were observed in the current
patient, and the only symptom was back pain for four months.
In the present study, a waist MRI scan revealed a
tumor with low signal intensity on T1-WI and high signal intensity
on T2-WI on the right side of the waist subcutaneous tissue in the
fifth lumbar level. These observations may indicate the presence of
a lower number of tortuous blood vessels and water-based substance
in the lesion, which was then confirmed during surgery. Imaging
examinations, including ultrasound, computed tomography and MRI
scans, are useful in order to confirm the diagnosis, identify the
tumor nature, and observe its extension and association with the
surrounding tissues, assisting the selection of the surgical
strategy and follow-up treatment (51). However, a definitive diagnosis of the
tumor in the present study was based on histological evidence.
Surgical resection appears to be the most effective
treatment for hemolymphangioma. In order to prevent recurrence,
thorough radical resection may be required during surgery. In the
English literature, the reported recurrence rates were in the range
of 10–27% upon complete removal of the lesions, while the
recurrence rates were 50–100% in cases where the lesions were
partially removed (4,52). The extend of surgical resection
depends mainly on the anatomical location and complexity of the
tumor (3,4,12,52).
In conclusion, hemolymphangioma of the waist is an
uncommon vascular and lymphatic lesion, presenting mainly with back
pain. Preoperative imaging examinations, including ultrasound and
MRI, are important for a full evaluation of the tumor in order to
confirm the diagnosis and plan the surgical strategy. Complete
surgical resection is the most effective treatment with good
prognosis.
References
|
1
|
Li QY, Xu Q, Fan SF and Zhang Y: Gastric
haemolymphangioma: a literature review and report of one case. Br J
Radiol. 85:e31–e34. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Landing BH and Farber S: Tumors of the
Cardiovascular SystemAtlas of Tumor Pathology. Armed Forces
Institute of Pathology; Washington DC: pp. 124–138. 1956
|
|
3
|
Kosmidis I, Vlachou M, Koutroufinis A and
Filiopoulos K: Hemolymphangioma of the lower extremities in
children: two case reports. J Orthop Surg Res. 5:562010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Antonino A, Gragnano E, Sangiuliano N, et
al: A very rare case of duodenal hemolymphangioma presenting with
iron deficiency anemia. Int J Surg Case Rep. 5:118–121. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Balderramo DC, Di Tada C, de Ditter AB and
Mondino JC: Hemolymphangioma of the pancreas: case report and
review of the literature. Pancreas. 27:197–199. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Filston HC: Hemangiomas: cystic hygromas
and teratomas of the head and neck. Semin Pediatr Surg. 3:147–159.
1994.PubMed/NCBI
|
|
7
|
Sun LF, Ye HL, Zhou QY, et al: A giant
hemolymphangioma of the pancreas in a 20-year-old girl: a report of
one case and review of the literature. World J Surg Oncol.
7:312009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Toyoki Y, Hakamada K, Narumi S, et al: A
case of invasive hemolymphangioma of the pancreas. World J
Gastroenterol. 14:2932–2934. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Banchini E, Bonati L and Villani LG: A
case of hemolymphangioma of the pancreas. Minerva Chir. 42:807–813.
1987.[(In Italian)]. PubMed/NCBI
|
|
10
|
Montete P, Marmuse JP, Claude R and
Charleux H: Hemolymphangioma of the pancreas. J Chir (Paris).
122:659–663. 1985.[(In French)]. PubMed/NCBI
|
|
11
|
Couinaud C, Jouan, Prot, Chalut, Favre and
Schneiter: A rare tumor of the head of the pancreas.
Hemolymphangioma weighing 1,500 kg. Presse Med. 75:1955–1956.
1967.[(In French)]. PubMed/NCBI
|
|
12
|
Couinaud, Jouan, Prot, Chalut and
Schneiter: Hemolymphangioma of the head of the pancreas. Mem Acad
Chir (Paris). 92:152–155. 1966.[(In French)]. PubMed/NCBI
|
|
13
|
Zhang Y, Chen XM, Sun DL and Yang C:
Treatment of hemolymphangioma of the spleen by laparoscopic partial
splenectomy: a case report. World J Surg Oncol. 12:602014.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dong F, Zheng Y, Wu JJ, et al:
Hemolymphangioma: a rare differential diagnosis of cystic-solid or
cystic tumors of the pancreas. World J Gastroenterol. 19:3520–3523.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Bethouart M, Houcke M, Proye C and
Linquette M: Hepatosplenic hemolymphangioma. Lille Med. 25:288–290.
1980.[(In French)]. PubMed/NCBI
|
|
16
|
Scaltriti F and Manenti A:
Hemolymphangioma of the lower pole of the spleen (migrated into the
pelvis minor). Chir Ital. 19:543–554. 1967.[(In Italian)].
PubMed/NCBI
|
|
17
|
Kim WT, Lee SW and Lee JU: Bleeding
gastric hemolymphangioma: endoscopic therapy is feasible. Dig
Endosc. 25:553–554. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Chen G, Cui W, Ji XQ and Du JF: Diffuse
hemolymphangioma of the rectum: a report of a rare case. World J
Gastroenterol. 19:1494–1497. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Zehani A, Ayadi-Kaddour A, Cherif J,
Marghli A, et al: Cystic mediastinal hemolymphangioma. Tunis Med.
90:754–755. 2012.[(In French)]. PubMed/NCBI
|
|
20
|
Contamin C, Denis B, Mallion JM, et al:
Heart hemolymphangioma. Apropos of a case. Coeur Med Interne.
12:671–678. 1973.[(In French)]. PubMed/NCBI
|
|
21
|
Bagolan P, Alati E and Fisicaro M: Some
defects of development of the mediastinum; three cases: one
cavernous hemolymphangioma and two cystic hygromas. Archivio Chir
Torace. 10:559–573. 1953.[(In Italian)]. PubMed/NCBI
|
|
22
|
Zhang X, Sheng X, Liu F, et al:
Hemolymphangioma of the chest wall: A rare case report. Oncol Lett.
3:816–818. 2012.PubMed/NCBI
|
|
23
|
Bosdure E, Mates M, Mely L, et al: Cystic
intrathoracic hemolymphangioma: a rare differential diagnosis of
acute bronchiolitis in an infant. Arch Pediatr. 12:168–172.
2005.[(In French)]. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Zernov NG, Poliakov VE and Vorob'eva ML:
Diseases of the lymphatic vessels in children lymphangioma,
hemolymphangioma, lymphangitis. Feldsher Akush. 51:27–29. 1986.[(In
Russian)]. PubMed/NCBI
|
|
25
|
Sztaba R and Vondrat W: Thoracic
hemolymphangioma with chylothorax in a newborn infant. Ann Chir
Infant. 6:21–26. 1965.[(In French)]. PubMed/NCBI
|
|
26
|
Fang YF, Qiu LF, Du Y, Jiang ZN and Gao M:
Small intestinal hemolymphangioma with bleeding: a case report.
World J Gastroenterol. 18:2145–2146. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Beninson J and Hurley JP: Hemolymphangioma
in a neonate-a therapeutic problem-case history. Angiology.
39:1043–1047. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Cole DJ, Sood SC and Broomhead IW:
Pulmonary embolism associated with hemolymphangioma of lower
extremity. Plast Reconstr Surg. 63:265–268. 1979. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Gaillard de Collogny L and Delage J:
Cervical hemolymphangioma in a young patient. J Fr Otorhinolaryngol
Audiophonol Chir Maxillofac. 30:469–473. 1981.[(In French)].
PubMed/NCBI
|
|
30
|
Bortolozzi G and Santoni G:
Hemolymphangioma of the uterine cervix associated with early
carcinoma. Minerva Ginecol. 26:722–729. 1974.[(In Italian)].
PubMed/NCBI
|
|
31
|
Nataf P, Martin de Lasalle E, Benomar M,
Gandjbakhch I and Cabrol C: Pericardial hemolymphangioma. Apropos
of a case. Arch Mal Coeur Vaiss. 81:1137–1140. 1988.[(In French)].
PubMed/NCBI
|
|
32
|
Ullik R: On a hemolymphangioma of the
floor of the mouth. Wien Klin Wochenschr. 71:958–960. 1959.[(In
German)]. PubMed/NCBI
|
|
33
|
Canavese F, Cortese MG, Proietti L, et al:
Bulky-pedunculated hemolymphangioma of the esophagus: rare case in
a two-years old girl. Eur J Pediatr Surg. 6:170–172. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Tsonchev P: Hemolymphangioma cavernosum
axillae dextrae. Khirurgiia (Sofiia). 11:869–870. 1958.[(In
Bulgarian)]. PubMed/NCBI
|
|
35
|
Kanaitsuka T, Itani K, Shigeta H, et al: A
case report of giant retroperitoneal hemolymphangioma. Nihon Naika
Gakkai Zasshi. 76:1595–1603. 1987.[(In Japanese)]. View Article : Google Scholar : PubMed/NCBI
|
|
36
|
Houdart R, Palau R, Auclair E, Costa JC
and Potet F: Infected retroperitoneal hemolymphangioma in an adult
with the Klippel-Trenaunay syndrome. Ultrasonic diagnosis. Presse
Med. 15:2161986.[(In French)]. PubMed/NCBI
|
|
37
|
Gossot D, Decazes JM, Sarfati E and Dubost
C: Cystic hemolymphangioma of the adrenal gland. J Chir (Paris).
124:404–405. 1987.[(In French)]. PubMed/NCBI
|
|
38
|
Giacalone PL, Boulot P, Marty M, et al:
Fetal hemangiolymphangioma: a case report. Fetal Diagn Ther.
8:338–340. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
39
|
Daudet M: Reflections apropos of a case of
hepatic hemolymphangioma of the infant. Operation recovery.
Pediatrie. 20:445–451. 1965.[(In French)]. PubMed/NCBI
|
|
40
|
Laufer J and Girsault M: Hemolymphangioma
of the tongue treated with combination embolization-surgery.
Apropos of a case. Rev Stomatol Chir Maxillofac. 87:184–187.
1986.[(In French)]. PubMed/NCBI
|
|
41
|
Bureau Y, Delaire J, Barriere H, Litoux P
and Bureau B: Hemolymphangioma of the tongue. Results of surgical
treatment. Bull Soc Fr Dermatol Syphiligr. 73:422–423. 1966.[(In
French)]. PubMed/NCBI
|
|
42
|
Chanfi M: Hemolymphangioma of the orbit in
a young girl: a clinical observation. J Fr Ophtalmol. 27:1047–1049.
2004.[(In French)]. View Article : Google Scholar : PubMed/NCBI
|
|
43
|
Guillot M, Dufier JL, Pierre-Kahn A,
Nihoul-Fekete C, Lenoir G and Haye C: Hemolymphangioma of the orbit
in children. Arch Fr Pediatr. 40:401–403. 1983.[(In French)].
PubMed/NCBI
|
|
44
|
Wang LC, Krunic AL, Medenica MM, Soltani K
and Busbey S: Treatment of hemorrhagic lymphatic malformation of
the tongue with a pulsed-dye laser. J Am Acad Dermatol.
52:1088–1090. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
45
|
Lu YY and Zhan AL: Imaging diagnosis of CT
and MRI on hemolymphangioma. Zhongguo CT He MRI Za Zhi. 8:51–53.
2010.[(In Chinese)].
|
|
46
|
Fan Z, Li Y, Yan K, et al: Application of
contrast-enhanced ultrasound in the diagnosis of solid pancreatic
lesions—a comparison of conventional ultrasound and
contrast-enhanced CT. Eur J Radiol. 82:1385–1390. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
47
|
Cophignon J, d'Hermies F and Civit T:
Vascular tumors of the orbit. Neurochirurgie. 56:197–212. 2010.[(In
French)]. View Article : Google Scholar : PubMed/NCBI
|
|
48
|
Riquet M, Briere J, Le Pimpec-Barthes F,
et al: Cystic lymphangioma of the neck and mediastinum: are there
acquired forms? Report of 37 cases. Rev Mal Respir. 16:71–79.
1999.[(In French)]. PubMed/NCBI
|
|
49
|
Giron J, Conte J, Chicoisne MP, Mazères F,
Berjaud J and Dahan M: Cervico-mediastinal cystic lymphangioma. Ann
Radiol (Paris). 35:217–221. 1992.[(In French)]. PubMed/NCBI
|
|
50
|
Fontaliran F, Guillois B and Colin A:
Congenital atrioventricular block and maternal lupus erythematosus.
Histologic discovery of tumor of the atrioventricular node. Arch
Mal Coeur Vaiss. 82:609–613. 1989.[(In French)]. PubMed/NCBI
|
|
51
|
Kennedy TL, Whitaker M, Pellitteri P and
Wood WE: Cystic hygroma/lymphangioma: a rational approach to
management. Laryngoscope. 111:1929–1937. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
52
|
Hebra A, Brown MF, McGeehin KM and Ross AJ
III: Mesenteric, omental and retroperitoneal cysts in children: a
clinical study of 22 cases. South Med J. 86:173–176. 1993.
View Article : Google Scholar : PubMed/NCBI
|