Introduction
The question of whether patients with advanced
gastric carcinoma should receive bursa omentalis resection
treatment has long been debated (1,2). However,
the Japanese Classification of Gastric Carcinoma (14th edition)
(4) clearly indicates that, for cases
in which the serosa of the posterior gastric wall has been invaded
by the tumor, a bursa omentalis resection should be performed for
the purpose of cleaning up the tiny planting nidi in the bursa
omentalis (3). In traditional open
surgery, the difficulty of a bursa omentalis resection is low, but
in laparoscopic resection of gastric carcinoma with radical
gastrectomy, it has become one of the difficult points in the
surgery (5,6). Thus, there are no reports regarding
bursa omentalis resection as part of a minimally invasive approach.
Since the first report of laparoscopic distal gastrectomy by Kitano
et al (7) in 1994, this
technique has been widely performed for gastric cancer due to its
advantages of reduced pain, earlier recovery and improved cosmetic
outcome. With the use of laparoscopic technology in the clinical
study of advanced gastric carcinoma, the resection paths and
feasibility of the technique has increasingly become a clinical
issue that requires solving urgently. The present study aimed to
inquire into the skills required for a laparoscopic resection of
the bursa omentalis and lymph node scavenging with radical
gastrectomy, and the feasibility of the technique.
Materials and methods
General data
During the period between January 2012 and January
2012, 18 patients (10 males and 8 females) with advanced gastric
carcinoma received laparoscopic resection of the bursa omentalis
and lymph node scavenging with radical gastrectomy. In Table I, the general clinical characteristics
of the patients, surgical duration, bursa omentalis resection time,
amount of bleeding during surgery, post-operative complications
associated with the surgery, length of hospital stay and number of
lymph nodes scavenged are recorded.
 | Table I.Clinical characteristics of the
patients. |
Table I.
Clinical characteristics of the
patients.
| Characteristic | Value |
|---|
| Number of cases,
n | 18 |
| Gender, n |
|
| Male | 10 |
|
Female | 8 |
| Age, years | 74.6±14.5 |
| Pre-operative T
stage, n |
|
| T2 | 0 |
| T3 | 4 |
| T4 | 14 |
| Surgical duration,
min | 289.3±30.3 |
| Bursa omentalis
resection time, min | 46.1±18.6 |
| Amount of bleeding
during surgery, ml | 35.5±6.5 |
| Length of hospital
stay, days | 9.1±2.1 |
| Lymph nodes
scavenged, n | 25.3±6.2 |
| Post-operative
complications |
|
| Wound
infection | 1 |
| Bowel
obstruction | 1 |
| Urinary
tract infection | 1 |
Trocar and operator's position
The patients were placed in a horizontal supine
position and the trocar was positioned adopting a five-hole method
(the same as for a laparoscopic resection of gastric carcinoma with
radical gastrectomy). The surgeon was positioned to the right side
of the patient.
Laparoscopic resection
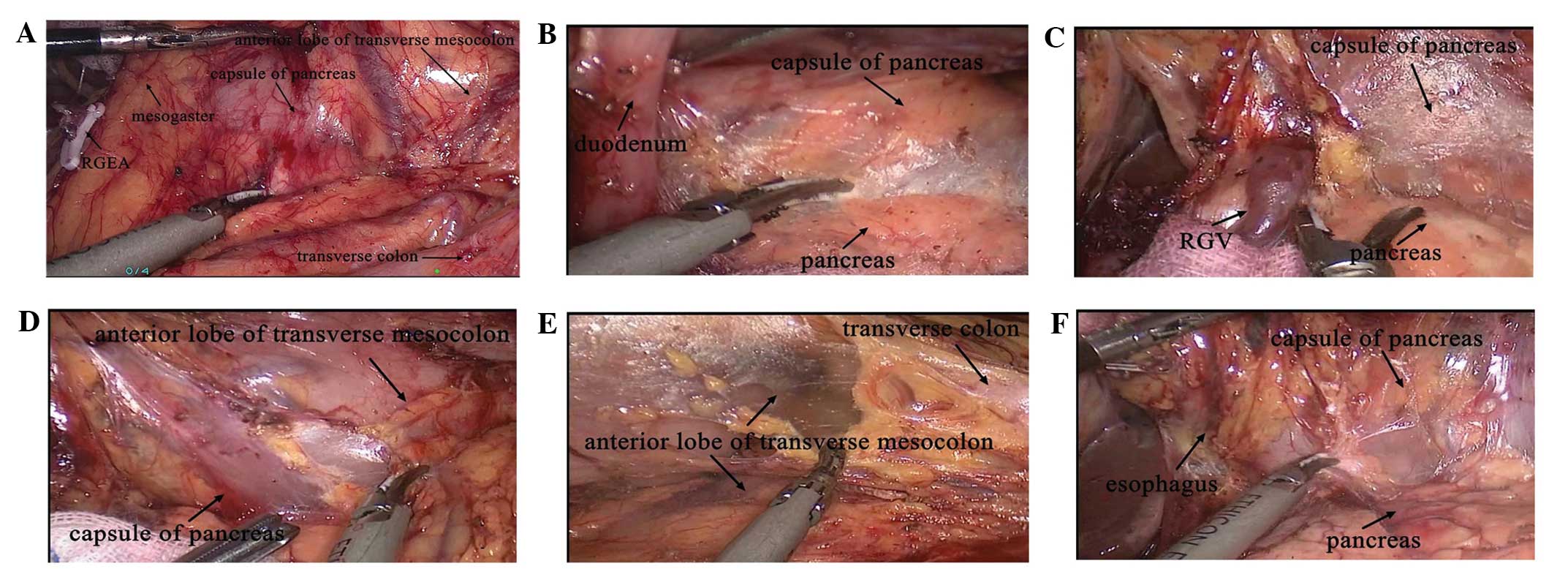
The main surgical steps for the laparoscopic
resection of the bursa omentalis and lymph node scavenging are
shown in Fig. 1.
The first step was to lift up the greater omentum on
the right side of the transverse colon, create clearance between
the transverse mesocolon and distal gastric membrane with an
ultrasound scalpel along the pancreatic head surface, scavenge the
station 6 lymph node, dissect the pancreatic head membrane, create
clearance posterior to the duodenum, scavenge the station 12 and 15
lymph nodes on the right lateral border of bursa omentalis, and
transect the duodenum with a linear scavenging sealer.
In the second step, the assistant lifted and
tightened the distal end of the stomach to the left. The surgeon
dissected the pancreatic head membrane with an ultrasound scalpel,
scavenged the station 8, 9, 7 and 11 lymph nodes upwards, separated
the attachment site of the bursa omentalis and liver, dissected the
anterior lobe of the transverse mesocolon downwards and resected
the greater omentum.
In the third step, if the surgery required a distal
radical gastrectomy, this requirement was met when the pancreatic
capsule was dissected to the middle of the splenic artery and the
anterior lobe of transverse mesocolon was dissected to the left
gastroepiploic artery root (scavenging of station 3 and 1 lymph
nodes). If the surgery required a radical total gastrectomy, six
procedures were followed: Dissection of the pancreas to the hilus
lienis; dissection of the anterior lobe of the transverse mesocolon
to the left gastroepiploic artery root (scavenging of the station 4
lymph nodes); severing of the short gastric vessels on the left of
the bursa omentalis; scavenging of the station 4 lymph nodes and
the splenic hilar lymph nodes (station 10 lymph nodes); scavenging
the station 2 lymph nodes; and removing the whole bursa
omentalis.
Reconstruction of the digestive
tract
Following gastric disassociation and lymph node
scavenging, reconstruction of the digestive tract was completed
laparoscopically. In the surgeries performed with radical total
gastrectomy the reconstruction of the digestive tract was of
esophagojejunal Roux-en-Y type (10 cases). For distal subtotal
gastrectomy, 2 cases adopted the Billroth-I type and 6 cases
adopted the Billroth-II type.
Observation indices
Observation indices used for observing the patients
included: i) Surgical duration; ii) bursa omentalis resection time;
iii) amount of bleeding during surgery; iv) post-operative
complications associated with the surgery; v) length of hospital
stay; vi) number of lymph nodes scavenged; and vii) short-term
follow-up results.
Statistical analysis
Data are presented as mean ± standard deviation or
median with range. All analyses were performed using SPSS software
version 17.0 (SPSS, Inc., Chicago, IL, USA).
Results
All cases received D2 dissection according to the
Japanese Gastric Cancer Association gastric cancer treatment
guidelines (4), and the tumor
location and surgical type are shown in Table II. All patients successfully received
a bursa omentalis resection and lymph node scavenging, and no case
underwent conversion to open surgery. The mean surgical duration
was 289.3±30.3 min, the bursa omentalis resection time was
46.1±18.6 min and the amount of bleeding during surgery was
35.5±6.5 ml for these patients. No cases suffered from
post-operative complications associated with the surgery, such as
pancreatic fistulae, anastomotic fistulae or intestinal
obstructions. The length of hospital stay was 9.1±2.1 days and the
number of lymph nodes scavenged was 25.3±6.2. There were no
complications during the surgery and no patients succumbed. The
short-term follow-up period was a 6 months and no patients
succumbed within this time.
 | Table II.Tumor location and surgical type. |
Table II.
Tumor location and surgical type.
| Parameter | No. of cases |
|---|
| Tumor location |
|
|
Cardia | 3 |
| Gastric
body | 7 |
| Gastric
mucosa | 8 |
| Surgical type |
|
| Total
gastrectomy | 10 |
| Distal
gastrectomy | 8 |
| Proximal
gastric resection | 0 |
| Anastomosis |
|
|
Billroth-I | 2 |
|
Billroth-II | 6 |
|
Roux-en-Y | 10 |
|
Esophagus-stomach | 0 |
Discussion
For a long period of time, in East Asia and
particularly in Japan, bursa omentalis resection has been used to
improve the prognosis of patients with serous invasive carcinoma
(8). When performing an open radical
gastrectomy for the treatment of gastric carcinoma, a bursa
omentalis resection and lymph node scavenging is considered to be
the standard procedure, and open omental resection technology has
been extensively developed (9).
Although, due to the lack of concrete proof, disputes remain over
whether patients can benefit from bursa omentalis resection
clinically, the mid-term evaluation of a prospective, random and
multi-center clinical study (3) in
Japan showed that bursa omentalis resection may aid in increasing
the post-operative survival rate of patients with gastric
carcinoma. Therefore, unless more definite proof is obtained, the
use of bursa omentalis resection will not be stopped. With the
generalization and development of laparoscopic technology, the
safety, possibility of a radical cure, minimally invasive nature
and surgical proficiency of laparoscopic radical gastrectomy for
gastric carcinoma have been confirmed (10,11).
Clinical research shows that it is safe and feasible to perform a
laparoscopic resection of the bursa omentalis and lymph node
scavenging with radical gastrectomy (12), and studies performed in Japan also
indicate that a bursa omentalis resection with laparoscopic radical
gastrectomy that is performed by surgeons who have passed the
learning curve period will not increase the incidence rate of
surgical complications (13). As
laparoscopic radical gastrectomy is at the stage of investigation
and development, in addition to meeting the requirement that the
operator should be skilled and experienced in open bursa omentalis
resection and have well-knit basic skills in using a laparoscope,
attention must also be paid to the construction of the surgical
team. The assistant and camera assistant must have deep
understanding and knowledge on the anatomy of the bursa omentalis.
This type of surgery is demanding of the assistant's skills in
separating the surgical plane at a certain angle, strength and
width, and also is demanding of the camera assistant's skills in
adjusting the view. The operational difficulty in the laparoscopic
resection of the whole bursa omentalis is extremely high and
studies associated with its clinical surgical technology are also
extremely scarce.
Based on the aforementioned background information,
the present study performed an initial study on the safety of a
laparoscopic resection of the bursa omentalis and lymph node
scavenging with radical gastrectomy in treating advanced gastric
carcinoma. Lymph node scavenging technology has become increasingly
well developed, but the laparoscopic resection of the bursa
omentalis remains difficult to a certain extent. Firstly, the
anatomical structure of the bursa omentalis is rather complicated,
consisting of the fascia, vessel and lymphatic duct between the
stomach and other organs, such as the pancreas and transverse
mesocolon. Furthermore, the passage of the vessels is complicated
and the trauma caused by dissection of the bursa omentalis is
large. Resection of the bursa omentalis and lymph node scavenging
should be performed simultaneously and cannot be separated. The
completion of a complete bursa omentalis resection also means the
completion of lymph node scavenging around the stomach. This
requires that the surgeon and the assistant should each have good
knowledge of the surgery and cooperate well with each other.
Meanwhile, they should also be capable of controlling the injury
caused by the surgery. Secondly, the surgical view is not good: In
a traditional open resection of the bursa omentalis, using
multi-point exposing methods (e.g., ‘four-point’ page turning), the
surgeons and their assistants can easily spread apart dense fascial
spaces such as the middle portion of the anterior lobe of the
transverse mesocolon and the capsula pancreatis, but the
laparoscopic surgical team consists of only 2–3 members (partially
due to the use of a mechanical arm to hold the camera). Through the
tacit ‘three-point type’ exposure by the surgeon and the assistant,
the surgical view can be completely exposed, with the surgeon using
only one operational hand to perform the separation and resection
procedures. Therefore, the surgeon must have solid knowledge of
anatomy and a well-developed surgical technique with the
laparoscope. Currently, the method of splenic artery approach lymph
scavenging causes damage to the integrity of the bursa omentalis,
and stripping the outside of the bursa omentalis has become a
necessary way to solve the problem. At the same time, efforts
should be made to seek a method of exposure with the best surgical
view and practical path. In practical surgeries, we have found that
the fascial space on the right side of the anterior lobe of
transverse mesocolon is loose. It is easy for the surgeon to stand
on the right side of the patient to separate the space and scavenge
the hepatoduodenal ligament lymph on the right side of the bursa
omentalis along the mesogastrium, mesocolon and pancreatic head.
Therefore, with the duodenum transected, the assistant can retract
the stomach cephalad, and the right side of bursa omentalis may
easily be exposed (14). Meanwhile,
the surgeon performs ‘apple-dissecting’ surgery to complete
stripping and lymph scavenging from the right side to the left
side. The difficult points in the surgical process are mainly
embodied by the three sections as follows: i) The middle portion of
the anterior lobe of the transverse mesocolon, where the fascial
spaces are dense and the spaces on the left side are loose: Fusion
with the posterior lobe serosa of the greater omentum extends to
the back side of the pancreas tail and spleen. When using the
‘three-point’ type exposure, the anterior lobe of the transverse
mesentery and the transverse colon are spread to form a 45° angle.
The surgeon should perform the procedure with patience and the
camera assistant should keep a suitable distance. ii) The upper
side wall: The left hepatic lobe and the caudate lobe are pulled
open with a hanging maneuver method under the laparoscope,
carefully dissecting away two layers of serosa in the upper wall of
the bursa omentalis along the left side of the hepatoduodenal
ligament and the bursa omentalis Winslow hole, transiting the back
layer and the caudate lobe of the liver to the left until the crura
of the diaphragm on the right side, dissecting upwards along the
upper part of the vena cava ligament to the cardia and the back of
the abdominal segment of the esophagus, and downwards to the cauda
pancreatis capsule (the back wall of bursa omentalis is the cauda
pancreatis capsule and is easily dissected away) and dissecting the
posterior lobe serosa of the bursa omentalis. iii) The left side
wall: Dissection is continued to the left towards the peritoneum of
the left adrenal gland, left kidney, gastrolienal ligament, spleen,
splenorenal ligament, stomach esophagus and hepatic ligaments along
the capsula pancreatis, and the fusion fascia, formed by the
capsula pancreatis, the serosa under the spleen and the mesocolon,
are totally resected.
Therefore, in clinical practice, the compartments
and anatomical plane should be observed carefully, in order to
avoid the bleeding risks caused by mesenteric vessels, injury of
the pancreas and the surgical wound. In the present study, none of
the patients experienced surgery-associated complications (e.g.,
pancreatic fistulae, anastomotic fistulae or intestinal
obstruction) following the procedure, which shows that the surgical
technology is safe and feasible. However, as the number of cases is
not large enough, the significance and long-term effects of
laparoscopic resection of the bursa omentalis and lymph node
scavenging with radical gastrectomy call for further study.
References
|
1
|
Cao F, Li J, Li A, Fang Y and Li F:
One-stage laparoscopic resection for a large gastric
gastrointestinal stromal tumor and synchronous liver metastases
following preoperative imatinib therapy: A case report. Oncol Lett.
5:1233–1236. 2013.PubMed/NCBI
|
|
2
|
Glehen O, Passot G, Villeneuve L, Vaudoyer
D, Bin-Dorel S, Boschetti G, Piaton E and Garofalo A: GASTRICHIP:
D2 resection and hyperthermic intraperitoneal chemotherapy in
locally advanced gastric carcinoma: a randomized and multicenter
phase III study. BMC Cancer. 14:1832014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Fujita J, Kurokawa Y, Sugimoto T,
Miyashiro I, Iijima S, Kimura Y, Takiguchi S, Fujiwara Y, Mori M
and Doki Y: Survival benefit of bursectomy in patients with
resectable gastric cancer: Interim analysis results of a randomized
controlled trial. Gastric Cancer. 15:42–48. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Japanese Gastric Cancer Association, .
Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric
Cancer. 14:113–123. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Hallet J, Labidi S, Bouchard-Fortier A,
Clairoux A and Gagné JP: Oncologic specimen from laparoscopic
assisted gastrectomy for gastric adenocarcinoma is comparable to
D1-open surgery: The experience of a Canadian centre. Can J Surg.
56:249–255. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yang Y, Li J, Mao S and Zhu H: Comparison
of immunohistology using pan-CK and EMA in the diagnosis of lymph
node metastasis of gastric cancer, particularly micrometastasis and
isolated tumor cells. Oncol Lett. 5:768–772. 2013.PubMed/NCBI
|
|
7
|
Kitano S, Iso Y, Moriyama M and Sugimachi
K: Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc
Endosc. 4:146–148. 1994.PubMed/NCBI
|
|
8
|
Epstein DM, Capeci CM and Rokito AS:
Patella tendon rupture after arthroscopic resection of the
prepatellar bursa - a case report. Bull NYU Hosp Jt Dis.
68:307–310. 2010.PubMed/NCBI
|
|
9
|
Brito AM, Sarmento BJ, Mota ED, Fraga AC
Jr, Campoli PM, Milhomem LM and da Mota OM: Prognostic role of
positive peritoneal cytology in patients with resectable gastric
cancer. Rev Col Bras Cir. 40:121–126. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Huang JL, Wei HB, Zheng ZH, Chen TF, Huang
Y, Wei B, Guo WP and Hu BG: Comparison of laparoscopy-assisted
distal gastrectomy with open gastrectomy for advanced gastric
cancer. Zhonghua Wei Chang Wai Ke Za Zhi. 15:615–617. 2012.(In
Chinese). PubMed/NCBI
|
|
11
|
Wang Y, Xie Y, Wu X, Li L, Ma Y and Wang
X: Laparoscopic management of pedicle torsion of adnexal cysts.
Oncol Lett. 5:1707–1709. 2013.PubMed/NCBI
|
|
12
|
Katai H, Sasako M, Fukuda H, Nakamura K,
Hiki N, Saka M, Yamaue H, Yoshikawa T and Kojima KJCOG Gastric
Cancer Surgical Study Group: Safety and feasibility of
laparoscopy-assisted distal gastrectomy with suprapancreatic nodal
dissection for clinical stage I gastric cancer: A multicenter phase
II trial (JCOG 0703). Gastric Cancer. 13:238–244. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Imamura H, Kurokawa Y, Kawada J, Tsujinaka
T, Takiguchi S, Fujiwara Y, Mori M and Doki Y: Influence of
bursectomy on operative morbidity and mortality after radical
gastrectomy for gastric cancer: Results of a randomized controlled
trial. World J Surg. 35:625–630. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Yu J, Hu Y, Chen T, Mou T, Cheng X and Li
G: Laparoscopic distal gastrectomy with D2 dissection for advanced
gastric cancer. Chin J Cancer Res. 25:474–476. 2013.PubMed/NCBI
|