Introduction
Follicular lymphoma is the most common subtype of
indolent non-Hodgkin's lymphoma. Widespread nodal involvement is a
typical presentation of this disease, with the majority of patients
presenting with Ann Arbor stage III or IV, whereas only 5–10% of
patients present with early stage I or II (1–3).
Follicular lymphoma arising in the intestine has recently been
drawing attention for its distinct clinical features, which are
different from their nodal counterpart. Several studies have
suggested that the majority of patients with intestinal follicular
lymphoma present with localized disease and show favorable clinical
courses (3–5).
Intestinal follicular lymphomas were initially
introduced as a disease predominantly involving the duodenum
(6). The representative macroscopic
features of the duodenal lesions are multiple small, whitish
polypoid lesions (5). The detection
of such duodenal lesions by esophagogastroduodenoscopy is the
initial diagnostic clue in the cases of the majority of the
patients with this disease entity. Since the development of novel
enteroscopy devices such as double-balloon enteroscopy and video
capsule enteroscopy, recent studies have revealed the frequent
involvement of the jejunum and ileum in these patients. Among
follicular lymphoma patients presenting with intestinal
involvement, the reported percentage of cases with multiple
follicular lymphoma lesions in the jejunum and/or ileum has ranged
from 66.7 to 100% (3,7–11).
These results emphasize the importance of
enteroscopy examinations to precisely evaluate the extent of the
intestinal lesions in follicular lymphoma patients. However, the
majority of the previous studies were conducted in a single
tertiary-care center, and to the best of our knowledge, the number
of patients with this disease entity who underwent enteroscopy
examinations in actual clinical settings has never been determined.
A retrospective multicenter survey was therefore conducted to
reveal the present status of enteroscopy examinations among
follicular lymphoma patients presenting with intestinal
involvement. The purposes of the present study were to determine
the current state of enteroscopy examinations, including the
performance rate, and to determine the prevalence of small
intestinal lesions in a patient population in Japan.
Patients and methods
Patients
A database search performed at the Department of
Pathology at the Okayama University Graduate School of Medicine,
Dentistry and Pharmaceutical Sciences (Okayama, Japan) identified
110 follicular lymphoma patients with gastrointestinal involvement
who were treated at Okayama University Hospital or one of 16
collaborating institutions (listed in the Acknowledgements section)
between July 1990 and October 2013. A subset of the 110 patients
examined also participated in a number of our previous studies
(4,6,12–19).
The diagnosis of follicular lymphomas was made
according to World Health Organization (WHO) classifications
(1,20). A histological diagnosis was based on
morphological and immunophenotypical analyses of endoscopically
biopsied specimens or surgically resected specimens.
Histopathological grading was also determined according to WHO
criteria (1). Patients with grade 3
follicular lymphoma were excluded from this study since these cases
are generally managed based on treatment strategies established for
diffuse large B-cell lymphomas (1).
Clinical data regarding the patients' endoscopic, radiological and
biological examinations were obtained from retrospectively reviewed
clinical records. The Lugano staging system for the classification
of gastrointestinal lymphoma was used to determine each patient's
clinical stage (21,22).
The present study was approved by the Ethical
Committee of the Okayama University Hospital and adhered to the
Declaration of Helsinki.
Analyses
Based on the clinical records of the enrolled
patients, the patients were divided into two groups: The Ent group
was composed of the patients who underwent any type of enteroscopy,
such as per oral/per anal double-balloon enteroscopy and video
capsule enteroscopy, and the No-Ent group was comprised of the
patients who had never undergone enteroscopy. First, to determine
the prevalence of follicular lymphoma lesions in the small
intestine and their endoscopic features, the study evaluated the
Ent group patients' modalities of enteroscopy performed, the
macroscopic appearance of the lesions and the affected regions of
the small intestine. Subsequently, to identify potential factors
affecting the performance rate of enteroscopy among follicular
lymphoma patients with gastrointestinal involvement, patient
gender, age at lymphoma diagnosis, histopathological grade,
clinical stage, the date of the initial diagnosis and the annual
volume of enteroscopy examinations at the institution where the
patient was treated were evaluated.
The annual volume of enteroscopy is presented as the
total number of enteroscopy examinations performed at the
participating institution in 2013. The 17 institutions were then
divided into the following four groups in accordance with the
annual number of enteroscopies performed: Low-volume institutions,
0–25 examinations/year (9 institutions); middle-volume
institutions, 26–50 examinations/year (3 institutions); high-volume
institutions, 51–100 examinations/year (3 institutions); and
ultra-high volume institutions, >101 examinations/year (2
institutions).
Statistical analysis
For the comparisons of the two groups, statistical
analyses, including t-tests, χ2 tests and F-tests were
performed using JMP 8.0.1 software (SAS Institute, Cary, NC, USA).
P<0.05 was considered to indicate a statistically significant
difference.
Results
Among the 110 patients, 34 patients (30.9%) had
undergone one or more enteroscopy examinations at the initial
diagnostic work-up and/or during the follow-up period (Table I). A total of 21 patients underwent
video capsule enteroscopy, 17 patients underwent double-balloon
enteroscopy, 1 patient underwent per-oral single balloon
enteroscopy and 1 patient underwent per-oral push enteroscopy. A
total of 6 patients underwent a video capsule enteroscopy plus a
double-balloon enteroscopy. Of the 10 patients in whom the small
intestine was investigated only by double-balloon enteroscopy, 3
underwent only a per-oral enteroscopy, 2 underwent only a per-anal
enteroscopy and the remaining 6 underwent a per-oral plus a
per-anal enteroscopy. Eventually, the entire length of the small
intestine was examined in 28 patients by video capsule enteroscopy
and/or the combination of per-oral plus per-anal double-balloon
enteroscopy.
 | Table I.Prevalence and endoscopic features of
follicular lymphoma lesions in the small intestine |
Table I.
Prevalence and endoscopic features of
follicular lymphoma lesions in the small intestine
| Feature | No. of patients |
|---|
| Total no. of
patients | 34 |
| Modality of
enteroscopy |
|
|
VCE | 21 |
|
DBE | 17 |
|
SBE | 1 |
| Push
enteroscopy | 1 |
| Affected regions of
the small intestine |
|
| Jejunum
only | 16 |
| Ileum
only | 2 |
| Jejunum
plus ileum | 6 |
|
None | 10 |
| Macroscopic
appearance |
|
| Whitish
granulesa | 22 |
|
Ulcer | 2 |
|
Stenosis | 2 |
|
Ulcerative tumor | 1 |
| Wall
thickening | 1 |
The enteroscopy examinations revealed only jejunal
involvement in 16 patients and only ileal involvement in 2
patients. A total of 6 patients presented with small intestinal
lesions in the jejunum plus the ileum, whereas 10 patients
exhibited no involvement in the small intestine. Finally 24/34
patients (70.6%) exhibited involvement in the jejunum and/or ileum.
Among the 34 patients who underwent enteroscopy, 32 patients
(94.1%) presented with duodenal involvement and 22/32 patients
(68.8%) with involvement in the jejunum and/or ileum.
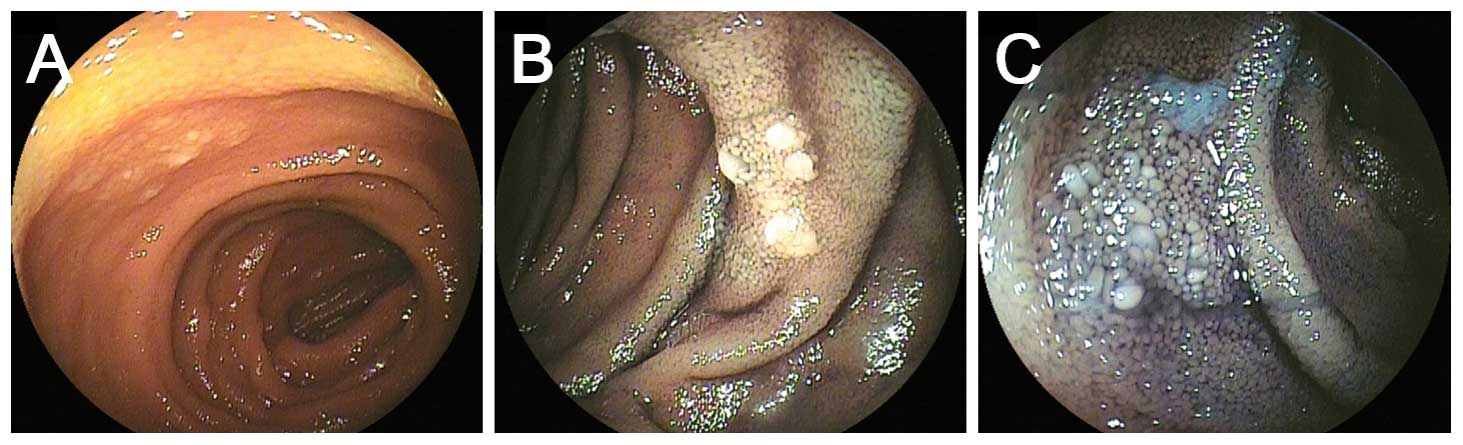
In terms of the macroscopic appearance, 22 patients
showed whitish granules in the jejunum and/or ileum (Figs. 1 and 2).
Such whitish granules, which are quite similar to the well-known
features observed in duodenal follicular lymphoma (1,5), were the
only presenting feature in 20 patients. In the remaining 4
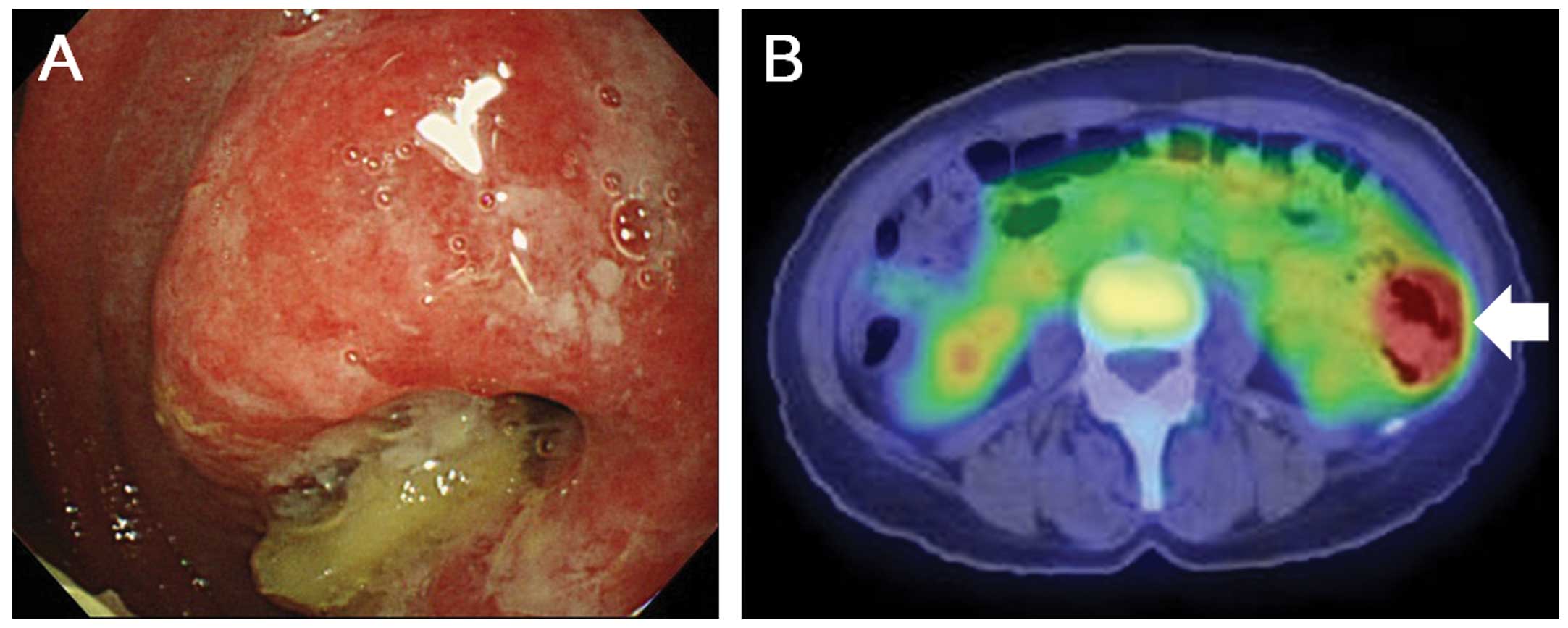
patients, 1 presented with an ulcerative tumor (Fig. 3), another with luminal stenosis, the
third with whitish granules, wall thickening and ulcers, and the
fourth with whitish granules, luminal stenosis and ulcers.
The patients were subdivided into the following two
groups according to the status of their small intestinal
examinations: The Ent group, i.e., the patients who underwent
enteroscopy (n=34), and the No-Ent group, i.e., the patients who
did not undergo an enteroscopy (n=76). The clinical characteristics
of each group are provided in Table
II. The comparisons of the two groups revealed that patient age
(P=0.886), gender (P=1.000), histological grade (P=0.674) and
clinical stage (I and II1 vs. II2 and IV; P=0.663) did not differ
significantly between the groups, whereas more patients diagnosed
in recent years (since 2008) underwent enteroscopy examinations
compared with the patients diagnosed previously (in 2007 or
earlier; P<0.001). Additionally, more patients treated at an
ultra-high volume institution were examined by enteroscopy compared
with the patients treated at other institutions (low-, middle- and
high-volume institutions; P=0.003).
 | Table II.Clinical backgrounds of the Ent and
No-Ent patients. |
Table II.
Clinical backgrounds of the Ent and
No-Ent patients.
| Parameter | Enteroscopy | No enteroscopy | P-value |
|---|
| No. of
patients | 34 | 76 |
|
| Male/female, n | 15/19 | 34/42 | 1.000 |
| Age at diagnosis of
FL, years | 63.0±2.0 | 63.4±1.4 | 0.886 |
| WHO grade, n |
|
| 0.674 |
| Grade
1 | 31 | 72 |
|
| Grade
2 | 3 | 4 |
|
| Lugano system
staging, n |
|
| 0.663 |
| I | 19 | 39 |
|
|
II1 | 5 | 10 |
|
|
II2 | 3 | 4 |
|
| IV | 7 | 23 |
|
| Date of initial
diagnosis, n |
|
|
<0.001a |
|
1990–2003 | 2 | 20 |
|
|
2004–2007 | 1 | 21 |
|
|
2008-present | 31 | 35 |
|
| Annual volume of
enteroscopy at the institution, n |
|
| 0.003b |
|
0–25 | 6 | 27 |
|
|
26–50 | 3 | 6 |
|
|
51–100 | 3 | 17 |
|
|
101+ | 22 | 26 |
|
Discussion
The primary purpose of the present study was to
investigate the performance rate of enteroscopy in follicular
lymphoma patients presenting with gastrointestinal involvement. To
the best of our knowledge, this study is the first to reveal the
performance rate in actual clinical settings. In this study, 34/110
patients (30.9%) underwent enteroscopy examinations. The
statistical analysis disclosed that the small intestines were more
frequently investigated in patients diagnosed in recent years
(since 2008) and in patients treated at the institutions where a
considerable number of enteroscopy examinations was performed (≥101
examinations/year). Conversely, the number of enteroscopy
examinations was fewer in patients diagnosed in earlier years,
particularly in 2007 or prior to this, and in patients treated at
institutions where <100 examinations were performed per
year.
In Japan, double-balloon enteroscopy was introduced
in the fall of 2003 (23) and video
capsule enteroscopy was introduced in the fall of 2007 (24). It is likely that the availability of
enteroscopy devices at the initial staging of follicular lymphoma
patients affected the performance rate of the enteroscopic
examinations. Another possible reason is that the high prevalence
of the intestinal lesions was recognized in 2008. However, it is
noteworthy that enteroscopy examinations were not performed at the
initial work-up or even in the follow-up period in 41 of the 44
patients (93.2%) who were diagnosed in 2007 or earlier.
As aforementioned, previous studies documented that
the jejunum and/or ileum was affected in 66.7 to 100% of follicular
lymphoma patients presenting with intestinal involvement (3,4,7–11). The
present study showed a similar prevalence, as the jejunum and/or
ileum was affected in 24/34 patients (70.6%). Consequently, all the
follicular lymphoma patients presenting with intestinal involvement
can be regarded as candidates for enteroscopy examinations,
regardless of the availability of enteroscopy devices in the
institution and regardless of the phase of the patient's clinical
course (i.e., at the initial work-up or during follow-up
period).
In the present study, the jejunum and/or ileum was
affected in 24 patients. Among them, 20 patients (83.3%) developed
whitish granules as the only presenting feature. Other studies have
described the small intestinal lesions observed by enteroscopy as
‘multiple white nodules’, ‘multiple small granules’, ‘small whitish
polyps’, ‘whitish granular lesions’ or ‘polypoid lesions’ (5,8,9,11). The
present study and previous reports indicated that the whitish
granules, which are similar to the typical endoscopic features of
duodenal follicular lymphoma, are the predominant morphology of the
jejunal and ileal involvement as well. Nakamura et al noted
that the jejunal lesions are easily identified as follicular
lymphoma lesions as physiological lymphoid structures rarely exist
in the jejunum, whereas ileal lesions are occasionally difficult to
differentiate from physiological lymphoid follicles (11). In such cases, histological
examinations with the immunostaining of biopsied specimens are
required for an accurate diagnosis.
The present study also found that 4 patients
exhibited macroscopic features other than whitish granules, namely
ulcerative lesions, luminal stenosis, tumorous lesions accompanied
by ulcers and/or wall thickening. These morphologies were probably
formed during the progression of the disease and as a result of an
increased number of infiltrated lymphoma cells within the small
intestinal wall (7,25). Biopsy examinations are generally
useful for such lesions showing atypical macroscopic features, not
only for the accurate pathological diagnosis of follicular
lymphomas, but also for the detection of the histological
transformation from grades 1 and 2 to grade 3, which generally
facilitates the prompt initiation of treatment.
No standardized treatment strategies have been
established for limited-stage gastrointestinal follicular lymphoma.
The initial treatment may be radiotherapy, systemic chemotherapy,
monoclonal antibody monotherapy, a combination of these therapies
or a ‘watch and wait’ policy (3–5). Several
studies have stated that the watch and wait strategy can be an
acceptable initial approach due to the indolent nature of this
disease entity (2,3,12,26–28). On
the other hand, for limited-stage follicular lymphoma of nodal
origin, radiotherapy is recommended as the preferred treatment with
curative potential (2,29). In the study by Schmatz et al,
it was reported that all the patients with primary intestinal
follicular lymphoma treated by radiotherapy alone (n=19)
experienced complete remission, and none of these patients
developed a local recurrence during a median follow-up time of 37
months (3). Radiotherapy may thus be
one of the treatment options for limited-stage gastrointestinal
follicular lymphoma, as well as for nodal cases. In such
situations, surveillance of the jejunum and ileum prior to local
treatment is particularly vital, since the majority of treatment
failures occur outside the involved field of radiotherapy (30).
At the present time, double-balloon enteroscopy and
video capsule enteroscopy are the two major devices that enable the
direct visualization of the entire length of the small intestines.
Video capsule enteroscopy is more convenient for patients than
double-balloon enteroscopy; the capsule-type device is easily
swallowed, and the full length of the small intestines can be
examined at a single examination session. Moreover, sedation and
exposure to X-ray is not required during a video capsule
enteroscopy procedure. On the other hand, although the
double-balloon enteroscopy generally requires sedation, exposure to
X-rays, and per-oral and per-anal examinations to observe the
entire small intestine, it provides the great advantage of biopsy
sampling. A biopsy is particularly valuable for the diagnostic
work-up of ileal lesions of follicular lymphoma and for the
detection of histological transformation, as aforementioned.
The results of the present study revealed that the
majority of the patients (76/110, 69.1%) had not undergone
enteroscopy examinations at the initial work-up and/or in the
follow-up period, despite the high prevalence of small intestinal
lesions among these patients. At the present time, the clinical
significance of enteroscopy examinations in follicular lymphoma
patients remains a subject of debate, as it has not been revealed
whether or not small intestinal lesions detected by enteroscopy
affect the prognoses of follicular lymphoma patients. We believe
that, in follicular lymphoma patients presenting with
gastrointestinal involvement (particularly in patients at limited
stages), the entire gastrointestinal tract should be screened by
video-capsule enteroscopy, esophagogastroduodenoscopy and
colonoscopy at the initial diagnostic work-up.
Double-balloon enteroscopy is required to take
biopsy samples in cases of lesions with atypical morphology or
ileal lesions mimicking physiological lymphoid follicles, in order
to make an accurate pathological diagnosis and to detect the
histological transformation. We contend that this policy is
acceptable, as the histological transformation to grade 3
follicular lymphoma generally requires the prompt initiation of
treatment. Other topics to debate concerning enteroscopy
examinations include whether enteroscopy should be repeated during
the follow-up period and whether a biopsy is required at each
enteroscopy examination to screen for transformation. Further
studies should address these questions.
The present study has certain limitations. First,
among the 34 patients who underwent enteroscopy, 24 patients
(70.6%) presented with jejunal and/or ileal involvement, but not
all of the 34 patients had the entire small intestine examined. For
example, 1 patient underwent per-oral push enteroscopy, 3 patients
underwent per-oral enteroscopy only, and two patients underwent
only a per-anal enteroscopy. As a result, an underestimation of the
prevalence of small intestinal lesions may have occurred. Second,
the enteroscopy examinations were performed under different
conditions, since the patients were treated at various
institutions. It is possible that differences in methodology among
the participating institutions affected the detection of small
intestinal lesions.
In conclusion, this multicenter survey revealed that
34/110 (30.9%) follicular lymphoma patients presenting with
intestinal involvement underwent enteroscopy examinations, and that
jejunal and/or ileal involvement was frequently identified (24/34
patients, 70.6%). The clinical significance of precisely evaluating
the extent of the intestinal lesions by enteroscopy should be
determined hereafter.
Acknowledgements
The authors would like to thank the following 16
collaborating institutions for providing the database information:
Okayama Saiseikai General Hospital, Okayama; Tsuyama Chuo Hospital,
Tsuyama; Mitoyo General Hospital, Kanonji; Kagawa Prefectural
Central Hospital, Takamatsu; Sumitomo Besshi Hospital, Niihama;
Okayama City Hospital, Okayama; Hiroshima City Hospital, Hiroshima;
Kagawa Rosai Hospital, Marugame; Chugoku Central Hospital,
Fukuyama; Fukuyama City Hospital, Fukuyama; Japanese Red Cross
Okayama Hospital, Okayama; St. Mary's Hospital, Himeji; Iwakuni
Clinical Center, Iwakuni; Ako Central Hospital, Ako; Onomichi
Municipal Hospital, Onomichi; and Kitagawa Hospital, Okayama,
Japan.
References
|
1
|
Harris NL, Swerdlow SH, Jaffe ES, et al:
Follicular lymphomaWHO Classification of Tumours of Haematopoietic
and Lymphoid Tissues. Swerdlow SH, Campo E, Harris NL, et al: IARC
press; Lyon, France: pp. 220–226. 2008
|
|
2
|
Dreyling M, Ghielmini M, Marcus R, Salles
G and Vitolo UESMO Guidelines Working Group: Newly diagnosed and
relapsed follicular lymphoma: ESMO Clinical Practice Guidelines for
diagnosis, treatment and follow-up. Ann Oncol. 22 (suppl
6):vi59–vi63. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Schmatz AI, Streubel B, Kretschmer-Chott
E, et al: Primary follicular lymphoma of the duodenum is a distinct
mucosal/submucosal variant of follicular lymphoma: A retrospective
study of 63 cases. J Clin Oncol. 29:1445–1451. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Takata K, Okada H, Ohmiya N, et al:
Primary gastrointestinal follicular lymphoma involving the duodenal
second portion is a distinct entity: A multicenter, retrospective
analysis in Japan. Cancer Sci. 102:1532–1536. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yamamoto S, Nakase H, Yamashita K, et al:
Gastrointestinal follicular lymphoma: Review of the literature. J
Gastroenterol. 45:370–388. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yoshino T, Miyake K, Ichimura K, et al:
Increased incidence of follicular lymphoma in the duodenum. Am J
Surg Pathol. 24:688–693. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Higuchi N, Sumida Y, Nakamura K, et al:
Impact of double-balloon endoscopy on the diagnosis of jejunoileal
involvement in primary intestinal follicular lymphomas: A case
series. Endoscopy. 41:175–178. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Akamatsu T, Kaneko Y, Ota H, Miyabayashi
H, Arakura N and Tanaka E: Usefulness of double balloon enteroscopy
and video capsule endoscopy for the diagnosis and management of
primary follicular lymphoma of the gastrointestinal tract in its
early stages. Dig Endosc. 22:33–38. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kodama M, Kitadai Y, Shishido T, et al:
Primary follicular lymphoma of the gastrointestinal tract: A
retrospective case series. Endoscopy. 40:343–346. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Nakamura S, Matsumoto T, Umeno J, et al:
Endoscopic features of intestinal follicular lymphoma: The value of
double-balloon enteroscopy. Endoscopy. 39 (suppl 1):E26–E27. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Nakamura M, Ohmiya N, Hirooka Y, et al:
Endoscopic diagnosis of follicular lymphoma with small-bowel
involvement using video capsule endoscopy and double-balloon
endoscopy: A case series. Endoscopy. 45:67–70. 2013.PubMed/NCBI
|
|
12
|
Takata K, Sato Y, Nakamura N, et al:
Duodenal and nodal follicular lymphomas are distinct: The former
lacks activation-induced cytidine deaminase and follicular
dendritic cells despite ongoing somatic hypermutations. Mod Pathol.
22:940–949. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Takata K, Sato Y, Nakamura N, et al:
Duodenal follicular lymphoma lacks AID but expresses BACH2 and has
memory B-cell characteristics. Mod Pathol. 26:22–31. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Takata K, Tanino M, Ennishi D, et al:
Duodenal follicular lymphoma: Comprehensive gene expression
analysis with insights into pathogenesis. Cancer Sci. 105:608–615.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Sato Y, Ichimura K, Tanaka T, et al:
Duodenal follicular lymphomas share common characteristics with
mucosa-associated lymphoid tissue lymphomas. J Clin Pathol.
61:377–381. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Iwamuro M, Okada H, Takata K, et al:
Diagnostic role of 18F-fluorodeoxyglucose positron emission
tomography for follicular lymphoma with gastrointestinal
involvement. World J Gastroenterol. 18:6427–6436. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Takeuchi K, Iwamuro M, Imagawa A, et al:
Primary follicular lymphoma of the duodenum with erosions as
atypical macroscopic features. Case Rep Med.
2012:5826072012.PubMed/NCBI
|
|
18
|
Iwamuro M, Okuda M, Yumoto E, et al:
Magnifying endoscopy for intestinal follicular lymphoma is helpful
for prompt diagnosis. Gut Liver. 7:258–261. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Iwamuro M, Shinagawa K, Okada H, Takata K,
Yoshino T and Yamamoto K: Elevated soluble IL-2 receptor levels
correlate with tumor bulk of follicular lymphomas with intestinal
involvement. Clin Biochem. 47:191–195. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Harris NL, Jaffe ES, Diebold J, et al:
World Health Organization classification of neoplastic diseases of
the hematopoietic and lymphoid tissues: Report of the Clinical
Advisory Committee meeting-Airlie House, Virginia, November 1997. J
Clin Oncol. 17:3835–3849. 1999.PubMed/NCBI
|
|
21
|
Zucca E, Roggero E, Bertoni F and Cavalli
F: Primary extranodal non-Hodgkin's lymphomas. Part 1
Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol.
8:727–737. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Rohatiner A, d'Amore F, Coiffier B, et al:
Report on a workshop convened to discuss the pathological and
staging classifications of gastrointestinal tract lymphoma. Ann
Oncol. 5:397–400. 1994.PubMed/NCBI
|
|
23
|
Yamamoto H, Yano T, Kita H, Sunada K, Ido
K and Sugano K: New system of double-balloon enteroscopy for
diagnosis and treatment of small intestinal disorders.
Gastroenterology. 125:1556–1557. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Nakamura M, Ohmiya N, Niwa Y and Goto H:
Endoscopic examination for the small bowel-video capsule endoscopy
and double balloon enteroscopy. Nihon Rinsho. 66:1253–1258.
2008.(In Japanese). PubMed/NCBI
|
|
25
|
Iddan G, Meron G, Glukhovsky A and Swain
P: Wireless capsule endoscopy. Nature. 405:4172000. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Misdraji J, Harris NL, Hasserjian RP,
Lauwers GY and Ferry JA: Primary follicular lymphoma of the
gastrointestinal tract. Am J Surg Pathol. 35:1255–1263. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Campbell BA, Voss N, Woods R, et al:
Long-term outcomes for patients with limited stage follicular
lymphoma: Involved regional radiotherapy versus involved node
radiotherapy. Cancer. 116:3797–3806. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Yanai S, Nakamura S, Takeshita M, et al:
Translocation t(14;18)/IGH-BCL2 in gastrointestinal follicular
lymphoma: Correlation with clinicopathologic features in 48
patients. Cancer. 117:2467–2477. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Mac Manus MP and Hoppe RT: Is radiotherapy
curative for stage I and II low-grade follicular lymphoma? Results
of a long-term follow-up study of patients treated at Stanford
University. J Clin Oncol. 14:1282–1290. 1996.PubMed/NCBI
|
|
30
|
Gustavsson A, Osterman B and
Cavallin-Ståhl E: A systematic overview of radiation therapy
effects in non-Hodgkin's lymphoma. Acta Oncol. 42:605–619. 2003.
View Article : Google Scholar : PubMed/NCBI
|