Introduction
Mesenchymal chondrosarcoma (MC) is a rare neoplasm,
constituting ~1% of all chondrosarcomas (1). Almost 24% of cases of this rare tumor
originate from an extraskeletal site, and the predominant
extraosseous site is the head and neck region, followed by the
extremities and trunk (2). MC cases
that arise in the kidney are extremely rare and, to the best of our
knowledge, only seven cases have previously been reported in the
literature (2–8). Wilms' tumor is the most common type of
renal malignancy in children. Classically, a radical nephrectomy
for Wilms’ tumor has been recommended as the standard option
(9).
The present study describes the eighth case of
primary renal MC, initially misdiagnosed as Wilm's tumor, which
presented with a large right renal mass with hemorrhage and a
second mass with calcification in the left renal pelvis. To the
best of our knowledge, the present case is the first MC with
bilateral kidney invasion and calcification in the renal
pelvis.
Case report
A 17-year-old male presented with sudden severe pain
in the right flank and high fever, and was admitted to the Shenzhen
People's Hospital (Shenzhen, China) in May 2014. Laboratory tests
were performed and the results were as follows: White blood cell
(WBC) count, 11.08×109/l (normal,
4–10×109/l); neutrophilic granulocyte percentage (N%),
80.1% (normal, 50–70%); red blood cell (RBC) count,
5.64×1012/l (normal, 4.0–5.5×1012/l);
hemoglobin (HBG) level, 156 g/l (normal, 120–160 g/l); aspartate
aminotransferase (AST) level, 243 U/l (normal, 0–40 U/l); and
alanine aminotransferase (ALT) level, 201 U/l (normal, 0–40 U/l).
Imaging studies using ultrasonography and abdominal computerized
tomography (CT) indicated a right 10-cm heterogeneous renal mass
and calcification in the left renal pelvis. The patient was then
diagnosed with a right renal tumor with hemorrhage and a left renal
pelvis calculus, and transferred to the Peking University Shenzhen
Hospital (Shenzhen, China) for further treatment. Physical
examination demonstrated percussion pain over the right kidney
region. Laboratory tests were performed and demonstrated the
following levels: WBC count, 13.08×109/l; N%, 82.3%; RBC
count, 5.06×1012/l; and HBG level, 145 g/l. Tumor
markers, such as α-fetoprotein, urinalysis and kidney function were
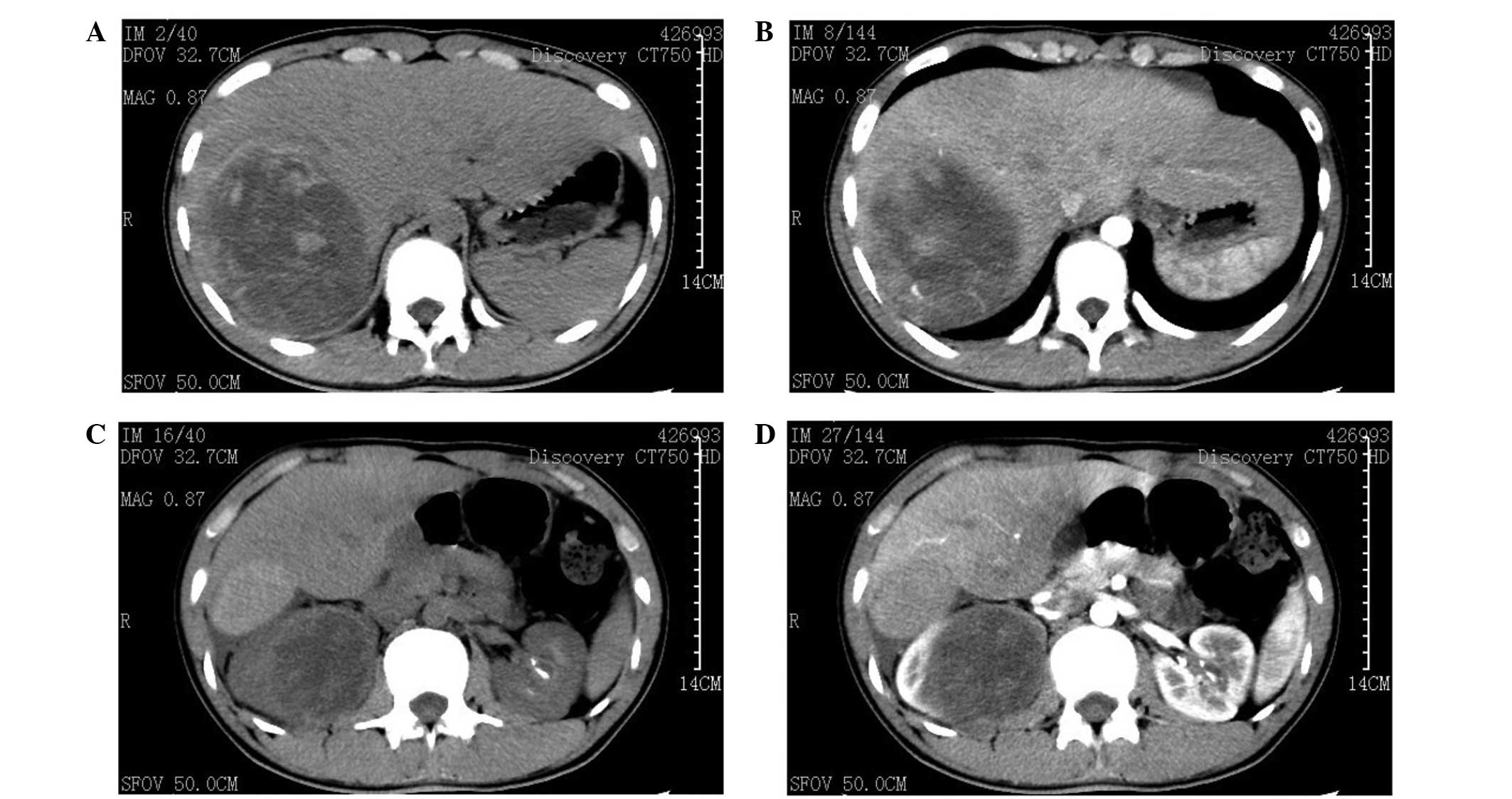
within the normal range. Enhanced CT scans demonstrated a large
soft heterogeneous mass (7.8×9.5×15 cm) located between the liver
and right kidney with no clear demarcation (Fig. 1A). The CT number was 25–64 Hu and no
enhancement was observed at the artery phase (Fig. 1B). The shape and size of the left
kidney were normal; however, a well-demarcated mass (1.3×2.4 cm)
with patchy dense calcification occupied the renal pelvis (Fig. 1C), with no enhancement (Fig. 1D). No evidence of metastasis was
observed on the CT scan. Consultation with the Department of
Hepatobiliary Surgery (Peking University Shenzhen Hospital)
excluded the possibility of liver metastasis and the patient's
liver dysfunction was considered to be a result of tumor
oppression. Liver supportive and anti-infective therapies were
performed, and AST and ALT levels dropped to within the normal
limits. However, the symptoms of high fever persisted (39°C), which
was interpreted as a result of the tumor hemorrhage, subsequent to
excluding the possibility of infectious disease by a specialized
infectious disease doctor.
Following an initial diagnosis of a Wilms' tumor, a
right radical nephrectomy was performed. However, complications
occurred during the surgery and the integrity of the tumor was
destroyed. The tumor was a soft-tissue mass, which involved the
upper pole of the right kidney and bulged into the perirenal fat.
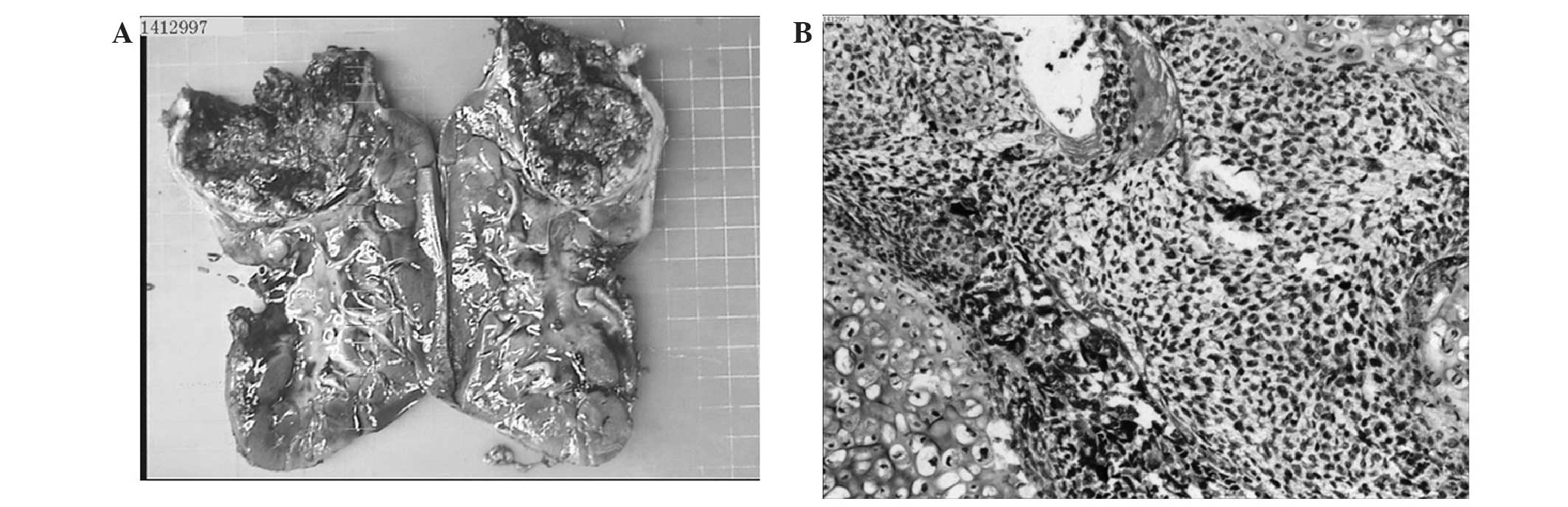
It had a grayish, dull-red appearance, was well-circumscribed and
contained areas of hemorrhage and necrosis (Fig. 2A). Histological examination indicated
a bimorphic growth pattern, which consisted of a sheath of
undifferentiated spindle-shaped cells surrounded with islands of
well-differentiated cartilage (Fig.
2B). Immunohistochemical analysis was performed and the tumor
was found to be positive for cluster of differentiation (CD) 68,
CD57, CD99 and myogenin, whereas it was negative for Wilms tumor
protein 1, smooth muscle actin, epithelial membrane antigen and
neuron-specific enolase, supporting the diagnosis of MC. The
patient recovered from surgery without any postoperative
complications. Bone scans and chest radiographs for disease staging
were negative. During the 3 months of follow-up, the left renal
tumor did not demonstrate any enlargement and no metastasis was
observed. The patient underwent 6 cycles of chemotherapy consisting
of doxorubicin (70 mg/m2, day 1) and cyclophosphamide
(700 mg/m2, day 1), each cycle lasted 28 days. The left
renal tumor did not demonstrate any enlargement and no metastasis
was observed 10 months after surgery.
Written informed consent for the present study was
obtained from the patient.
Discussion
MC is a rare, high-grade malignancy of the bone or
soft tissue, with a unique, biphasic histology and poor prognosis.
Due to its rarity and variable length of disease-free survival
rates, the disease course of MC remains poorly understood (10). MC arising in the brain and the
meninges, retroperitoneum and the extremities has previously been
reported, but MC arising in the kidney is extremely rare (10). A review of the literature was
conducted through searching the PubMed database (http://www.ncbi.nlm.nih.gov/pubmed) for English
language papers published between its inception and 28th July 2014,
using the terms ‘renal’ or ‘kidney’ and ‘mesenchymal
chondrosarcoma’; seven cases of primary renal MC were identified
(Table I) (2–8). Men and
women are equally affected by MC, most frequently in the second to
fourth decade of life (average age, 25 years). Clinical symptoms
are nonspecific and include pain, swelling, and a palpable soft
tissue mass (11). As presented in
Table I, three MC patients were male
and four were female, and the age range was 22–64 years with a mean
age of 45 years, which may be explained by the limited number of
cases (2–8). To the best of our knowledge, the patient
described in the present study is the youngest patient diagnosed
with MC. As in the present case, the majority of the MC patients
presented with flank pain and gross hematuria, incidental mass,
macroscopic hematuria by examination and high fever. The MC tumors
ranged in size between 2.5 and 12 cm with a mean size of 8 cm
(2–8).
At present, the left renal tumor in the patient of the current
study is the smallest MC observed in the kidney. The majority of
kidney MC tumors originated in the renal parenchymal (6/7
cases)(2–7), while the other case originated in the
renal pelvis (8). The current study
described the first case of MC that presented with bilateral kidney
invasion, with one tumor in the renal parenchymal region and one in
the contralateral renal pelvis.
 | Table I.Summary of reported primary renal
mesenchymal chondrosarcoma cases. |
Table I.
Summary of reported primary renal
mesenchymal chondrosarcoma cases.
| First author
(ref) | Gender | Age, years | Presentation | Imaging findings | Location | Tumor size, cm | Metastasis | Outcomes |
|---|
| Pitfield (3) | M | 61 | Severe flank
pain | Tumor
calcification | Total kidney | 12×11 | Not clear | Succumbed to the
disease 2 months later |
| Malhotra (2) | M | 27 | Gross hematuria and
flank pain | Tumor
calcification | Low pole | 9×8×7 | Femora | Recurrence after 28
months |
| Gomez-Brouchet
(4) | F | 52 | Macroscopic
hematuria | Tumor
calcification | Upper pole | 8 | No | Disease-free after 1
year |
| Kaneko (5) | F | 61 | Incidental mass | Tumor
calcification | Renal
parenchymal | 2.5×2 | No | Disease-free after 6
years |
| Buse (6) | F | 23 | Gross hematuria and
flank pain | Inhomogeneous mass
with calcification | Upper pole | 7×5 | Thyroid | Recurrence after 1
year |
| Xu (7) | M | 64 | Gross hematuria and
flank pain | Hypodense mass | Renal
parenchymal | 11×8×6 | Ureter | Succumbed to the
disease 2 months later |
| Tyagi (8) | F | 22 | Hematuria, high fever
and flank pain | Inhomogeneous and
hypodense mass | Renal pelvis | 6.5×6.2×6 | Lung | Disease-free after 6
cycles of chemotherapy |
Radiologically, MCs usually present as soft-tissue
masses with dense and granular calcification (12), as was observed in 5/7 cases documented
by imaging (2–6), in addition to the left renal mass
observed in the patient in the present case report. Renal MCs may
also present as heterogeneous and hypodense masses without
calcification (7–8), such as the right renal tumor in the
patient in the current study. To the best of our knowledge, the
present case study describes the first case with evidence of two MC
kidney tumors identified on a CT scan. The diagnosis of primary MC
is usually based on the typical histological appearance: Islands of
well-differentiated cartilage surrounded by undifferentiated
spindle mesenchymal cells (2).
Further immunohistopathological analysis is also performed when
possible. In addition, the possibility of metastasis of skeletal
chondrosarcoma should be excluded by extensive bone imaging (bone
scan, positron emission tomography-CT).
MCs are high-grade aggressive tumors. In the
literature, 4/6 cases demonstrated metastasis at presentation;
metastatic sites included the femora, thyroid, ureter and lung
(2,6–8). The
prognosis was poor, with two patients succumbing to the disease
within 2 months after diagnosis (3,7) and two
patients experiencing recurrence (2,6), which is
similar to the estimated survival rate of 55% at 5 years and 27% at
10 years for extraskeletal MC (11).
The recommended management for MC is with wide local resection and
limb salvage when possible, and the use of neoadjuvant chemotherapy
may be considered to control local disease and reduce the risk of
metastasis (13). Kaneko et al
(5) reported a patient with a tumor
size of 2.5×2 cm, who underwent local excision and remained
disease-free after 6 years, highlighting the importance of early
diagnosis and treatment to achieve an improved prognosis.
In conclusion, MC is an extremely rare neoplasm in
the kidney with poor prognosis. To the best of our knowledge, the
present study described the first case of MC that presented with
bilateral kidney invasion and calcification in the renal pelvis
with a unique appearance on a CT scan. In addition, the clinical
features were discussed, which may deepen the understanding of this
unusual neoplasm.
Acknowledgements
This study was supported by grants from the National
Natural Science Foundation of China (grant no. 81101922), the
Medical Scientific Research Foundation of Guangdong Province of
China (grant nos. A2012584 and A2013606), the Science and
Technology Development Fund Project of Shenzhen (grant no.
JCYJ20130402114702124) and the fund of Guangdong Key medical
subject.
References
|
1
|
Trembath DG, Dash R, Major NM and Dodd LG:
Cytopathology of mesenchymal chondrosarcomas: A report and
comparison of four patients. Cancer. 99:211–216. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Malhotra CM, Doolittle CH, Rodil JV and
Vezeridis MP: Mesenchymal chondrosarcoma of the kidney. Cancer.
54:2495–2499. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Pitfield J, Preston BJ and Smith PG: A
calcified renal mass: chondrosarcoma of kidney. Br J Radiol.
54:2621981. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Gomez-Brouchet A, Soulie M, Delisle MB and
Escourrou G: Mesenchymal chondrosarcoma of the kidney. J Urol.
166:23052001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kaneko T, Suzuki Y, Takata R, Takata K,
Sakuma T and Fujioka T: Extraskeletal mesenchymal chondrosarcoma of
the kidney. Int J Urol. 13:285–286. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Buse S, Behnisch W, Kulozik A, Autschbach
F and Hohenfellner M: Primary chondrosarcoma of the kidney: Case
report and review of the literature. Urol Int. 83:116–118. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Xu H, Shao M, Sun H and Li S: Primary
mesenchymal chondrosarcoma of the kidney with synchronous implant
and infiltrating urothelial carcinoma of the ureter. Diagn Pathol.
7:1252012. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Tyagi R, Kakkar N, Vasishta RK and
Aggarwal MM: Mesenchymal chondrosarcoma of kidney. Indian J Urol.
30:225–227. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gleason JM, Lorenzo AJ, Bowlin PR and
Koyle MA: Innovations in the management of Wilms’ tumor. Ther Adv
Urol. 6:165–176. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shakked RJ, Geller DS, Gorlick R and
Dorfman HD: Mesenchymal chondrosarcoma: Clinicopathologic study of
20 cases. Arch Pathol Lab Med. 136:61–75. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Murphey MD, Walker EA, Wilson AJ,
Kransdorf MJ, Temple HT and Gannon FH: From the archives of the
AFIP: Imaging of primary chondrosarcoma: radiologic-pathologic
correlation. Radiographics. 23:1245–1278. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hashimoto N, Ueda T, Joyama S, et al:
Extraskeletal mesenchymal chondrosarcoma: An imaging review of ten
new patients. Skeletal Radiol. 34:785–792. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Douis H and Saifuddin A: The imaging of
cartilaginous bone tumours. II. Chondrosarcoma. Skeletal Radiol.
42:611–626. 2013. View Article : Google Scholar : PubMed/NCBI
|