Introduction
Desmoplastic small-round-cell tumor (DSRCT) is an
uncommon and aggressive malignancy with a poor prognosis, which is
predominantly diagnosed in adolescent males (1,2). The 3-
and 5-year survival rates of patients with DSRCT were reported to
be 44% and 15%, respectively (3). It
primarily develops in the abdominal cavity. Gerald and Rosai
(1) first reported the occurrence of
DSRCT in 1989 and characterized it as a distinct type of
small-round-blue-cell tumor, which mainly occurs on serosal
surfaces, including the peritoneum and tunica vaginalis. In
addition, DSRCT was reported to primarily affect Caucasian males in
the second or third decade of life (1,2). In
general, the manifestations of intra-abdominal DSRCT are
nonspecific and may present with signs and symptoms that include
vague abdominal discomfort or a palpable abdominal mass (4). It can be distinguished from other type
of small-round-cell tumors, including neuroblastoma, Ewing's
sarcoma and Wilms' tumor, based on its clinical, immunohistological
and cytogenetic characteristics.
DSRCT treatments may comprise chemotherapy, surgical
resection and radiation therapy, however, survival rates are low.
Certain targeted therapies, such as IGF-1R inhibitors, mTOR
inhibitors and androgen blockade, have been suggested to provide a
possible clinical benefit. In addition, polychemotherapy, surgery
combined with hyperthermic intraperitoneal chemotherapy, or
radio-immunotherapy may also be promising strategies for long-term
disease control of DSRCT (5).
The present study describes the manifestations of
two cases of DSRCT that were complicated with other diseases and
involved the invasion of the pelvis or abdominal vessels. The two
cases were initially misdiagnosed, prior to immunohistological
confirmation. Written informed consent for the publication of these
case reports was obtained from the patient or the patient's
family.
Case reports
Case 1
A 25-year old man was admitted to the First
Affiliated Hospital, College of Medicine, Zhejiang University
(Hangzhou, China) in May 2008 after presenting with repeated
diarrhea and abdominal distension lasting for 9 months; in
addition, the patient had symptoms of significant weight loss and
anemia. The patient had visited the local clinic prior to admission
and trophozoites were identified in ascites and stool. Following an
anti-amebic treatment consisting of metronidazole (400 mg three
times per day, orally) for 1 month by the local clinic, the
symptoms were not alleviated. The patient underwent sonographic
examination of the abdomen, which revealed multiple heterogeneous
masses in the liver and abdomen regions, the largest measuring a
maximum diameter of 12 cm. These findings were confirmed by
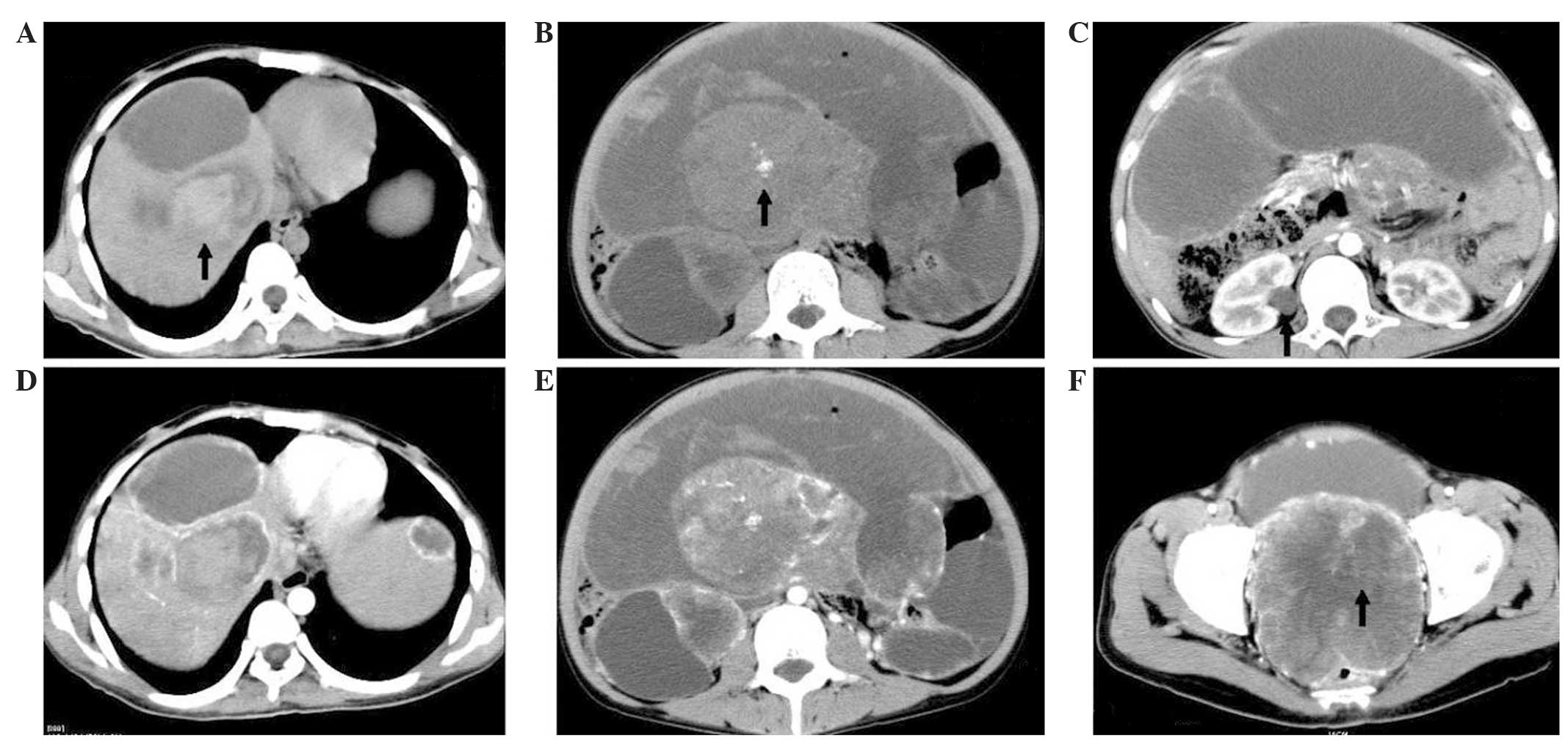
computed tomography (CT) of the abdomen and pelvis (Fig. 1). Laboratory results revealed that the
hemoglobin count, platelet count and cancer antigen (CA)125
concentration were 96 g/l (normal, 120–160 g/l),
778×109/l (normal, [100–300]×109/l)and 60.9
U/ml (normal, <25 U/ml), respectively. Based on imaging features
and laboratory data, a diagnosis of a malignant tumor with amoeba
infection was made. Subsequently, an ultrasound (US)-guided
percutaneous fine-needle biopsy of the abdominal mass was performed
in order to histopathologically analyze the mass. The results
revealed a poorly-differentiated tumor composed of clusters of
small-round-cells with insufficient cytoplasm separated by a small
amount of fiber. The round and spindle-shaped tumor cells exhibited
a vortex-like distribution and the chromatin was evenly dispersed
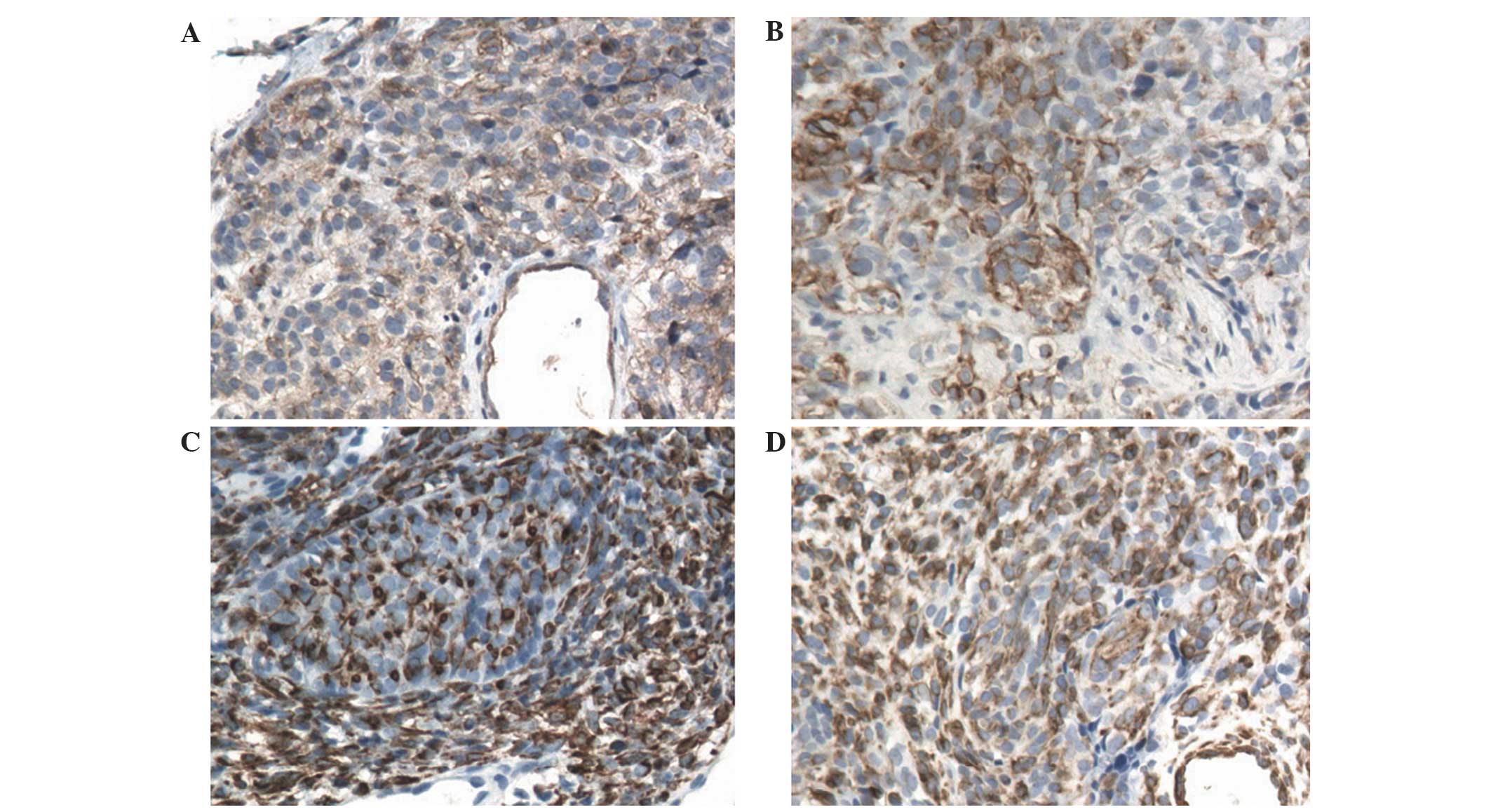
with inconspicuous nucleoli. The immunohistochemistry results were
positive for CD99, cytokeratin, vimentin and desmin (Invitrogen
Life Technologies, Paisley, UK; Fig.
2A–D, respectively). The Ewing Sarcoma/Wilms Tumor 1 (EWS/WT1)
fusion transcript, identified by reverse transcription-polymerase
chain reaction, confirmed a diagnosis of DSRCT. Chemotherapy was
advised, however, the patient refused the treatment due to the
financial cost of treatment and concerns regarding the potential
side effects, and succumbed to his illness within 1 year of
discharge from hospital.
Case 2
A 68-year-old man presented with a 20-day history of
persistent abdominal pain and was admitted to the First Affiliated
Hospital, College of Medicine, Zhejiang University, in February
2011. Physical examination revealed a stony hard mass in upper
abdomen. Routine laboratory investigations revealed
carcinoembryonic antigen and CA125 concentrations of 11.2 ng/ml
(normal, 0.0–5.0 ng/ml) and 55.1 U/ml, respectively. A US
identified solid mass lesions in the abdominal cavity.
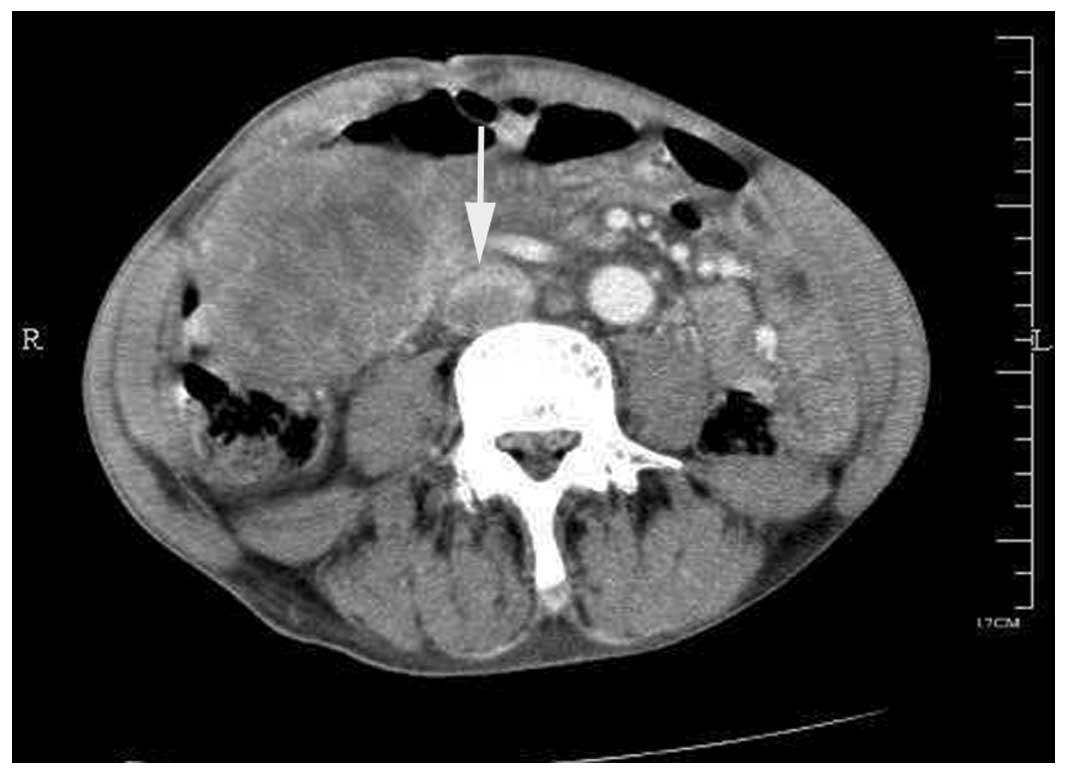
Contrast-enhanced CT of the abdomen demonstrated comparable
findings, as well as an inferior vena caval tumor thrombus
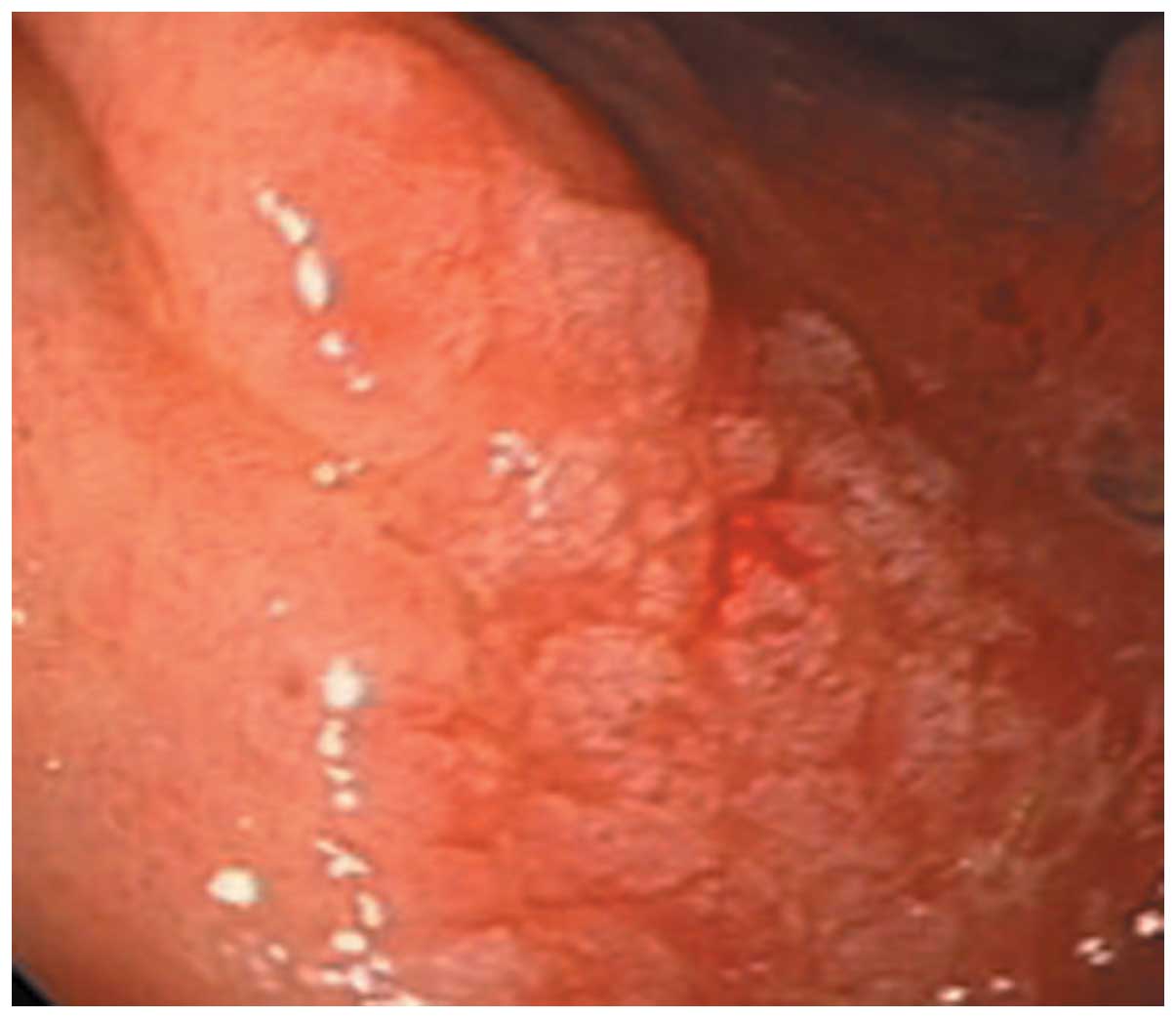
formation (Fig. 3). An endoscopy was
then performed, which revealed protruded lesions with erosion and
ulcers on the gastric body (Fig. 4);
in addition, the pathological results following endoscopic biopsy
of the stomach indicated a diagnosis of adenocarcinoma.
Subsequently, a US-guided biopsy with histological analysis of the
mass provided evidence of DSRCT. The patient refused treatment due
to concerns regarding side effects and financial costs, and
succumbed to the disease soon after discharge from hospital.
Discussion
DSRCT is an aggressive type of malignancy, which is
most commonly diagnosed in adolescents and young adults (6). At histological analysis, the tumor
manifests as islands of small-round-cells encompassed by
hypocellular, desmoplastic, collagenous stroma (2,7).
Immunohistochemical analyses of DSRCT show particular coexpression
of epithelial markers (cytokeratin), mesenchymal markers (vimentin
and desmin) and neural markers (neuron-specific enolase) (8). In addition, the t(11;22)(p13;Q12)
translocation results in the integration of the N-terminal domain
of EWS to the C-terminal DNA-binding domain of WT1 resulting in the
expression of an aberrant transcription factor that is involved in
the pathogenesis of DSRCT (9). In the
first case presented in the present study, the patient was infected
with an amoeba; therefore, clinical symptoms, including diarrhea
and weight loss, misled the diagnosis, resulting in delayed
treatment. Due to the nonspecific manifestations of DSRCT, numerous
imaging modalities are usually employed in order to evaluate
patients. The primary features characteristic of DSRCT that are
identified using CT include: Intra-abdominal soft-tissue masses
located at the omental and serosal surfaces, which do not have a
distinct organ of origin; solid, dominant, heterogeneous pelvic
masses in the retrovesical or rectouterine regions; and concurrent
metastases, which are common at the time of diagnosis, particularly
those that involve the lymph nodes and liver (10,11). DSRCT
may be associated with ascites, hepatic metastases, adenopathies,
tumor calcification and hydronephrosis due to obstructing tumor
(12). In the first case described in
the present study, imaging revealed several of these
characteristics.
In the second case discussed in the present study,
the patient was >60 years old, which is unusual compared with
the majority of cases, which occur in young men. In addition, the
imaging results of this case report revealed intra-abdominal
soft-tissue masses involving the omental and serosal surfaces,
which did not have a distinct organ of origin. If the biopsy of the
mass was omitted from the diagnostic process, it may be concluded
that the abdominal mass was homologous with gastric adenocarcinoma;
however, the biopsy revealed DSRCT, which has a different prognosis
and should be treated with a distinct chemotherapeutic
approach.
In general, the prognosis of patients with DSRCT is
poor and the ideal therapeutic modality remains to be elucidated;
therefore, early diagnosis is essential. The present two cases were
misdiagnosed as simple infection or gastrointestinal carcinoma due
to the nonspecific clinical manifestations. Biopsy confirmed the
diagnosis, however, the imaging findings were the first indication
of an aggressive malignancy. Therefore, in an adolescent or young
adult with multiple heterogeneous peritoneal soft tissue masses,
DSRCT should be considered and biopsy is recommended.
Acknowledgements
The present study was supported by grants from the
National Science and Technology Major Project (no. 2012ZX10002004)
and the Scientific Research Fund of Zhejiang Provincial Education
Department (no. N20130382).
References
|
1
|
Gerald WL and Rosai J: Case 2.
Desmoplastic small cell tumor with divergent differentiation.
Pediatr Pathol. 9:177–183. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lae ME, Roche PC, Jin L, Lloyd RV and
Nascimento AG: Desmoplastic small round cell tumor: A
clinicopathologic, immunohistochemical, and molecular study of 32
tumors. Am J Surg Pathol. 26:823–835. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Lal DR, Su WT, Wolden SL, Loh KC, Modak S
and La Quaglia MP: Results of multimodal treatment for desmoplastic
small round cell tumors. J Pediatr Surg. 40:251–255. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Leuschner I, Radig K and Harms D:
Desmoplastic small round cell tumor. Semin Diagn Pathol.
13:204–212. 1996.PubMed/NCBI
|
|
5
|
Mora J, Modak S, Cheung NK, Meyers P, de
Alava E, Kushner B, Magnan H, Tirado OM, Laquaglia M, Ladanyi M and
Rosai J: Desmoplastic small round cell tumor 20 years after its
discovery. Future Oncol. 11:1071–1081. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Biswas G, Laskar S, Banavali SD, Gujral S,
Kurkure PA, Muckaden M, Parikh PM and Nair CN: Desmoplastic small
round cell tumor: extra abdominal and abdominal presentations and
the results of treatment. Indian J Cancer. 42:78–84. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gerald WL, Miller HK, Battifora H,
Miettinen M, Silva EG and Rosai J: Intra-abdominal desmoplastic
small round-cell tumor. Am J Surg Pathol. 15:499–513. 1991.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Schröder S and Padberg BC: Desmoplsatic
small-cell tumor of the peritoneum with divergent differentiation:
Immunocytochemical and biochemical findings. Am J Clin Pathol.
99:353–355. 1993.
|
|
9
|
Biegel JA, Conard K and Brooks JJ:
Translocation (11;22) (p13;q12): Primary change in intra-abdominal
desmoplastic small round cell tumor. Genes Chromosomes Cancer.
7:119–121. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Pickhardt PJ, Fisher AJ, Balfe DM, Dehner
LP and Huettner PC: Desmoplastic small round cell tumor of the
abdomen: radiologic histopathologic correlation. Radiology.
210:633–638. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bellah R, Suzuki-Bordalo L, Brecher E,
Ginsberg JP, Maris J and Pawel BR: Desmoplastic small round cell
tumor in the abdomen and pelvis: Report of CT findings in 11
affected children and young adults. Am J Roentgenol. 184:1910–1914.
2005. View Article : Google Scholar
|
|
12
|
Chouli M, Viala J, Dromain C, Fizazi K,
Duvillard P and Vanel D: Intra-abdominal desmoplastic small round
cell tumors: CT findings and clinicopathological correlations in 13
cases. Eur J Radiol. 54:438–442. 2005. View Article : Google Scholar : PubMed/NCBI
|