Introduction
Randomized clinical studies and meta-analyses
(1–3)
have provided compelling evidence that a combination of
post-operative radiotherapy and breast-conserving surgery reduces
the local recurrence of breast cancer. Therefore, post-operative
radiation is an indispensable therapy integrated into the standard
therapeutic scheme for breast cancer patients, with the exception
of those patients aged >70 years and those with early-stage
cancer with an estrogen receptor-positive, prolactin
receptor-positive and human epidermal growth factor
receptor-2-negative genotype who could adopt endocrine therapy only
after surgery. Currently, boost irradiation for the whole breast
following breast-conserving surgery has been regarded as a classic
radiotherapy scheme (4–6). Although accelerated partial breast
irradiation has been demonstrated to be superior in terms of less
adverse reactions and a shortened treatment period compared with
conventional irradiation, and has been widely accepted in clinical
practice in recent years, it is mainly adopted for low-risk
patients with breast cancer at an early stage (7). Whole-breast irradiation remains an
irreplaceable therapy following breast-conserving surgery for
high-risk patients, however, the hypofractionated radiotherapy for
the whole breast remains under evaluation. Therefore, determination
of the target volume of the breast is considered critical for
post-operative irradiation therapy. Currently, conformal modulated
radiotherapy is the mainstream treatment for breast cancer
(4,8,9). The
post-operative intensity-modulated radiotherapy for breast cancer
is usually plotted based on the image from computed tomography (CT)
scan, and delineation of the target volume is based on the
CT-simulated location scan image; however, there is lack of clearly
defined boundaries between mammary gland and non-gland adipose
tissue in the images of the CT scan (10). It remains to be elucidated whether the
target volume of glandular breast tissue delineated by the CT scan
is sufficient for radiotherapy or not. Given the limitation in
delineating glandular breast tissue by the CT scan, the anatomical
or surface landmarks would be usually considered as a reference
tool in clinical practice. Delineation of target volume based on
the surface marks or anatomical landmarks displayed by the image
from the CT scan has been used for conventional tangential
irradiation for the whole breast, and ensures that the gland tissue
does not miss receiving radiation (11,12).
However, this method cannot be individualized for each patient, as
the position, size, shape and structure of the breast of each
patient are different, with consequent overexposure or
underexposure to the radiation. Underexposure may lead to missing
the target and the risk of recurrence, and overexposure may result
in severe acute and chronic skin reactions (12–14). In
addition, other organs, such as the lung and heart, may be
irradiated. Therefore, determination of the target volume by
palpation is comparatively accurate and individualized. Based on
the physical examination and palpation, Bentel et al
(11) placed a metal wire around the
breast, which was then used as a reference to delineate the target.
They found that the target volume differed in 65% of breasts
tested; 30% exhibited a difference in the medial boundary and 56%
in the lateral boundary. Subsequently, this method has been
continuously used by researchers to delineate the target volume of
the whole breast. However, there is a lack of a standardized
delineation method for delineating the target volume of the whole
breast. Therefore, in the current study, a comparison was performed
between the three aforementioned delineation methods in order to
find out an optimal and feasible method for clinical practice.
Materials and methods
Inclusion and exclusion criteria
The current study was approved by the Ethics
Committee of Shandong Cancer Hospital and Institute (Jinan, China),
and written informed consent was obtained from each participant. A
total of 15 patients with breast cancer who underwent
post-operative radiotherapy between May 2012 and November 2012 were
enrolled into the present study. The inclusion criteria were as
follows: An age of between 20 and 60 years old; local resection
with extended scope for breast tumor removal, and breast tumor
determined as stage T1N0M0 or T2N0M0 post-operatively with a
diameter ranging between 0.5 and 3.0 cm; and no medical history of
breast radiotherapy. The exclusion criteria were as follows: An age
of >60 years; radical mastectomy or modified radical surgery, or
quadrant resection for breast tumor removal; a breast tumor with a
diameter of >3.0 cm; and a medical history of breast trauma or
breast radiotherapy.
CT simulation location method
First, the patients were secured with a bracket. The
patients were placed in a supine position and their bilateral arms
were opened and lifted. The bracket was adjusted to ensure the most
comfortable position for patients and the affected breast was fully
exposed. The edge of the mammary gland was detected by palpation,
along which a metal wire was placed and fixed on the skin surface.
Metal tags were placed 10 mm beneath the breast folds, at the
axillary midline and the posterior axillary line of the same side,
respectively, as laser-positioning marks. A continuous spiral CT
scan with a 3-mm layer thickness was performed for each patient
under free-breathing conditions, from the cricothyroid membrane to
the bottom of the lung, with a 5-cm caudal extension. All images
were sent to the Eclipse™ treatment planning system (Varian Medical
Systems, Inc., Palo Alto, CA, USA).
Delineation of target volume
The target volume was delineated by a senior
radiation oncologist with >5 years of experience. The radiation
oncologist was familiar with the breast anatomy and breast imaging,
and was able to skillfully utilize the Eclipse delineation
tool.
Methods of delineating target
volume
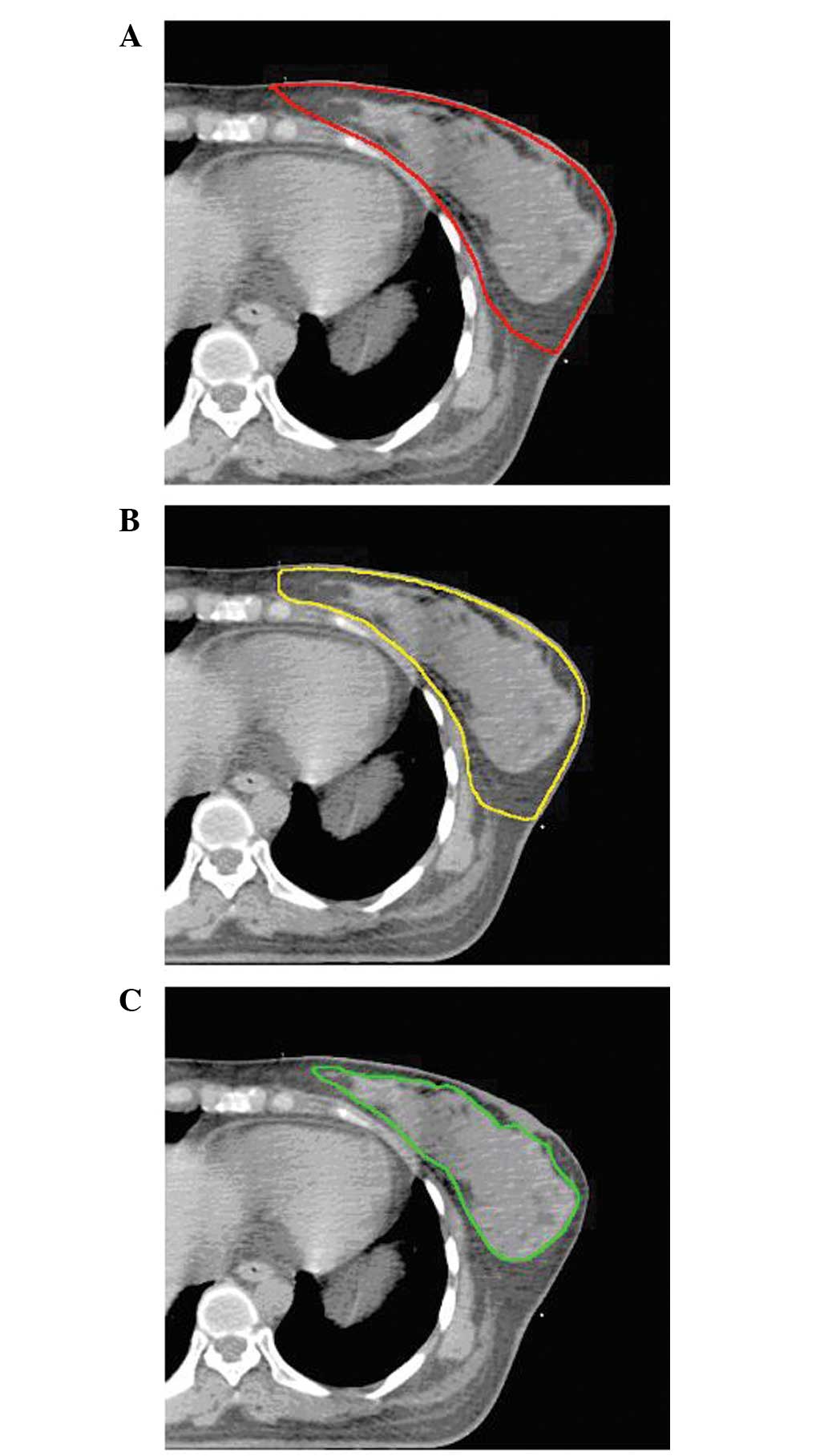
Based on the images from the CT scan, the following
three methods were used to delineate the clinical target volume
(CTV): CT scan images (CTVgl), anatomical landmarks (CTVan) and
breast palpation (CTVpa). The window width of the CT image was set
as 400 HU and window level was set as 750 HU, so that the contrast
image between the mammary gland tissue and the surrounding adipose
tissue was relatively clear. While one delineation method was used,
the other two were switched off to avoid any potential
interference.
To delineate the target volume by surface marks of
the breast (CTVan), the anterior boundary was 5 mm beneath the
skin, the posterior boundary was at the anterior edge of the
pectoralis major muscle, the cephalic boundary was at the inferior
edge of the collarbone, the caudal boundary was 10 mm beneath the
ipsilateral breast folds, the medial boundary was at the
parasternal line and the lateral boundary was at the midaxillary
line or posterior axillary line (Fig.
1A).
To delineate the target volume by palpation marks of
the breast (CTVpa), the cephalic, caudal, medial and lateral
boundaries were defined based on the metal wire placed according to
palpation. The delineation scope included the external edge of the
metal wire. The anterior boundary was 5 mm beneath the skin and the
posterior boundary was at the anterior edge of the pectoralis major
muscle (Fig. 1B).
To delineate the target volume by the CT scan images
(CTVgl), delineation was performed based on the breast gland tissue
displayed by images of the CT scan, excluding the surrounding
adipose tissues (Fig. 1C).
Calculation of target volume and
comparison of parameters
The CTV was calculated by the Eclipse treatment
planning system based on the three different delineation methods.
The degree of inclusion (DI) and conformal index (CI) were compared
among the three methods.
The DI represents the inclusion of one volume in
another volume. The formula for the DI of target A in target B is
DIA=A∩B/A, meaning the percentage of overlapping areas (between
targets A and B) in target A, while the formula for the DI of
target B in target A is DIB=A∩B/B (15). Assuming target B as the standard
target, target A was used for radiotherapy, therefore, normal
tissue of 1-DIA received unnecessary irradiation. Meanwhile, the
target tissue of 1-DIB missed the irradiation received.
The CI is defined as the ratio of overlapping areas
(between targets A and B) to the combination of targets A and B
(CI=A∩B/A∩B), representing the similarity between targets A and B.
If two target volumes are identical, CI=1, whereas if two target
volumes are not overlapping at all, CI=0 (16).
Statistical analysis
Statistical analysis was performed using SPSS 19.0
software (IBM, Armonk, NY, USA). One-way analysis of variance was
used for analyzing the differences among the three methods based on
the evaluation of the target volume. Paired t-test was used for
two-by-two comparison. P<0.05 was considered to indicate a
statistically significant difference.
Results
Patient characteristics
The general characteristics of the patients,
including patient age, tumor size and location, and treatment
administered, are listed in Table
I.
 | Table I.General characteristics of the
patients. |
Table I.
General characteristics of the
patients.
|
| Patients |
|---|
|
|
|
|---|
| Clinical
features | n | % |
|---|
| Age range, years |
|
|
|
30–40 | 6 | 40.0 |
|
40–50 | 7 | 46.7 |
|
50–60 | 2 | 13.3 |
| Breast |
|
|
| Left | 9 | 60.0 |
|
Right | 6 | 40.0 |
| Quadrant |
|
|
| Upper
outer | 8 | 53.3 |
| Lower
outer | 3 | 20.0 |
| Upper
inner | 4 | 26.7 |
| Lower
inner | 0 | 0.0 |
| Size of primary
tumor, cm |
|
|
| ≤1 | 3 | 20.0 |
| 1–2 | 7 | 46.7 |
|
>2 | 5 | 33.3 |
| Clinical stage |
|
|
|
T1N0M0 | 10 | 66.7 |
|
T2N0M0 | 5 | 33.3 |
| Axillary lymph node
removal method |
|
|
| Sentinel
lymph node biopsy | 11 | 73.3 |
| Axillary
lymphadenectomy | 4 | 26.7 |
| Post-operative
chemotherapy |
|
|
| Yes | 12 | 80.0 |
| No | 3 | 20.0 |
| Post-operative
endocrine therapy |
|
|
| Yes | 3 | 20.0 |
| No | 12 | 80.0 |
Comparison of target volume
The target volumes defined by CTVan, CTVpa and CTVgl
were 792.229±282.246, 618.331±295.903 and 196.825±117.618
cm3, respectively, with significant differences among
the methods (F=17.161; P<0.0001). Two-by-two comparison
indicated that there was no significant difference between CTVan
and CTVpa (t=3.256; P=0.08); whereas there was a significant
difference between CTVan and CTVgl (t=8.433; P<0.0001) and
between CTVpa and CTVgl (t=6.001; P<0.0001).
Comparison of CI
CI1-2 is defined as the CI between CTVan and CTVpa,
with a mean of 0.644±0.122 (range, 0.490–0.859); CI1-3 is defined
as the CI between CTVan and CTVgl, with a mean of 0.264±0.108
(range, 0.130–0.423); and CI2-3 is defined as the CI between CTVpa
and CTVgl, with a mean of 0.328±0.115 (range, 0.151–0.522). There
was a significant difference between CI1-2 and CI1-3 (t=14.708;
P<0.0001) and also between CI1-2 and CI2-3 (t=8.012;
P<0.0001).
Comparison of DI
The DI of CTVpa in CTVan was 0.890±0.08 (range,
0.774–0.990), the DI of CTVan in CTVpa was 0.709±0.144 (range,
0.492–0.892), the DI of CTVgl in CTVan was 0.994±0.005 (range,
0.985–1.000), the DI of CTVan in CTVgl was 0.264±0.109 (range,
0.130–0.423), the DI of CTVgl in CTVpa was 0.989±0.008 (range,
0.976–1.000) and the DI of CTVpa in CTVgl was 0.329±0.115 (range,
0.151–0.552).
The boundary defined by CTVan was regarded as the
standard. The distance between CTVpa and CTVan with regard to the
boundaries was measured in the medial, lateral, cephalic and caudal
directions (CTVpa boundary located outside the CTVan boundary was
depicted as a negative value; otherwise it was depicted as a
positive value), and their mean values were 3.35±7.23, 5.57±13.37,
1.75±11.62 and 11.25±4.07 mm, respectively. The boundary
differences and the correlation between target volumes and
boundaries delineated are listed in detail in Tables II and III.
 | Table II.Boundary differences of delineation
based on anatomical landmarks and palpation marks. |
Table II.
Boundary differences of delineation
based on anatomical landmarks and palpation marks.
| Boundary | Mean, mm | Maximum, mm | Minimum, mm | Coefficient of
variation |
|---|
| Medial | 3.35 | 18.0 | −9.2 | 2.16 |
| Lateral | 5.57 | 20.4 | −7.2 | 2.22 |
| Cephalic | 1.75 | 18.0 | −21.0 | 6.64 |
| Caudal | 11.25 | 21.0 | 6.0 | 0.36 |
 | Table III.Correlation between target volumes and
boundaries delineated based on anatomical landmarks and palpation
marks. |
Table III.
Correlation between target volumes and
boundaries delineated based on anatomical landmarks and palpation
marks.
|
| CTVan | CTVpa | CTVgl |
|---|
|
|
|
|
|
|---|
| Boundary | Correlation factor
(r) | P-value | Correlation factor
(r) | P-value | Correlation factor
(r) | P-value |
|---|
| Medial | −0.549 | 0.064 | −0.681 | 0.015 | −0.285 | 0.370 |
| Lateral | −0.252 | 0.430 | −0.460 | 0.132 | −0.243 | 0.446 |
| Cephalic | −0.601 | 0.051 | −0.748 | 0.005 | −0.542 | 0.069 |
| Caudal | −0.143 | 0.658 | −0.319 | 0.313 | −0.311 | 0.326 |
Discussion
Bentel et al (11) highlighted the fact that the glandular
breast tissue reflected by X-ray images cannot represent the real
volume of the breast, particularly at the superior and lateral
quadrants, and axillary tail; however, around 60% of cancer occurs
in these areas (17). In the current
study, the delineated CTVgl boundary based on the images of the CT
scan was significantly smaller than that delineated by the other
two methods; the target volume was only 24.7 and 31.7% of that
estimated by CTVan and CTVpa, respectively. One possible reason for
this may be that CTVgl included only the dense glandular breast
tissue and large breast ducts; the end of acinus and small breast
ducts may be excluded as they cannot be distinguished from the
adipose tissue by X-ray images. Therefore, there is a high risk of
missing the target volume if the analysis is based only on the
images of the CT scan. In addition, the findings of the current
study indicated that the target volume defined by CTVan and CTVpa
could contain 99% of the target volume defined by CTVgl. The
remaining 1% target volume was revealed as scattered tiny cloudy
shadows on the images of the CT scan, which exceeded the 5-mm
thickness of the subcutaneous tissue. According to anatomical
studies, the thickness of the subcutaneous adipose tissue of the
breast is only 0.5 to 2.5 mm (18–20),
therefore, the anterior boundary of target volume delineation is
usually set at a thickness of 3 to 5 mm of the subcutaneous tissue
to ensure sufficient irradiation without excessive exposure of
normal skin and subcutaneous tissue.
The results of the current study found that the
target volume defined by CTVpa was 22% smaller than that defined by
CTVan, and the CI of the two methods was 0.644 (range,
0.490–0.859). Further comparison indicated that the boundary
defined by CTVpa was within that defined by CTVan, however, there
was a large variation among patients; the most significant
difference was at the cephalic boundary with a coefficient of
variation up to 6.64, followed by the caudal and lateral boundaries
with a coefficient of variation of 0.36, consistent with the values
published in the literature. Giezen et al (21) found that the target volume based on
the images of the magnetic resonance imaging (MRI) scan was 4%
larger than that defined by the images of the CT scan; a
significant difference was found in the lateral and medial superior
directions, with a 17% alteration in the target center toward the
cephalic direction and a 3% alteration in the target center toward
the dorsal direction. By contrast, Hurkmans et al (12) found that the target volume varied
differently by each delineation, and a significant difference was
found in the posterior of the breast, and the cephalic and medial
boundaries, with a difference of 42, 28 and 24 mm, respectively;
the difference was relatively smaller at the anterior, caudal and
lateral boundaries, with values of 6, 15 and 8 mm, respectively.
The results of the current study also found that the difference in
cephalic and medial boundaries was negatively correlated with the
target volume defined by CTVpa, i.e., the larger the target volume
of CTVpa, the smaller the boundary difference. Occasionally, the
breast volume may exceed the boundary defined by CTVan; however,
the lateral or caudal boundary difference was not significantly
correlated with target volumes defined by either method. This is
due to a lack of clear boundary between the glandular breast tissue
and non-breast tissue on the images of the CT scan. The caudal and
lateral boundaries are relatively clear due to natural folds or
drooping of the breast tissue, therefore, delineation at the medial
or cephalic boundary is relatively arbitrary.
Given the limitation of the CT scan images to define
the boundary of the glandular breast tissue, the delineator and
delineation methods (or strategy) are important for defining the
CTV. For instance, Struikmans et al (10) reported that five delineators were used
in delineating CTV based on the CT scan images without using other
criteria; the CTV finally ranged between 229 and 1,214 cc, with a
significant difference. By contrast, Xu et al (22) found that there was no significant
difference among the five delineators with regard to CTV with same
delineation criteria, even when there was a clear difference prior
to the criteria being standardized among them. The majority of the
delineators have been adjusted significantly with regard to CTV
according to the delineation criteria. Therefore, the standardized
delineation criteria could significantly reduce the variation among
patients and delineators regarding CTV delineation, which is in
agreement with the results of the study by Wang et al
(23), which reported that the
variation in CTV delineated by one individual was not affected by
the CT scanning mode if standardized criteria were used. Metal
markers on the tumor bed, the tumor bed location and the age of the
patient are significant factors in CTV delineation. If the location
of the tumor bed is inclined too much on one side, subjective
judgment of the delineator will affect the consistency of
delineation (24). Adipose content of
glandular breast tissue is positively correlated with age, and as
judged by the images of the CT scan; the higher the adipose tissue
content, the higher the difficulty in delineating the target
volume. Therefore, palpation markers may be more valuable in
elderly patients.
Hurkmans et al (12) suggested that the metal wires placed
around the breast could reduce the arbitrary variation among
delineators, however, accurate delineation depends on the
pathological knowledge of the delineator on glandular breast tissue
and information provided by advanced imaging techniques. MRI has a
higher resolution on adipose tissue, and is able to reveal the
structure and surrounding soft tissue of the breast more clearly.
The major type of tissue in the cephalic direction of the breast is
the adipose tissue, which supports glandular breast tissue;
therefore, the volume delineated by the MRI scan is larger than
that delineated by the CT scan. Hence, MRI scan images will be of
use in target volume delineation, and the fusion of images from the
CT and MRI scans has already been widely used in target delineation
for brain tumors, nasopharyngeal carcinoma and prostate cancer
(25–27). Due to the profound difference in the
posture of each patient, there are significant variations between
the MRI and CT scan images of the breast; however, the fusion of
the images of the MRI and CT scans is less feasible and is
difficult for target volume delineation of the breast, therefore,
this technique remains to be improved and investigated further. By
contrast, the breast parenchyma are wrapped by the surrounding
fibrous connective tissues and adipose tissues, which function as
supportive structures, resulting in the difficulty to clearly
distinguish the glandular breast tissue even by MRI scan.
In summary, due to the limitation with regard to the
glandular breast tissue, it is not rational if the target volume
delineation is based only on the CT scan images, as this will lead
to missing target volume. CT scans in combination with MRI would
aid in defining the target volume, but requires further
investigation and improvements to the stabilization of the posture
of the patients and image fusion. Currently, a combination of
palpation marks and anatomical landmarks to define the contouring
scope of the breast is suggested to as a relatively rational method
for delineating the target volume of the breast. It is worth noting
that the knowledge and skill of the delineators is important for
accurate delineation, and the size and texture of the breast may
affect the determination of the breast boundaries by palpation,
particularly the cephalic and medial boundaries.
References
|
1
|
Liljegren G, Holmberg L, Bergh J, Lindgren
A, Tabár L, Nordgren H and Adami HO: 10-year results after sector
resection with or without postoperative radiotherapy for stage I
breast cancer: a randomized trial. J Clin Oncol. 17:2326–2333.
1999.PubMed/NCBI
|
|
2
|
Fisher B, Anderson S, Bryant J, Margolese
RG, Deutsch M, Fisher ER, et al: Twenty-year follow-up of a
randomized trial comparing total mastectomy, lumpectomy, and
lumpectomy plus irradiation for the treatment of invasive breast
cancer. N Engl J Med. 347:1233–1241. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
No authors listed. Favourable and
unfavourable effects on long-term survival of radiotherapy for
early breast cancer: an overview of the randomised trials. Early
Breast Cancer Trialists' Collaborative Group. Lancet.
355:1757–1770. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Early Breast Cancer Trialists'
Collaborative Group (EBCTCG), . Darby S, McGale P, Correa C, et al:
Effect of radiotherapy after breast-conserving surgery on 10-year
recurrence and 15-year breast cancer death: meta-analysis of
individual patient data for 10,801 women in 17 randomised trials.
Lancet. 378:1707–1716. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sedlmayer F, Sautter-Bihl ML, Budach W, et
al: Breast Cancer Expert Panel of the German Society of Radiation
Oncology (DEGRO): DEGRO practical guidelines: radiotherapy of
breast cancer I: radiotherapy following breast conserving therapy
for invasive breast cancer. Strahlenther Onkol. 189:825–833. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Hughes KS, Schnaper LA, Bellon JR, et al:
Lumpectomy plus tamoxifen with or without irradiation in women age
70 years or older with early breast cancer: long-term follow-up of
CALGB 9343. J Clin Oncol. 31:2382–2387. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Beitsch PD, Shaitelman SF and Vicini FA:
Accelerated partial breast irradiation. J Surg Oncol. 103:362–368.
2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Croog VJ, Wu AJ, McCormick B and Beal KP:
Accelerated whole breast irradiation with intensity-modulated
radiotherapy to the prone breast. Int J Radiat Oncol Biol Phys.
73:88–93. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Mouw KW and Harris JR: Irradiation in
early-stage breast cancer: conventional whole-breast, accelerated
partial-breast, and accelerated whole-breast strategies compared.
Oncology (Williston Park). 26:820–830. 2012.PubMed/NCBI
|
|
10
|
Struikmans H, Wárlám-Rodenhuis C, Stam T,
Stapper G, Tersteeg RJ, Bol GH and Raaijmakers CP: Interobserver
variability of clinical target volume delineation of glandular
breast tissue and of boost volume in tangential breast irradiation.
Radiother Oncol. 76:293–299. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bentel GC, Marks LB, Hardenbergh PH and
Prosnitz L: Variability of the location of internal mammary vessels
and glandular breast tissue in breast cancer patients undergoing
routine CT-based treatment planning. Int J Radiat Oncol Biol Phys.
44:1017–1025. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hurkmans CW, Borger JH, Pieters BR,
Russell NS, Jansen EP and Mijnheer BJ: Variability in target volume
delineation on CT scans of the breast. Int J Radiat Oncol Biol
Phys. 50:1366–1372. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kraus-Tiefenbacher U, Sfintizky A, Welzel
G, Simeonova A, Sperk E, Siebenlist K, et al: Factors of influence
on acute skin toxicity of breast cancer patients treated with
standard three-dimensional conformal radiotherapy (3D-CRT) after
breast conserving surgery (BCS). Radiat Oncol. 7:2172012.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Barnett GC, Wilkinson JS, Moody AM, Wilson
CB, Twyman N, Wishart GC, et al: The Cambridge Breast
Intensity-modulated Radiotherapy Trial: patient- and
treatment-related factors that influence late toxicity. Clin Oncol
(R Coll Radiol). 23:662–673. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hof H, Rhein B, Haering P, Kopp-Schneider
A, Debus J and Herfarth K: 4D-CT-based target volume definition in
stereotactic radiotherapy of lung tumours: comparison with a
conventional technique using individual margins. Radiother Oncol.
93:419–423. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ezhil M, Vedam S, Balter P, Choi B,
Mirkovic D, Starkschall G and Chang JY: Determination of
patient-specific internal gross tumor volumes for lung cancer using
four-dimensional computed tomography. Radiat Oncol. 4:42009.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Sohn VY, Arthurs ZM, Sebesta JA and Brown
TA: Primary tumor location impacts breast cancer survival. Am J
Surg. 195:641–644. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Na K, Xiang K and Wang G: Assessment of
thickness for breast skin and gland among office lady by
ultrasound. Zhonghua Xian Dai Ying Xiang Xue Za Zhi. 1:12–14.
2004.(In Chinese).
|
|
19
|
Wang XS and Liao KH: Yang Guoliang
Dermatology. 12th. Shanghai Scientific and Technological Literature
Publishing House; Shanghai: 2005, (In Chinese).
|
|
20
|
Li HD, Cai GB, Wang YQ, Zhang R, Li BB, Li
TY, et al: Study of normal human skin with 50 MHz ultrasound
biomicroscope. Zhong Guo Yi Xue Ying Xiang Ji Shu. 24:751–753.
2008.(In Chinese).
|
|
21
|
Giezen M, Kouwenhoven E, Scholten AN,
Coerkamp EG, Heijenbrok M, Jansen WP, et al: Magnetic resonance
imaging- versus computed tomography-based target volume delineation
of the glandular breast tissue (clinical target volume breast) in
breast-conserving therapy: an exploratory study. Int J Radiat Oncol
Biol Phys. 81:804–811. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Xu M, Li J, Yu Z, Yang T, Wang X, Zhou X,
et al: Effect of target delineation standard training for
radiotherapy on breast cancer after breast conserving surgery.
Zhonghua Fang She Zhong Liu Xu Za Zhi. 21:534–537. 2012.(In
Chinese).
|
|
23
|
Wang S, Li J, Zhang Y, Wang W, Li F, Xu M,
et al: Comparative study of 3D-CT and 4D-CT target delineation of
breast clinic volume for radiotherapy after breast conserving
surgery. Zhonghua Ru Xian Bing Za Zhi. 6:494–503. 2012.(In
Chinese).
|
|
24
|
Huang XB, Chen JY and Jiang GL: Factors
influencing clinical target volume delineation of intact breast in
intensity-modulated radiotherapy for breast cancer. Ai Zheng.
25:62–65. 2006.(In Chinese). PubMed/NCBI
|
|
25
|
Khoo VS, Dearnaley DP, Finnigan DJ,
Padhani A, Tanner SF and Leach MO: Magnetic resonance imaging
(MRI): considerations and applications in radiotherapy treatment
planning. Radiother Oncol. 42:1–15. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Emami B, Sethi A and Petruzzelli GJ:
Influence of MRI on target volume delineation and IMRT planning in
nasopharyngeal carcinoma. Int J Radiat Oncol Biol Phys. 57:481–488.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Manavis J, Sivridis L and Koukourakis MI:
Nasopharyngeal carcinoma: the impact of CT-scan and of MRI on
staging, radiotherapy treatment planning, and outcome of the
disease. Clin Imaging. 29:128–133. 2005. View Article : Google Scholar : PubMed/NCBI
|