Introduction
Subtentorial ependymoma mainly occurs in young
children and usually arises in the fourth ventricle (1). Although it is a relatively benign tumor,
cerebrospinal fluid (CSF) spread is found in 8–33% of patients
(2,3).
Moreover, subtentorial ependymoma is more inclined to exhibit CSF
metastasis compared with supratentorial ependymoma (4).
Bilateral primary posterior fossa ependymoma
originating from the cerebellopontine angle, termed primary
cerebellopontine angle ependymoma, is a rare form of subtentorial
ependymoma that predominantly occurs in infants and young children.
The main symptom is headache due to progressively increasing
intracranial pressure (5), while
cranial nerve deficit is relatively uncommon. Surgical resection
with subsequent radiotherapy is the primary treatment strategy for
patients with ependymoma (6). The
efficacy of conventional chemotherapy for this disease remains
uncertain; however, temozolomide appears to be a promising adjuvant
therapeutic approach for multifocal anaplastic ependymoma following
surgical resection (7). The extent of
surgical resection is the major determinant of overall survival in
pediatric patients (8). However, the
prognosis varies in different reports, with 5-year overall survival
ranging between 50 and 64%, and progression-free survival ranging
between 23 and 64% (5,9–11).
The present study reports a rare case of primary
cerebellopontine angle ependymoma extending to the internal
auditory canals and spinal cord in an adult man. To the best of our
knowledge, this is the first such case described in the literature,
with previously reported cases of primary cerebellopontine angle
ependymoma limited to one side with no spinal cord metastasis
(12–14). Written informed consent was obtained
from the patient.
Case report
On May 3, 2013, a 50 year-old man presented to the
Department of Neurosurgery of Shenzhen Second People's Hospital
(Shenzhen, China) due to headache, tinnitus and bilateral hearing
loss that had persisted for 4 months. A physical examination showed
no facial hypo- or hyperesthesia. Muscle strength and limb tone was
normal. The patient was positive for Romberg's sign and physical
reflections. Babinski's sign was negative. No significant past
medical history or family history were found.
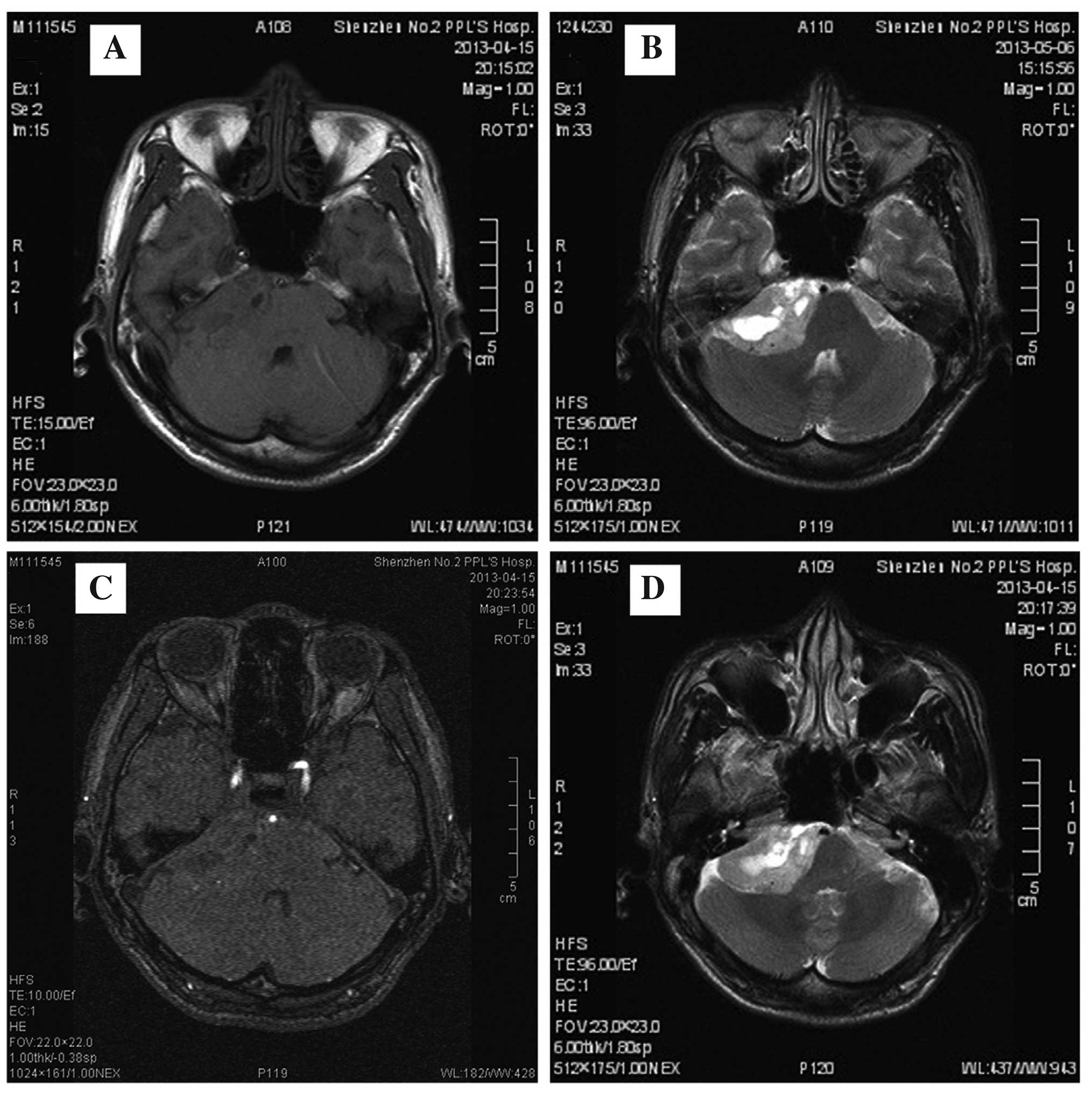
Magnetic resonance imaging (MRI) revealed a mass in
each of the cerebellopontine angles with well-defined margins and a
cyst in the middle of the right mass, which presented with abnormal
isointense to hypointense signals (compared with gray matter) on
T1-weighted images and heterogeneous hyperintense signals on
T2-weighted images. The two internal auditory canals were enlarged
due to mass extension. Contrast-enhanced MRI demonstrated a lack of
blood supply to the two masses (Fig.
1). The main differential diagnoses included acoustic neuroma,
meningioma, glioma or lower cranial nerve schwannoma, with acoustic
neuroma as the most probable preliminary diagnosis according to the
clinical symptoms, MRI appearance and enlarged internal auditory
canals.
A craniotomy was performed via a suboccipital
retrosigmoid approach, and a gross total resection was performed to
remove the tumor on the right side. During the surgery, it was
found that the tumor originated from the right cerebellopontine
angle and extended to the internal auditory canal. The tumor was
soft, fleshy and reddish-gray, with a big cyst inside. The blood
supply was poor and no apparent calcification was apparent.
Notably, the tumor was wrapped around the VII/VIII cranial nerve
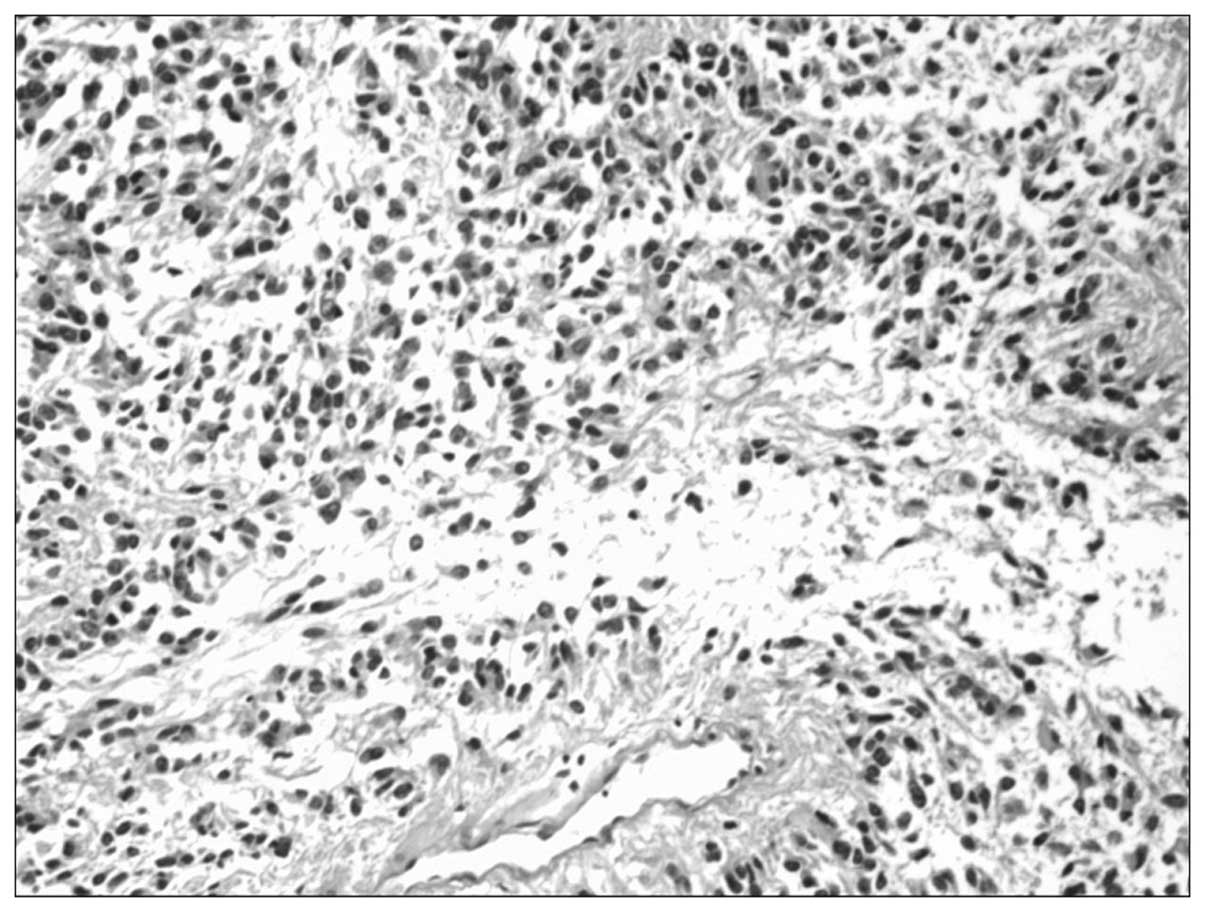
complex and all other lower cranial nerves. Histological
examination verified a papillary ependymoma, classified as a World
Health Organization grade II tumor (15). The tumor featured perivascular
pseudorosettes and small foci of bleeding, necrosis, degeneration
and pigment deposition (Fig. 2).
Moreover, the tumor was positively stained with neuron-specific
enolase, synaptophysin, cluster of differentiation (CD)99, glial
fibrillary acidic protein, S-100, chromogranin A, CD56 and Ki-67,
with a few cells with hyperchromatic nuclei.
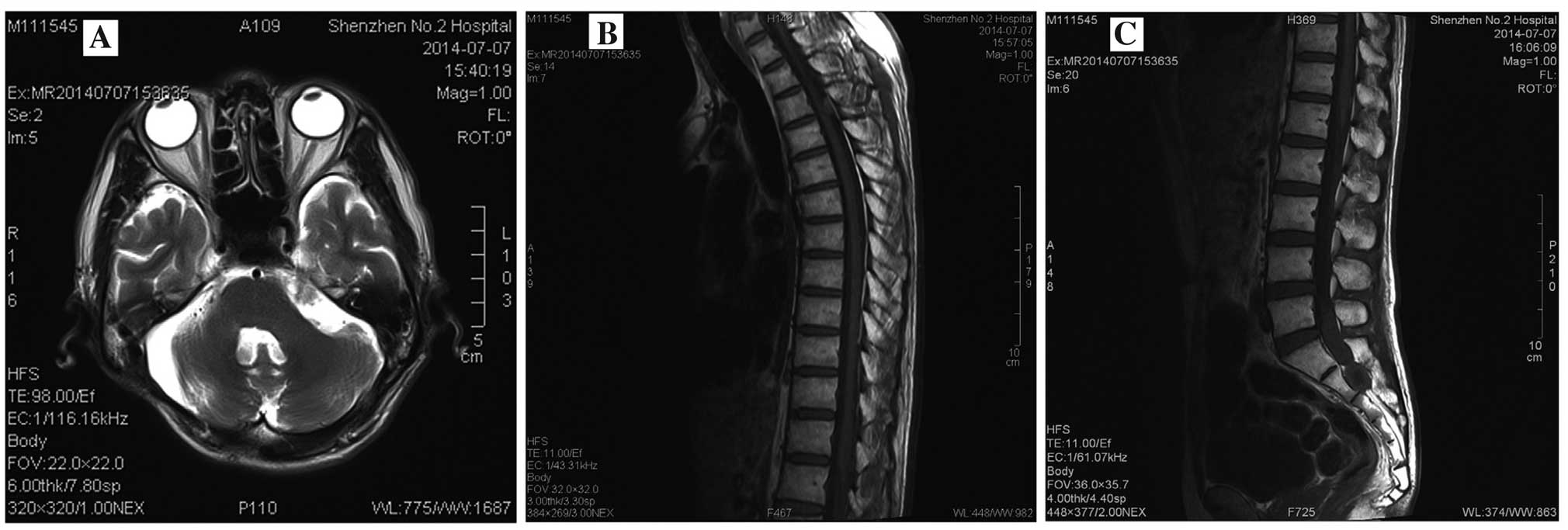
The surgery was successful and the follow up MRI
confirmed that the tumor on the right side had been completely
resected (Fig. 3A). Following the
surgery, the patient began to gradually recover in the period prior
to adjuvant chemotherapy and radiation treatment. However, during
this period, the patient started to complain of urine retention,
which had not been present prior to the surgery. This was initially
considered to be due to irritation by the urinary catheter and
prostate hypertrophy. As spinal metastasis is one of the features
of papillary ependymoma, full spinal cord MRI was performed and
massive occupational lesions were found at T3-T4 and L5-S2
(Fig. 3B and C). It was speculated
that these spinal tumors were of ependymomal origin, but a
histological examination was not performed since the patient
refused to undergo a biopsy procedure. Combination therapy using
single dose temozolomide chemotherapy (4 cycles of 150
mg/m2 administered for 5 days in a 28-day therapeutic)
and radiation therapy (3,600 cGy whole-brain and spinal cord
radiation treatment administered in 20 fractions over 28 days, and
1,620 cGy focal irradiation administered in 9 fractions over 13
days at the surgical incision site) was selected to control tumor
growth. A slight shrinkage of the T3 lesion was observed, and no
progression of the left cerebellopontine angle and S5-L2 lesions
were identified on follow-up MRI performed 13 months later
(Fig. 4).
Discussion
Ependymomas are relatively rare, with an incidence
of ~0.2 per 100,000 person-years. Men and Caucasians are more
susceptible to ependymomas compared with women and other
ethnicities (16). Particularly,
subtentorial ependymomas typically arise in the fourth ventricle
from the roof, floor, lateral medullary velum or its lateral
recesses, and the majority of the tumors appear in young children
(1). Through the foramina of Luschka
and lateral Magendie, ependymomas may extend into the
cerebellopontine angle or subarachnoid space (17). Typical MRI features of ependymomas are
hypointense to isointense on T1-weighted images and hyperintense on
T2-weighted images, with irregular enhancement and marked
heterogeneity due to hemorrhage, calcification, necrosis or cystic
components (18).
To date, radical resection is the widely accepted
therapy for ependymoma (19).
Adjuvant radiotherapy and chemotherapy have been used
post-operatively to prevent tumor recurrence. Chemotherapy has also
been used to decrease the tumor size prior to surgery and reduce
the radiotherapy dosage post-surgery. However, the potential for
adjuvant radiotherapy to improve the prognosis of a patient with
ependymoma remains under debate (19–21).
The prognosis of patients with ependymomas depends
on various factors, including tumor grade, therapeutic regimes,
extent of resection, Ki-67 index, gene type, location, age and
gender. Among them, radical removal of the tumor is the most
significant prognostic factor (22).
The prognosis of adults is significantly better than that of
children, with a 5-year-survival-rate of 55–90% compared with
14–60% (23).
For ependymoma, metastasis is relatively common for
the anaplastic type, subtentorial tumors and young patients
(24,25). In addition, surgery can potentially
cause tumor dissemination (26).
Therefore, it is important to avoid tumor dissemination and
spillage during surgery in cases of suspected ependymoma in order
to avoid CSF metastasis and recurrences. Moreover, full spinal cord
MRI is necessary for ependymomas, particularly subtentorial
ependymomas, as the tumor cells may migrate to other places through
the CSF.
In the present case, bilateral primary posterior
fossa ependymomas that originated from the cerebellopontine angles
with local invasion to the fourth ventricle and the internal
auditory canals, and with remote metastasis to the spinal cord were
reported in a 50-year-old male. This was an extremely rare case of
adult ependymoma with the following features: i) Cerebellopontine
angle origin; ii) wrapping of the VII/VIII cranial nerve complex;
and iii) extension into the internal auditory canals, with remote
metastasis to the spinal cord. These features could easily lead
doctors to form a diagnosis of neurofibromatosis type II acoustic
neuroma. The present case clearly suggests that ependymoma should
be considered as a differential diagnosis among the
cerebellopontine angle tumors. Another notable fact is that the
patient complained of a new symptom of urine retention shortly
after surgery, which was found to be caused by massive occupational
lesions in T3-T4 and L5-S2. Although a biopsy examination could not
be performed, it was highly speculated that these lesions were
metastases from the ependymoma in the brain. Apparently, these
metastasized lesions were unlikely due to surgical dissemination in
this case, as it is impossible to develop such large metastasized
lesions within a short period of two weeks (the time prior to
performing follow-up MRI).
To the best of our knowledge, this is the first
reported case of bilateral primary posterior fossa ependymomas
originating from the cerebellopontine angle and extending to the
internal auditory canals, with spinal cord metastasis. Although
primary cerebellopontine angle ependymoma is extremely rare and
difficult to diagnosis, pre-operative suspicion of ependymoma is
important for surgical planning, given its more malignant nature
and poorer prognosis compared with acoustic neuroma. The present
study also suggests that full spinal cord MRI is extremely
important to rule out spinal cord metastasis in ependymoma
patients.
Acknowledgements
This study was supported by the Shenzhen Key
Laboratory of Neurosurgery Award from the Shenzhen Science and
Technology Innovation Commission.
References
|
1
|
Cosgrove GR, Villemure JG, Robitaille Y
and Melanson D: Extraaxial ependymoma of the posterior fossa. Surg
Neurol. 24:433–436. 1985. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Qian X, Goumnerova LC, De Girolami U and
Cibas ES: Cerebrospinal fluid cytology in patients with ependymoma:
A bi-institutional retrospective study. Cancer. 114:307–314. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Salazar OM: A better understanding of CNS
seeding and a brighter outlook for postoperatively irradiated
patients with ependymomas. Int J Radiat Oncol Biol Phys.
9:1231–1234. 1983. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yuh EL, Barkovich AJ and Gupta N: Imaging
of ependymomas: MRI and CT. Childs Nerv Syst. 25:1203–1213. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Sanford RA, Merchant TE, Zwienenberg-Lee
M, Kun LE and Boop FA: Advances in surgical techniques for
resection of childhood cerebellopontine angle ependymomas are key
to survival. Childs Nerv Syst. 25:1229–1240. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Merchant TE and Fouladi M: Ependymoma: New
therapeutic approaches including radiation and chemotherapy. J
Neurooncol. 75:287–299. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Freyschlag CF, Tuettenberg J, Lohr F,
Thomé C, Schmieder K and Seiz M: Response to temozolomide in
supratentorial multifocal recurrence of malignant ependymoma.
Anticancer Res. 31:1023–1025. 2011.PubMed/NCBI
|
|
8
|
Bouffet E, Perilongo G, Canete A and
Massimino M: Intracranial ependymomas in children: A critical
review of prognostic factors and a plea for cooperation. Med
Pediatr Oncol. 30:319–329; discussion 329–331. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Pollack IF, Gerszten PC, Martinez AJ, Lo
KH, Shultz B, Albright AL, Janosky J and Deutsch M: Intracranial
ependymomas of childhood: Long-term outcome and prognostic factors.
Neurosurgery. 37:655–666; discussion 666–667. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Robertson PL, Zeltzer PM, Boyett JM, Rorke
LB, Allen JC, Geyer JR, Stanley P, Li H, Albright AL,
McGuire-Cullen P, et al: Survival and prognostic factors following
radiation therapy and chemotherapy for ependymomas in children: A
report of the Children's Cancer Group. J Neurosurg. 88:695–703.
1998. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bustamante-Montes P, Villa-Romero AR,
Lezana-Fernández MA, Fernández de Hoyos R, Borja-Aburto VH,
Lona-Zamora A and Rascón-Pacheco RA: Malnutrition as a multiple
cause of death. Salud Publica Mex. 33:475–481. 1991.(In Spanish).
PubMed/NCBI
|
|
12
|
Needle MN, Goldwein JW, Grass J, Cnaan A,
Bergman I, Molloy P, Sutton L, Zhao H, Garvin JH Jr and Phillips
PC: Adjuvant chemotherapy for the treatment of intracranial
ependymoma of childhood. Cancer. 80:341–347. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Kasliwal MK, Chandra PS and Sharma BS:
Images in neuro oncology: Primary extraaxial cerebellopontine angle
ependymoma. J Neurooncol. 83:31–32. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Lyons MK and Kelly PJ: Posterior fossa
ependymomas: Report of 30 cases and review of the literature.
Neurosurgery. 28:659–664; discussion 664–665. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Louis DN, Ohgaki H, Wiestler OD, Cavenee
WK, Burger PC, Jouvet A, Scheithauer BW and Kleihues P: The 2007
WHO classification of tumours of the central nervous system. Acta
Neuropathol. 114:97–109. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Bates JE, Peterson CR III, Yeaney GA,
Walter KA, Lundquist T, Rosenzweig D and Milano MT: Spinal drop
metastasis in myxopapillary ependymoma: A case report and a review
of treatment options. Rare Tumors. 6:54042014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Fukui MB, Hogg JP and Martinez AJ:
Extraaxial ependymoma of the posterior fossa. AJNR Am J
Neuroradiol. 18:1179–1181. 1997.PubMed/NCBI
|
|
18
|
Spoto GP, Press GA, Hesselink JR and
Solomon M: Intracranial ependymoma and subependymoma: MR
manifestations. AJNR Am J Neuroradiol. 11:83–91. 1990.PubMed/NCBI
|
|
19
|
Vitanovics D, Bálint K, Hanzély Z,
Banczerowski P and Afra D: Ependymoma in adults: Surgery,
reoperation and radiotherapy for survival. Pathol Oncol Res.
16:93–99. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Oh MC, Ivan ME, Sun MZ, Kaur G, Safaee M,
Kim JM, Sayegh ET, Aranda D and Parsa AT: Adjuvant radiotherapy
delays recurrence following subtotal resection of spinal cord
ependymomas. Neuro-oncol. 15:208–215. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Metellus P, Guyotat J, Chinot O, Durand A,
Barrie M, Giorgi R, Jouvet A and Figarella-Branger D: Adult
intracranial WHO grade II ependymomas: Long-term outcome and
prognostic factor analysis in a series of 114 patients.
Neuro-oncol. 12:976–984. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shim KW, Kim DS and Choi JU: The history
of ependymoma management. Childs Nerv Syst. 25:1167–1183. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Ambekar S, Ranjan M, Prasad C, Santosh V
and Somanna S: Fourth ventricular ependymoma with a distant
intraventricular metastasis: Report of a rare case. J Neurosci
Rural Pract. 4:(Sul 1). S121–S124. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Chao MM, Packer RJ, Myseros JS and Rood
BR: Isolated extracranial recurrence of anaplastic ependymoma.
Pediatr Blood Cancer. 56:317–318. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Liu X, Sun B, Xu Q, Che X, Hu J, Gu S and
Shou J: Outcomes in treatment for primary spinal anaplastic
ependymomas: A retrospective series of 20 patients. J Neurosurg
Spine. 19:3–11. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Yamada M, Sato T, Kuromi Y, Matsumoto Y,
Oda K, Kishida Y, Tamura T, Ichikawa M, Sakuma J and Saito K:
Surgical seeding of an anaplastic ependymoma. No Shinkei Geka.
41:1093–1097. 2013.(In Japanese). PubMed/NCBI
|