Introduction
Ectopic thymoma is a rare tumor that originates from
ectopic thymic tissue trapped during the migration of the embryonic
thymus (1). The incidence of ectopic
thymoma is ~4% (2). Various locations
of ectopic thymoma have been reported, with the cervical region
(ectopic cervical thymoma) appearing to be one of the most
frequent. Ectopic cervical thymoma commonly occurs in the
anterolateral region of the neck, or subjacent to or inside the
lower pole of the thyroid gland (1–5).
Furthermore, ectopic cervical thymoma commonly presents as a
palpable neck mass that can be easily examined by fine-needle
aspiration (FNA). However, due to its unusual locations and rare
incidence, it is easy to misinterpret the cytological features of
an ectopic cervical thymoma as a benign or malignant thyroid
lesion, such as thyroiditis, a thyroid malignancy or malignant
lymphoma of the thyroid (3–5). The present study reports a case of this
rare entity that was misdiagnosed as a lymphoproliferative lesion
by FNA.
Case report
In December 2012, a 52-year-old male presented to
Chi-Mei Medical Center (Tainan, Taiwan) with a five-year history of
a gradually enlarging anterior neck mass that had recently caused
shortness of breath. Laboratory examinations, including blood
count, biochemistry and serum thyroglobulin levels, were within
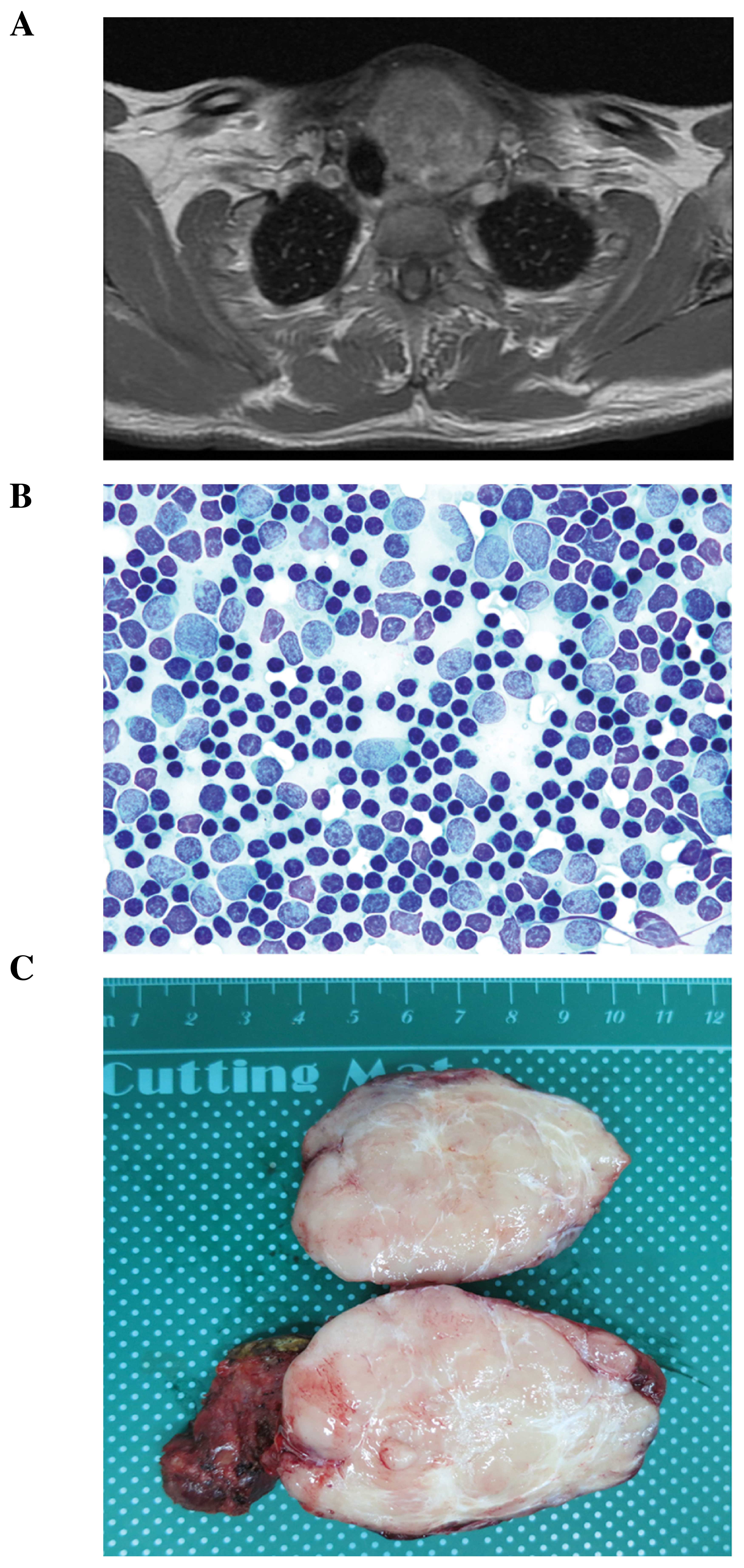
normal limits. However, neck MRI revealed a 6.4×4.8×4.4-cm mass in
the left thyroid accompanied by tracheal deviation, indicating a
nodular goiter (Fig. 1A).
Ultrasonography-guided FNA was performed, yielding
abundant small- to medium-sized lymphocytes mixed with scant larger
cells with round to oval nuclei and marginally more abundant
cytoplasm (Fig. 1B). These larger
cells were interpreted to be reactive lymphocytes or possible
follicular dendritic cells. However, no follicular cells,
specifically Hürthle cells, were identified. Therefore, the mass
was diagnosed as a lymphoproliferative lesion.
A subsequent left total thyroidectomy with mass
excision was performed as a result of the FNA smears. The tumor was
located external to the left lobe of the thyroid, but attached to
the lower end. The 6.5×4×3.5-cm excised tumor (22.5 g) was
encapsulated, with a whitish-gray and lobulated cut surface
(Fig. 1C), and was easily separated
from the grossly normal 4×3×2 cm thyroid (23.5 g). The resected
tissue was fixed in formalin and embedded in paraffin, prior to
4-µm thin sections being cut and stained with hematoxylin and
eosin.
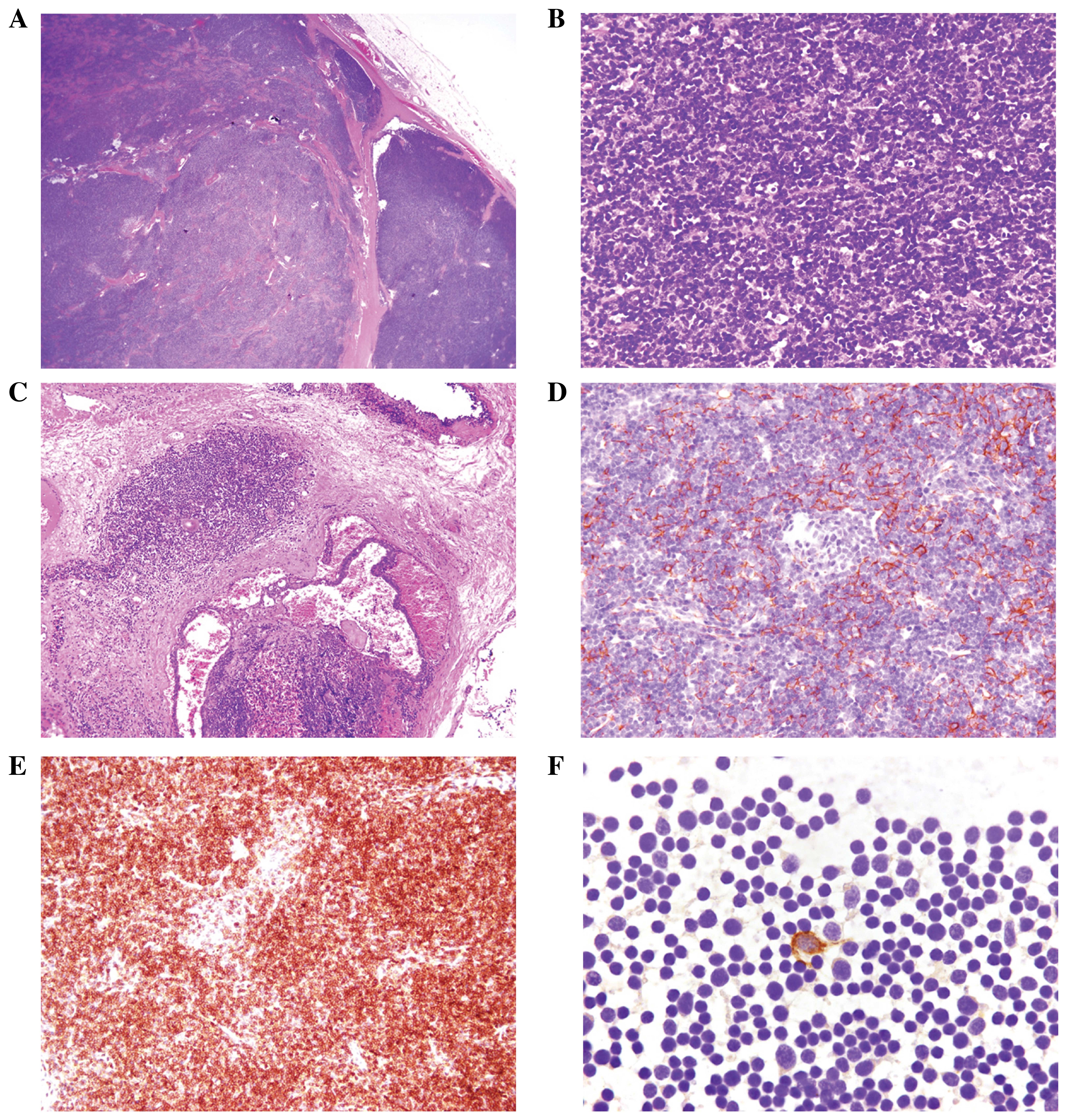
Microscopic analysis of the frozen sections revealed
that the tumor was predominantly composed of a densely packed
population of small lymphocytes in expansile sheets with preserved
lobular architecture and separated by fibrous bands (Fig. 2A). In addition, the presence of a
small number of interspersed large, polygonal cells characterized
by round, vesicular nuclei and occasionally prominent nucleoli was
focally identified (Fig. 2B).
Furthermore, microcystic changes with Hassall's corpuscles were
present in the subcapsular area (Fig.
2C). These features indicated the possibility of a lymphoid
lesion.
Immunohistochemical analysis was performed using a
labeled streptavidin-biotin peroxidase kit (Dako North America,
Inc., Carpinteria, CA, USA). The antibodies used were AE1/AE3 (Dako
North America, Inc.), cluster of differentiation (CD)1a, CD5, CD99
and terminal deoxynucleotidyl transferase (TdT; Novocastra
Laboratories Ltd., Newcastle upon Tyne, UK). The large polygonal
cells immunohistochemically expressed AE1/AE3 (Fig. 2D). By contrast, the small lymphocytes
showed immunopositivity for the immature T-cell markers, CD1a
(Fig. 2E), CD5 and TdT. Thus, the
neck tumor mimicking a thyroid mass was diagnosed as ectopic
thymoma, type B1, according to the World Health Organization (WHO)
classification (6). The adjacent
non-neoplastic thyroid exhibited no abnormal pathological findings.
Retrospective analysis of the FNA cytology revealed a rare groups
of large cells that were positive for AE1/AE3 on destained
Papanicolaou stain slides (Fig. 2F),
indicating that these cells may have represented thymic epithelial
cells. At the six-month post-operative follow-up, the patient was
healthy, with no known recurrence or distant metastasis of the
tumor.
Discussion
In contrast to mediastinal thymomas, thymomas
arising in ectopic cervical thymic tissue are rare and most often
affect female individuals, with a female:male ratio of 7:1
(1,4,5). The
majority of reported ectopic cervical thymomas are not associated
with myasthenia gravis or other paraneoplastic manifestations; only
rarely have cases been reported in association with myasthenia
gravis (7,8). The gross histological features of
ectopic cervical thymoma are identical to its mediastinal
counterparts. Furthermore, the clinical course is typically benign,
with tumor recurrence or metastasis rarely observed (9,10).
Although the microscopic features of ectopic and
mediastinal thymoma are parallels, the rarity and unusual location
of ectopic thymoma means that a straightforward diagnosis,
particularly based on FNA cytology, is difficult (10). Thymoma is composed of varying
proportions of neoplastic epithelial and reactive lymphoid
elements, and the cytological features of the tumor differ
depending on the cellular composition. When the epithelial and
lymphocytic components are obvious in the aspirate, a diagnosis of
thymoma can be easily attained. However, when a single component is
predominant, determining an accurate diagnosis is more difficult
(4).
To the best of our knowledge, only 14 cases of
ectopic cervical thymoma that include descriptions of the
cytological features based on FNA have been documented to date
(5,11). Taweevisit et al (4) compiled the details of all 14 cases in a
literature review. The initial cytological diagnoses included
Hashimoto thyroiditis, lymphocytic thyroiditis, papillary and
medullary carcinomas, malignant lymphoma of the thyroid and various
types of soft-tissue tumor (3–5,7,11–20). According to the 2004 WHO
classification system, the thymoma subtypes were predominantly type
AB and type B1, as well as two type A thymomas, one type B2 thymoma
and one type B3 thymoma (5,6).
In five of the reported cases, epithelial cells were
the predominant component; the cells had a round-polygonal or
spindle shape with eosinophilic cytoplasm. These tumors were
misdiagnosed as primary thyroid carcinoma, metastatic carcinoma and
various types of soft-tissue tumor (5,11,13,14,16. In one
case, cohesive epithelial cell clusters with rare intranuclear
inclusions were observed, resulting in the misdiagnosis as a
papillary carcinoma (16).
Identifying typical cytological features, such as papillary
architecture and nuclear changes, including powdery chromatin,
nuclear grooves and the psammoma bodies observed in papillary
thyroid carcinoma, which are absent from ectopic thymoma, may be
useful for forming a differential diagnosis. For example,
intranuclear inclusions and stromal amyloid do not occur in ectopic
thymoma, and, thus, may be useful for distinguishing it from a
spindle-cell lesion, such as a medullary carcinoma (13).
The majority of the reported cases were misdiagnosed
as thyroiditis or malignant lymphoma due to a predominantly
lymphoid population (3,4,7,12,15,19). In
such cases, the large, inconspicuous epithelial cells were
misinterpreted as follicular dendritic cells or cells of
undetermined nature (5). This was
also true in the present case. The current patient, a 52-year-old
male, presented with an enlarging mass in the anterior neck. The
mass was closely associated with the thyroid gland, and clinically,
the patient did not exhibit myasthenia gravis. The initial FNA
diagnosis was of a reactive lymphoid population, indicating the
possibility of a benign lymphoproliferative lesion. However, a
retrospective review of the patient's FNA smears revealed a
background of numerous small lymphocytes mixed with rare groups of
large, polygonal cells that may represent neoplastic thymic
epithelial cells. These large cells were positive for AE1/AE3
immunostaining, confirming their epithelial origin.
In consideration of the diagnostic course of the
present case, a careful search for large, oblong- to spindle-shaped
epithelial cells and the absence of Hürthle and/or follicular cells
may facilitate the differential diagnosis of ectopic thymoma from
thyroiditis (4). In addition, plasma
cells, tangible-body macrophages, dendritic-lymphocytic aggregates
and multinucleated foreign body giant cells are indicative of
chronic lymphocytic (Hashimoto) thyroiditis (4). Furthermore, immunohistochemical analysis
using cytokeratin and lymphoid markers, including immature T-cell
markers, may be useful for establishing the epithelial but not
lymphomatous nature of the ectopic thymoma.
In conclusion, the current study presents the
clinicopathological features of a single case of ectopic cervical
thymoma. A lack of awareness of this condition initially resulting
in an erroneous diagnosis based on FNA cytology. Therefore,
awareness of this entity, combined with a careful search for thymic
epithelial cells in the aspirate and precise interpretation of all
analyses, appear to be the key to forming an accurate
diagnosis.
Acknowledgements
The authors appreciate the support of the Biobank of
Chi Mei Medical Center (Tainan, Taiwan).
References
|
1
|
Chan JK and Rosai J: Tumors of the neck
showing thymic or related branchial pouch differentiation: a
unifying concept. Hum Pathol. 22:349–367. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Amodeo G, Cipriani O, Orsini R and
Scopelliti D: A rare case of ectopic laterocervical thymoma. J
Craniomaxillofac Surg. 41:7–9. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Yan B, Lim D and Petersson F: Ectopic
cervical thymoma: a report of two cases of a rare entity frequently
misdiagnosed on fine needle aspiration cytology and frozen section.
Head Neck Pathol. 4:152–156. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Oh YL, Ko YH and Ree HJ: Aspiration
cytology of ectopic cervical thymoma mimicking a thyroid mass. A
case report. Acta Cytol. 42:1167–1171. 1998. View Article : Google Scholar
|
|
5
|
Taweevisit M, Sampatanukul P and Thorner
PS: Ectopic thymoma can mimic benign and malignant thyroid lesions
on fine needle aspiration cytology: a case report and literature
review. Acta Cytol. 57:213–220. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Travis WD, Brambilla E, Müller-Hermelink
HK and Harris CC: World Health Organization Classification of
TumoursPathology and Genetics of Tumours of the Lung, Pleura,
Thymus and Heart. Third. IARC Press; Lyon: 2004
|
|
7
|
Choi H, Koh SH, Park MH and Kim SH:
Myasthenia gravis associated with ectopic cervical thymoma. J Clin
Neurosci. 15:1393–1395. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Wu TH, Jin JS, Huang TW, Chang H and Lee
SC: Ectopic cervical thymoma in a patient with myasthenia gravis. J
Cardiothorac Surg. 6:892011. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Kinoshita T, Yoshida J, Ishii G, Aokage K,
Hishida T and Nagai K: Pulmonary metastasis from encapsulated
cervical ectopic type a thymoma. Ann Thorac Surg. 94:e141–e142.
2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Jung JI, Kim HH, Park SH and Lee YS:
Malignant ectopic thymoma in the neck: a case report. AJNR Am J
Neuroradiol. 20:1747–1749. 1999.PubMed/NCBI
|
|
11
|
Milde P and Sidawy MK: Thymoma presenting
as a palpable thyroid nodule: a pitfall in fine needle aspiration
(FNA) of the neck. Cytopathology. 10:415–419. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Cohen JB, Troxell M, Kong CS and McDougall
IR: Ectopic intrathyroidal thymoma: A case report and review.
Thyroid. 13:305–308. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Gerhard R, Kanashiro EH, Kliemann CM,
Juliano AG and Chammas MC: Fine-needle aspiration biopsy of ectopic
cervical spindle-cell thymoma: A case report. Diagn Cytopathol.
32:358–362. 2005. View
Article : Google Scholar : PubMed/NCBI
|
|
14
|
Jin XJ, Song JY, Choi SJ, et al:
Aspiration cytology of cervical thymoma: A case report. Korean J
Pathol. 44:444–447. 2010. View Article : Google Scholar
|
|
15
|
Martin JM, Randhawa G and Temple WJ:
Cervical thymoma. Arch Pathol Lab Med. 110:354–357. 1986.PubMed/NCBI
|
|
16
|
Matsuura B, Tokunaga H, Miyake T,
Utsunomiya S, Minami H and Onji M: A case of malignant thymoma
mimicking thyroid carcinoma: A pitfall in fine-needle aspiration.
Endocr J. 51:237–241. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Ponder TB, Collins BT, Bee CS, Silverberg
AB, Grosso LE and Dunphy CH: Diagnosis of cervical thymoma by fine
needle aspiration biopsy with flow cytometry. A case report. Acta
Cytol. 46:1129–1132. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Vannucci J, Tassi V, Monacelli M and Puma
F: Totally cervical thymoma from the orthotopic thymus. Thorac
Cardiovasc Surg. 60:175–176. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Vengrove MA, Schimmel M, Atkinson BF,
Evans D and LiVolsi VA: Invasive cervical thymoma masquerading as a
solitary thyroid nodule. Report of a case studied by fine needle
aspiration. Acta Cytol. 35:431–433. 1991.PubMed/NCBI
|
|
20
|
Zeppa P, Varone V, Cozzolino I, Salvatore
D, Vetrani A and Palombini L: Fine needle cytology and flow
cytometry of ectopic cervical thymoma: A case report. Acta Cytol.
54:(Sul 5). S998–S1002. 2010.
|