Introduction
Diffuse large B cell lymphoma (DLBCL) is the most
prevalent form of non-Hodgkin's lymphoma (NHL) and has a high
incidence rate among elderly people (1,2). The
extranodal type of NHL is identified in 20–30% of patients
(3). DLBCL often presents in
extranodal sites, including the testis, skin, lung, bone and
central nervous system, as well as the respiratory and
gastrointestinal tracts (4). Primary
skeletal muscle lymphoma is exceptionally rare form of DLBCL,
particularly in the thigh and calf areas. The main symptoms of the
disease typically include presence of a mass, pain and swelling
(5). Imaging is conducted in order to
establish a diagnosis, and the most common imaging techniques used
include positron emission tomography/computed tomography (PET/CT)
and magnetic resonance imaging (MRI). The present study reports a
case of primary skeletal muscle lymphoma and provides a detailed
review of the literature associated with this disorder.
Case report
In March 2013, a 76-year-old female patient was
admitted to the Affiliated Cancer Hospital of Zhengzhou University
(Zhengzhou, China) and presented with a 1-year history of right
foot numbness, which gradually worsened. In January 2013, the
patient began experiencing pain and swelling in the right thigh and
calf. However, the patient denied suffering from typical ‘B’
symptoms, including fever, night sweats and weight loss, and had no
history of tobacco smoking, alcohol consumption or drug use.
Patient examination revealed a palpable firm mass of
54×48 mm in the right thigh and calf muscle, as well as several
10–28 mm firm, tender and mobile nodules distributed over the
patients right groin and popliteal fossa. However, there was no
evidence of hepatosplenomegaly. In addition, the patient had an
Eastern Cooperative Oncology Group performance score of 2
(http://ecog-acrin.org/resources/ecog-performance-status).
The blood test results were as follows: Hemoglobin,
10.5 g/dl (normal range, 12–16 g/dl); white cell count,
5.89×109/l; platelets, 268×109/l; lactate
dehydrogenase, 466 U/l (normal range, 109–245 U/l); and
β2-microglobulin, 3.81 mg/l (normal range, 0.8–2.2 mg/l).
Serological tests for hepatitis B and C virus as well as human
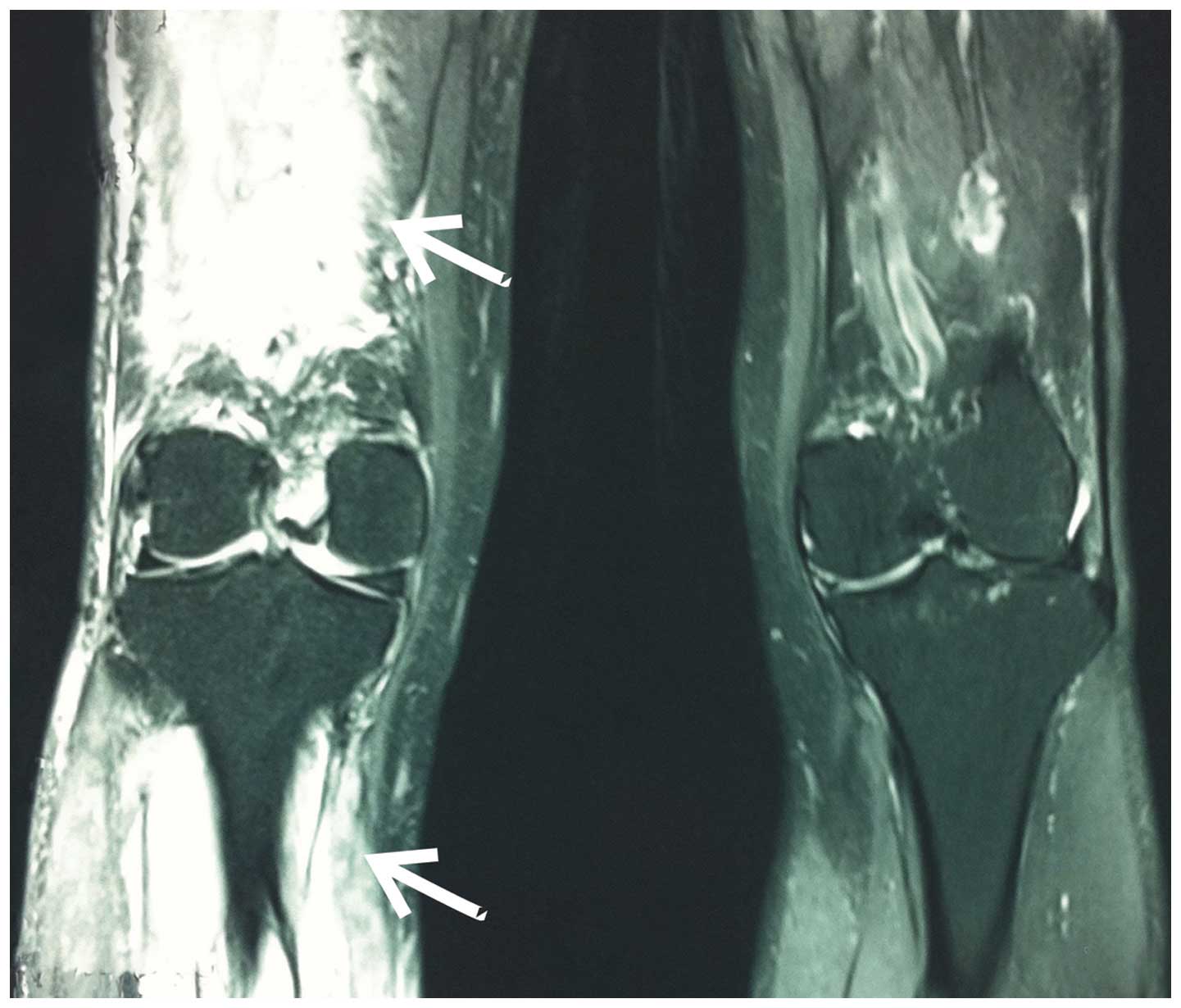
immunodeficiency virus were negative. MRI with enhanced T1-weighted
sequence revealed a hyperintense mass in the lower tibia and upper
fibula (Fig. 1), 90×54×48 mm in size.
Enlarged lymph nodes were observed in the right popliteal, right
inguinal and right iliac artery, 20–40 mm in size. CT scans
revealed enlarged lymph nodes in the mediastinum, while the
bilateral pulmonary region was normal. Bone marrow aspiration
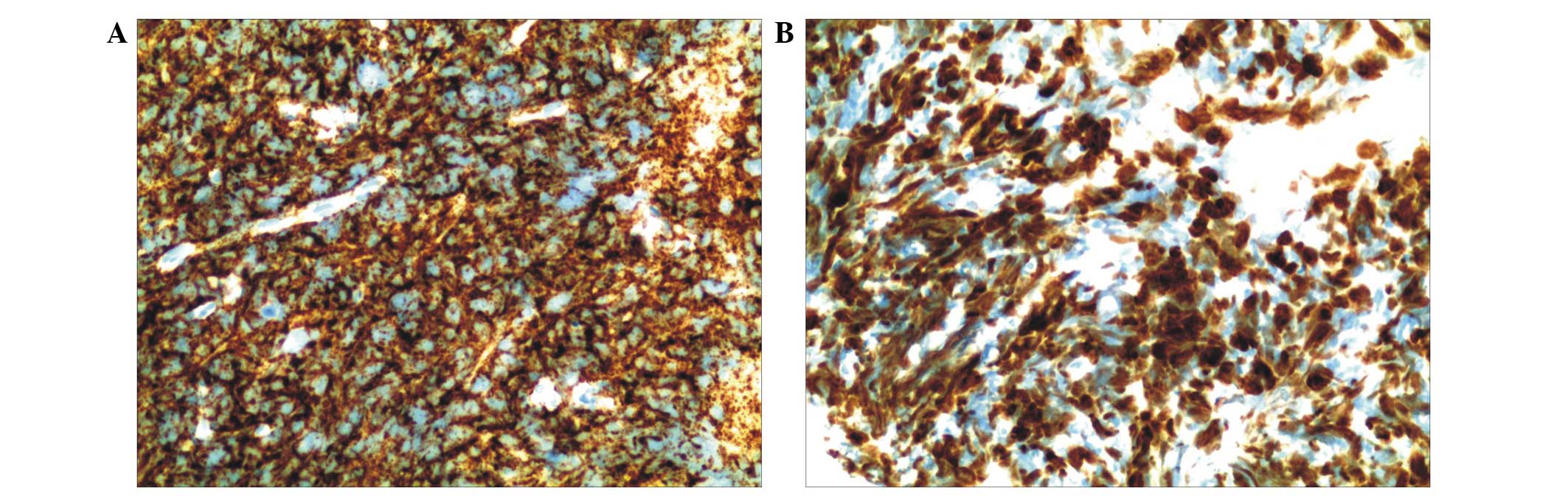
results were normal. A muscle biopsy was performed and the
histological analysis revealed a diagnosis of primary skeletal
muscle NHL DLBCL. Immunostaining of the tumoral cells demonstrated
positive staining for CD20 and CD79α, which is typical of cells
with B phenotype (Fig. 2A). Malignant
cells were strongly positive for Ki-67 (70%) (Fig. 2B). In addition, CD3, CD43, epithelial
membrane antigen, CD56 and synaptophysin were negative in the
malignant cells. The patient was diagnosed as DLBCL stage IV, with
an international prognostic index score of 4, indicating high risk
(6).
The patient received four cycles (21 days each) of
R-CHOP chemotherapy, which involved administration of the
following: 375 mg/m2 rituximab over 6 h on day −1; 750
mg/m2 cyclophosphamide, 2 mg vincristine and 50
mg/m2 doxorubicin (intravenous) on day 1; and 40
mg/m2 prednisolone (orally) on days 1–5, every 21-day
cycle. Chemotherapy was administered intravenously once a month for
a total of four cycles. The patient suffered neutropenia (absolute
neutrophil count, <0.5×109/l) and infectious
complication during the first cycle. The patient was then treated
with a modified R-Mini-CHOP (day 1, 600 mg/m2
cyclophosphamide, 2 mg/m2 vindesine and 375
mg/m2 rituximab; day 2, 50 mg/m2 epirubicin;
and days 1–5, 40 mg/m2 prednisone) for the remaining
three cycles. There was evident relief of pain and swelling in the
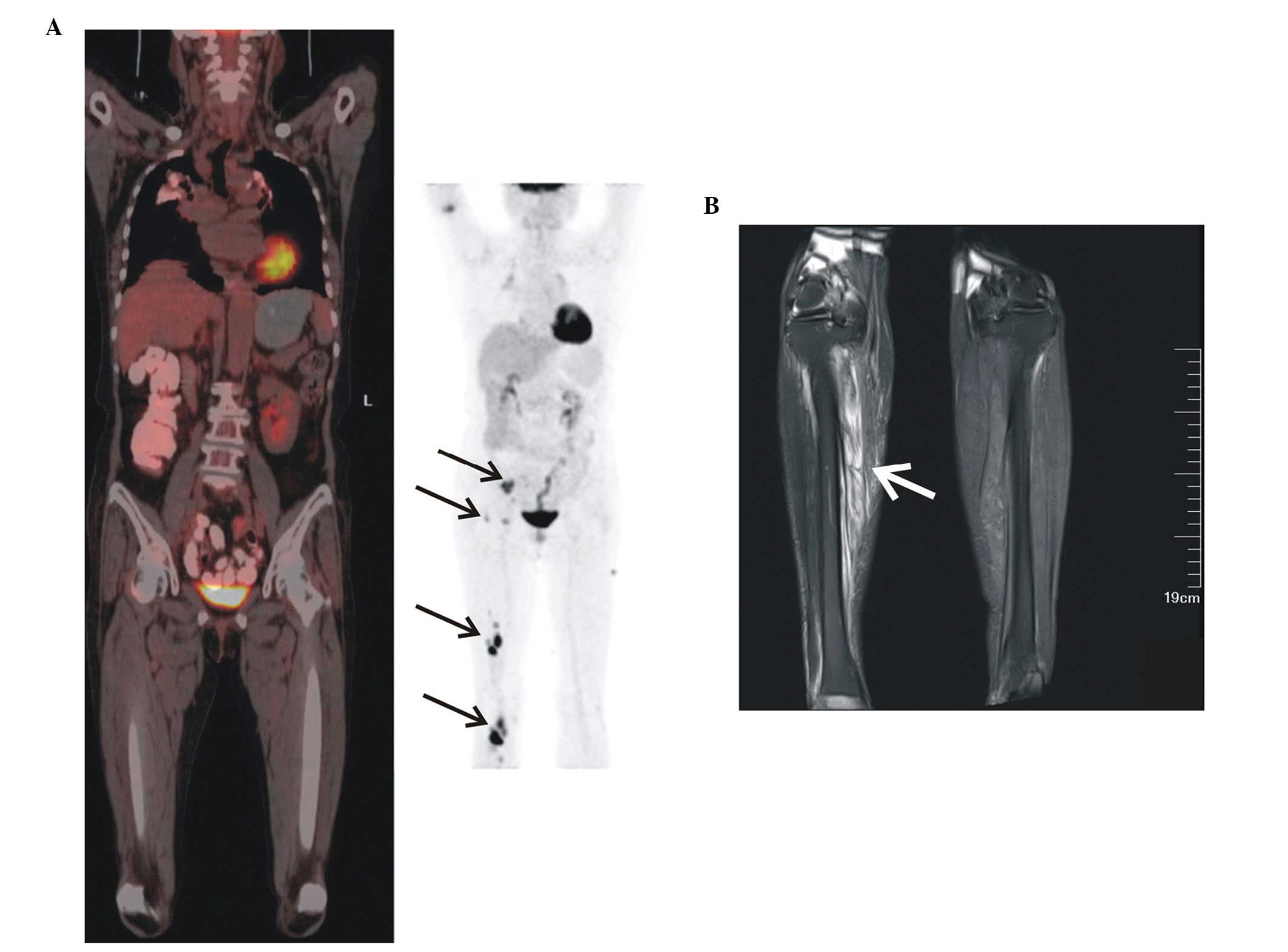
right extremity. PET/CT imaging with 18F-fluorodeoxyglucose
revealed a reduced fluorodeoxyglucose (FDG) uptake in the tumor and
lymph nodes. However, in addition to the right thigh and calf
muscle, FDG uptake persisted in the right iliac artery lymph nodes
and right inguinal lymph nodes (Fig.
3A). PET/CT was used to evaluate the efficacy of the treatment,
which revealed a stabilization of the disease. The patient was
further treated with chemotherapy as follows: Day 1, 375
mg/m2 rituximab; day 3/7, 1000 mg/m2
gemcitabine; day 3–7, 15 mg/m2 cisplatin; and day 3–7, 9
mg dexamethasone (R-GDP) every 30 days for a total of 2 cycles. In
October 2013 (2 months after chemotherapy), the patient suffered a
gradual aggravation of edema, swelling and pain in the right lower
limb. Doppler ultrasound results revealed an enlarged hypoechoic
mass in the right calf, 72×43 mm in size. Subsequently, an adjusted
chemotherapy regimen of bleomycin, cytarabine, vincristine,
cyclosphamide and dexamethasone (BCOAD) regimen was administrated
for 2 cycles. Subsequently, the patient received two cycles of
R-BCOAD chemotherapy, which involved administration of the
following: 375 mg/m2 rituximab over 6 h on day −1; 2.5
mg/m2 bleomycin, 0.5 mg vincristine and 10
mg/m2 cytarabine continuous infusion over 24 h on days
1–4; 650 mg/m2 cyclophosphamide on day 5; and 10
mg/m2 prednisolone (orally) on days 1–5, every 21-day
cycle. This chemotherapy was administered through a continuous
intravenous infusion of bleomycin, cytarabine and vincristine over
96 h. The edema was completely alleviated and the mass in the right
lower limb began to shrink. MRI results revealed a reduction in
tumor size in the lower limb and the mass in the right thigh became
undetectable (Fig. 3B). The patient
received a local radiation therapy; however, the effect of the
treatment was poor and the mass gradually increased. The patient
succumbed to the disease on July 2, 2014. Written informed consent
was obtained from the patient's family prior to the publication of
the present study.
Discussion
Primary skeletal muscle lymphoma was first reported
by Kandel et al (7) in 1984
and has since been reported to account for ~0.5% of extranodal
lymphomas (8), with an incidence rate
of <0.1% in all lymphoma of the extremities (9). Therefore, primary skeletal muscle NHL of
diffuse large B cell immunophenotype is exceptionally rare. This
disease may occur through one of the three ways: As disseminated
disease via the hematogenous or lymphatic pathways; as an extension
from adjacent organs, such as bones or lymph nodes; or very rarely,
as primary extranodal disease (10).
The common clinical symptoms of primary skeletal
muscle lymphoma are usually associated with muscle swelling, limb
pain and edema, without any sign of heat and redness (5); in addition, this disease may occur as
isolated lesions (11). The clinical
features of the extranodal lymphoma include pain and tenderness,
lymphadenopathy, ipsilateral extremity swelling and elevated
lactate dehydrogenase, which therefore aid the diagnosis the
primary skeletal muscle lymphoma (12). Furthermore, primary skeletal muscle
lymphoma exhibits certain distinctive MRI features, which allow it
to be differentiated from other types of soft-tissue tumors: On
T1-weighted images, an increased signal intensity is commonly
observed compared with normal muscle; and on T2-weighted images,
intermediate signal intensity is observed compared with fat
(11,13). In addition, on contrast-enhanced MRI,
skeletal muscle lymphoma demonstrates homogeneous diffuse
enhancement (14). CT scans may
reveal muscle swelling and also serve as a tool to guide biopsy.
With the development of technology, the clinical application of
PET/CT has become increasingly important for lymphoma diagnosis and
tumor staging (15). In the present
study, PET/CT was employed in order to assess the efficacy of the
chemotherapy treatments. However, imaging features of lymphoma in
skeletal muscle are nonspecific and it may be difficult to
distinguish lymphoma from other diseases, such as primary soft
tissue, sarcoma, metastases, trauma or myositis (11). Therefore, biopsy and pathological
evaluation are essential for the diagnosis of primary skeletal
lymphoma (16). The present case
report illustrated that MRI and CT provided the basis for diagnosis
and that the diagnosis was confirmed through biopsy histopathology
and immunohistochemistry.
The treatment of primary skeletal muscle lymphoma
relies predominantly on the type of lymphoma. The prognosis of
primary skeletal muscle lymphoma is poor compared with that of
lymph node lymphoma, especially at stages III–IV. Therefore,
selecting the most effective treatment regimen is essential. The
present study reported a case of DLBCL, the standard treatment for
which is R-CHOP (17–21).
The combination of chemotherapy and radiotherapy
significantly was reported to increase disease-free survival and
overall survival (OS) rates (22). In
addition, chemotherapy followed by local radiotherapy, compared
with chemotherapy alone, demonstrated improved event-free survival
(EFS) results (23). A previous study
reported 5-year survival, EFS and OS rates of 94, 84 and 91%,
respectively (24). However, ~50% of
DLBCL patients are unresponsive to the standard chemotherapy or
suffer disease relapse (19,20). Patients with refractory NHL have
limited treatment options and poor prognosis. Hou et al
(25) reported that GDP with or
without rituximab was effective in patients with refractory or
relapsed aggressive B cell NHL. The overall response rate of
patients with recurrent history or patients with refractory
aggressive histology B cell NHL is 49–72% (25–27). In
addition, 28% of patients suffered grade III–IV neutropenia and 40%
of patients suffered thrombocytopenia (25–27). Aribi
et al (26) reported that the
3-year progression-free and EFS rates were 20.5% (range, 16.3–24%)
and 19.7% (range, 15.9–23.5%) for the GPD regimen, respectively.
These results indicated that GDP with or without rituximab may be a
promising treatment option for refractory DLBCL. However, in the
present study, the patient received a modified BCOAD regimen, which
had not been previously reported; the results demonstrated that the
treatment was effective in this patient and to date the patient has
remained stable and healthy.
In conclusion, primary skeletal muscular DLBCL is a
rare lesion that frequently occurs among elderly adults. Imaging
can be used to reveal the location and the size of the mass. Biopsy
or surgery are the key to the diagnosis of DLBCL. Selection of the
appropriate treatment regimen is challenging and requires further
investigation.
References
|
1
|
Yancik R and Ries LA: Cancer in older
persons: An international issue in an aging world. Semin Oncol.
31:128–136. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Flowers CR, Sinha R and Vose JM: Improving
outcomes for patients with diffuse large B-cell lymphoma. CA Cancer
J Clin. 60:393–408. 2010.PubMed/NCBI
|
|
3
|
Freeman C, Berg JW and Cutler SJ:
Occurrence and prognosis of extranodal lymphomas. Cancer.
29:252–260. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Bourdeanu L, Menon R and Somlo G: Diffuse
large B-cell lymphoma with calf muscle localization. Case Rep
Hematol. 2011:2924942011.PubMed/NCBI
|
|
5
|
Lee VS, Martinez S and Coleman RE: Primary
muscle lymphoma: Clinical and imaging findings. Radiology.
203:237–244. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Talaulikar D, Shadbolt B, Dahlstrom JE and
McDonald A: Routine use of ancillary investigations in staging
diffuse large B-cell lymphoma improves the International Prognostic
Index (IPI). J Hematol Oncol. 2:492009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kandel RA, Bédard YC, Pritzker KP and Luk
SC: Lymphoma. Presenting as an intramuscular small cell malignant
tumor. Cancer. 53:1586–1589. 1984. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Glass AG, Karnell LH and Menck HR: The
National Cancer Data Base report on non-Hodgkin's lymphoma. Cancer.
80:2311–2320. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Travis WD, Banks PM and Reiman HM: Primary
extranodal soft tissue lymphoma of the extremities. Am J Surg
Pathol. 11:359–366. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Suresh S, Saifuddin A and O'Donnell P:
Lymphoma presenting as a musculoskeletal soft tissue mass: MRI
findings in 24 cases. Eur Radiol. 18:2628–2634. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Hwang S: Imaging of lymphoma of the
musculoskeletal system. Radiol Clin North Am. 46:379–396. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Damron TA, Le MH, Rooney MT, Vermont A and
Poiesz BJ: Lymphoma presenting as a soft tissue mass. A soft tissue
sarcoma simulator. Clin Orthop Relat Res:221–230. 1999.
|
|
13
|
Chun CW, Jee WH, Park HJ, Kim YJ, Park JM,
Lee SH and Park SH: MRI features of skeletal muscle lymphoma. AJR
Am J Roentgenol. 195:1355–1360. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Hwang S: Imaging of lymphoma of the
musculoskeletal system. Magn Reson Imaging Clin N Am. 18:75–93.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Kang HJ, Beylergil V, Price AP, Abramson
SJ and Carrasquillo JA: FDG PET/CT detection of intussusception
caused by lymphoma in a pediatric patient. Clin Nucl Med. 39:97–98.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Knowles B and Serpell JW: Extra-nodal
lymphoma presenting as a mimic of soft-tissue sarcoma. ANZ J Surg.
73:26–30. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Coiffier B, Lepage E, Briere J, Herbrecht
R, Tilly H, Bouabdallah R, Morel P, Van Den Neste E, Salles G,
Gaulard P, et al: CHOP chemotherapy plus rituximab compared with
CHOP alone in elderly patients with diffuse large-B-cell lymphoma.
N Engl J Med. 346:235–242. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Feugier P, Van Hoof A, Sebban C,
Solal-Celigny P, Bouabdallah R, Fermé C, Christian B, Lepage E,
Tilly H, Morschhauser F, et al: Long-term results of the R-CHOP
study in the treatment of elderly patients with diffuse large
B-cell lymphoma: A study by the Groupe d'Etude des Lymphomes de
l'Adulte. J Clin Oncol. 23:4117–4126. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Habermann TM, Weller EA, Morrison VA,
Gascoyne RD, Cassileth PA, Cohn JB, Dakhil SR, Woda B, Fisher RI,
Peterson BA, et al: Rituximab-CHOP versus CHOP alone or with
maintenance rituximab in older patients with diffuse large B-cell
lymphoma. J Clin Oncol. 24:3121–3127. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Coiffier B, Thieblemont C, Van Den Neste
E, Lepeu G, Plantier I, Castaigne S, Lefort S, Marit G, Macro M,
Sebban C, et al: Long-term outcome of patients in the LNH-98.5
trial, the first randomized study comparing rituximab-CHOP to
standard CHOP chemotherapy in DLBCL patients: A study by the Groupe
d'Etudes des Lymphomes de l'Adulte. Blood. 116:2040–2045. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Niitsu N: Current treatment strategy of
diffuse large B-cell lymphomas. Int J Hematol. 92:231–237. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Spina M, Balzarotti M, Uziel L, Ferreri
AJ, Fratino L, Magagnoli M, Talamini R, Giacalone A, Ravaioli E,
Chimienti E, et al: Modulated chemotherapy according to modified
comprehensive geriatric assessment in 100 consecutive elderly
patients with diffuse large B-cell lymphoma. Oncologist.
17:838–846. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Huang Z, Xu Z and Zhou Y: Chemotherapy
alone versus chemotherapy followed by consolidative radiotherapy
for limited-stage aggressive non-Hodgkin's lymphoma: A
meta-analysis of randomized controlled trials. Cancer Radiother.
17:736–743. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Dorth JA, Prosnitz LR, Broadwater G,
Beaven AW and Kelsey CR: Radiotherapy dose-response analysis for
diffuse large B-cell lymphoma with a complete response to
chemotherapy. Radiat Oncol. 7:1002012. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Hou Y, Wang HQ and Ba Y: Rituximab,
gemcitabine, cisplatin, and dexamethasone in patients with
refractory or relapsed aggressive B-cell lymphoma. Med Oncol.
29:2409–2416. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Aribi M, Mesli N, Remla N, Sari BE, Taleb
A, Touhami H, Bekadja MA, ZouaouiBenhadji Z, Bouzid K and Meguenni
K: Gemcitabine and treatment of diffuse large B-cell lymphoma in
relapsed or refractory elderly patients: A prospective randomized
trial in Algeria. J Cancer Res Ther. 6:41–46. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Crump M, Baetz T, Couban S, Belch A,
Marcellus D, HowsonJan K, Imrie K, Myers R, Adams G, Ding K, et al:
Gemcitabine, dexamethasone, and cisplatin in patients with
recurrent or refractory aggressive histology B-cell non-Hodgkin
lymphoma: A Phase II study by the national cancer institute of
Canada clinical trials group (NCIC-CTG). Cancer. 101:1835–1842.
2004. View Article : Google Scholar : PubMed/NCBI
|