Introduction
A number of previous studies have indicated that
certain immune cells are essential for the progression of tumors
and may serve as good indicators of prognosis (1–5). Patients
with lymphocyte infiltration around the tumor, for example, may
have a good prognosis due to efficient natural killer cells, or
because the lymphocytes are involved in lymphokine-activated tumor
cell killing (6–8). However, several lines of evidence
indicate that a high density of neutrophils may actually promote
tumor growth and metastasis (9,10) and/or
suppress lymphocyte activity, leading to counteraction of the
antitumor immune response (11). In
previous clinical studies, tumor-bearing patients who had
granulocytosis were treated by selective granulocytapheresis (a
procedure which produces controlled depletion of granulocytes),
which resulted in prolonged survival rates (12,13). The
neutrophil/lymphocyte (N/L) ratio, represents the relative number
of each of these two major leukocyte populations and indicates
fluctuations in their numbers and their likely impact on the
progression or prognosis of cancer. A number of studies on
gastrointestinal cancer have supported this theory. We have
previously reported that the N/L ratio was significantly associated
with increased tumor stage and overall survival of patients with
gastric and rectal cancer (14,15). One
theory is that the high N/L ratio reflects the poor status of the
immune system against cancer and/or the progression of cancer, but
no previous studies have demonstrated that the N/L ratio may serve
as an independent indicator of chemotherapy effect for patients
with unresectable or recurrent gastric cancer. Considerable efforts
have been made to identify the parameters that predict the
effectiveness of chemotherapy, including computerised tomography
(CT) scan and the identification of tumor markers. By contrast, the
N/L ratio, which is measured relatively easily, may be a valuable
index (indicator of chemotherapy efficacy) in the clinical setting
for determining patients that may benefit from chemotherapy. Based
on these concepts, the present study evaluated whether the baseline
N/L ratio is a predictor of the effectiveness of chemotherapy in
the treatment of unresectable or recurrent gastric cancer.
Patients and methods
A total of 135 patients were selected with
unresectable or recurrent gastric cancer who had not previously
received adjuvant chemotherapy 1 month prior to randomization (79
males and 56 females; average age, 61.05±12.05 years; range, 33–82
years), who were diagnosed using gastroscope biopsy. A total of 56
cases were classified by surgery (aborted the surgery prior to
laparotomy or underwent bypass surgery), 70 cases were classified
by CT or magnetic resonance imaging, 9 cases were classified by
alternative methods. All the patients received chemotherapy for a
2–6 month course, and patients who objected to bone marrow
suppression and/or inflammation were excluded. The N/L ratio was
calculated prior to chemotherapy (pre-chemo-N/L ratio) and 2–4
weeks from after the chemotherapy was finished
(post-chemo-chemo-N/L ratio). The overall survival was calculated
from the date of diagnosis until the date of mortality or the last
follow-up time period.
All the data, including gender, age, stage of
disease and pathological factors were obtained from the clinical
and pathological records and included in the univariate analyses.
Significant differences were determined by a non-parametric test.
Univariate influence of a given parameter on survival was assessed
with log-rank test. P<0.05 was considered to indicate a
statistically significant difference. All statistical analyses were
performed using SPSS software, version 16 (SPSS, Inc., Chicago, IL,
USA).
Results
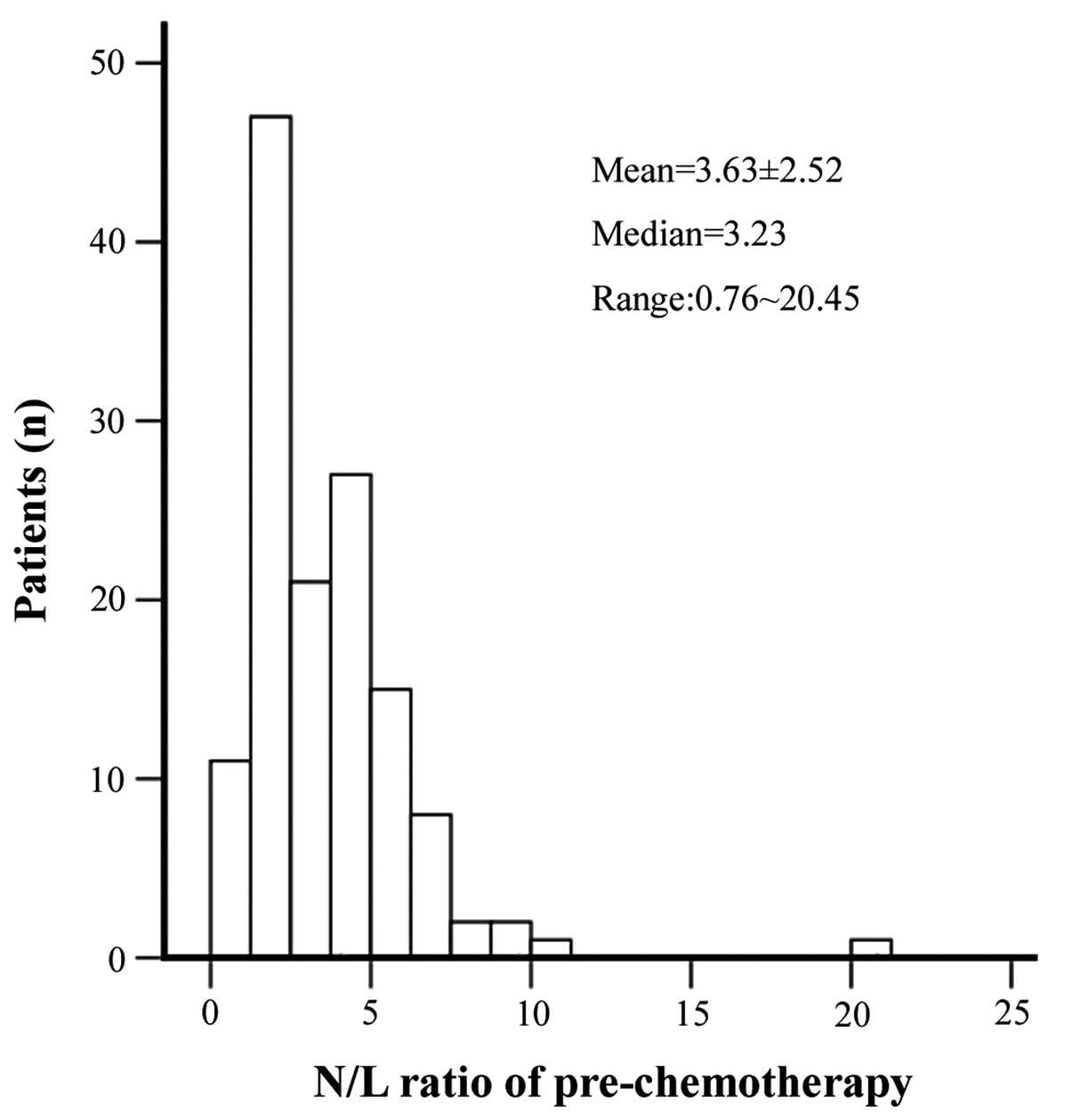
The distribution of the baseline pre-chemo-N/L ratio
in the 135 patients and the post-chemo-N/L ratio were examined. The
median pre-chemo-N/L ratio was 3.23, the mean was 3.63±2.52 (range:
0.76–20.45), with the 25th and 75th percentiles 1.85 and 4.55,
respectively (Fig. 1). The
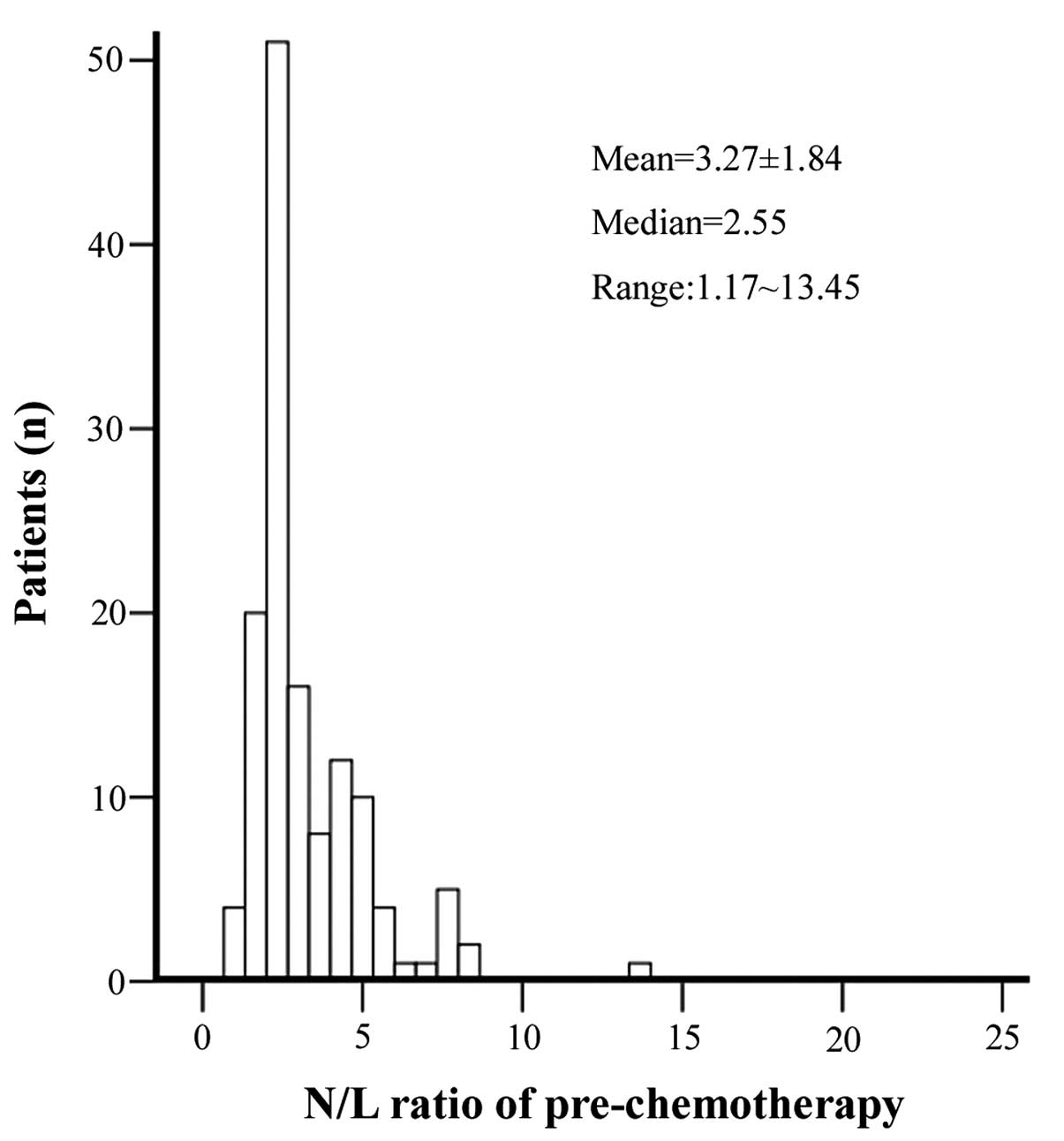
post-chemo-N/L ratio was 2.55, the average was 3.27±1.83 (range:
1.17~13.45), with the 25th and 75th percentiles 2.19 and 4.28,
respectively (Fig. 2). The N/L ratio
of the post-chemotherapy group was significantly reduced compared
with the ratio of the pre-chemotherapy group (P<0.001), as
assessed by Pearson's correlation. The median overall survival rate
was 7.9 months, which is longer compared with those patients not
treated with adjuvant chemotherapy. The N/L ratio of normal
controls is usually <2.0 since the proportions of neutrophils
and lymphocytes in WBCs are ~50–60 and 30–40%, respectively
(16). Thus, compared with normal
controls, the N/L ratio of enrolled patients was significantly
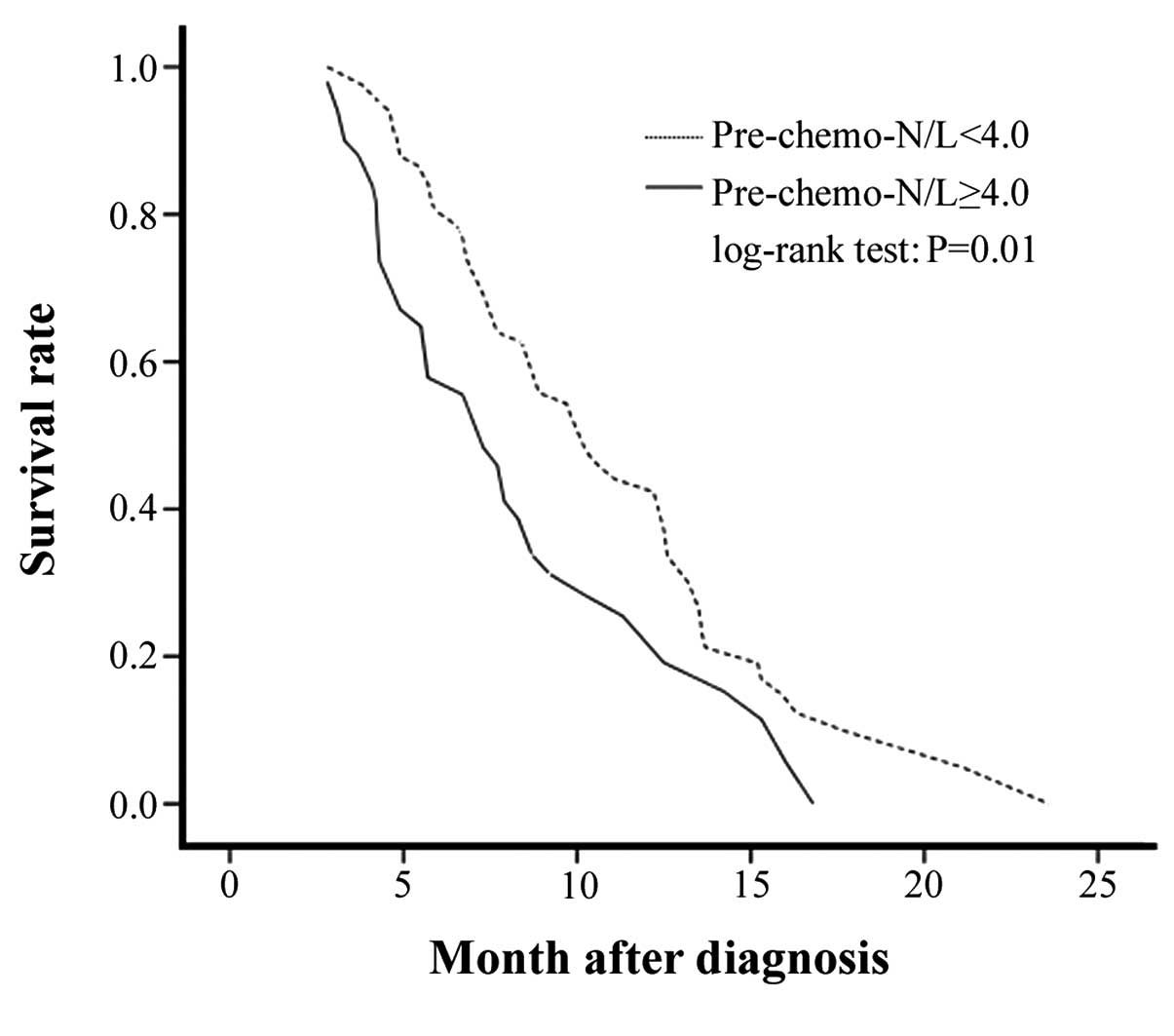
increased. The median overall survival of 8.75 months in the
pre-chemotherapy group with an N/L<4.0, was significantly
increased compared with the 6.7 months for the N/L≥4.0 group
(P=0.01; Fig. 3). The median overall
survival was 9.7 months in the post-chemo-N/L<2.5 group, which
was significantly increased compared with the median survival rate
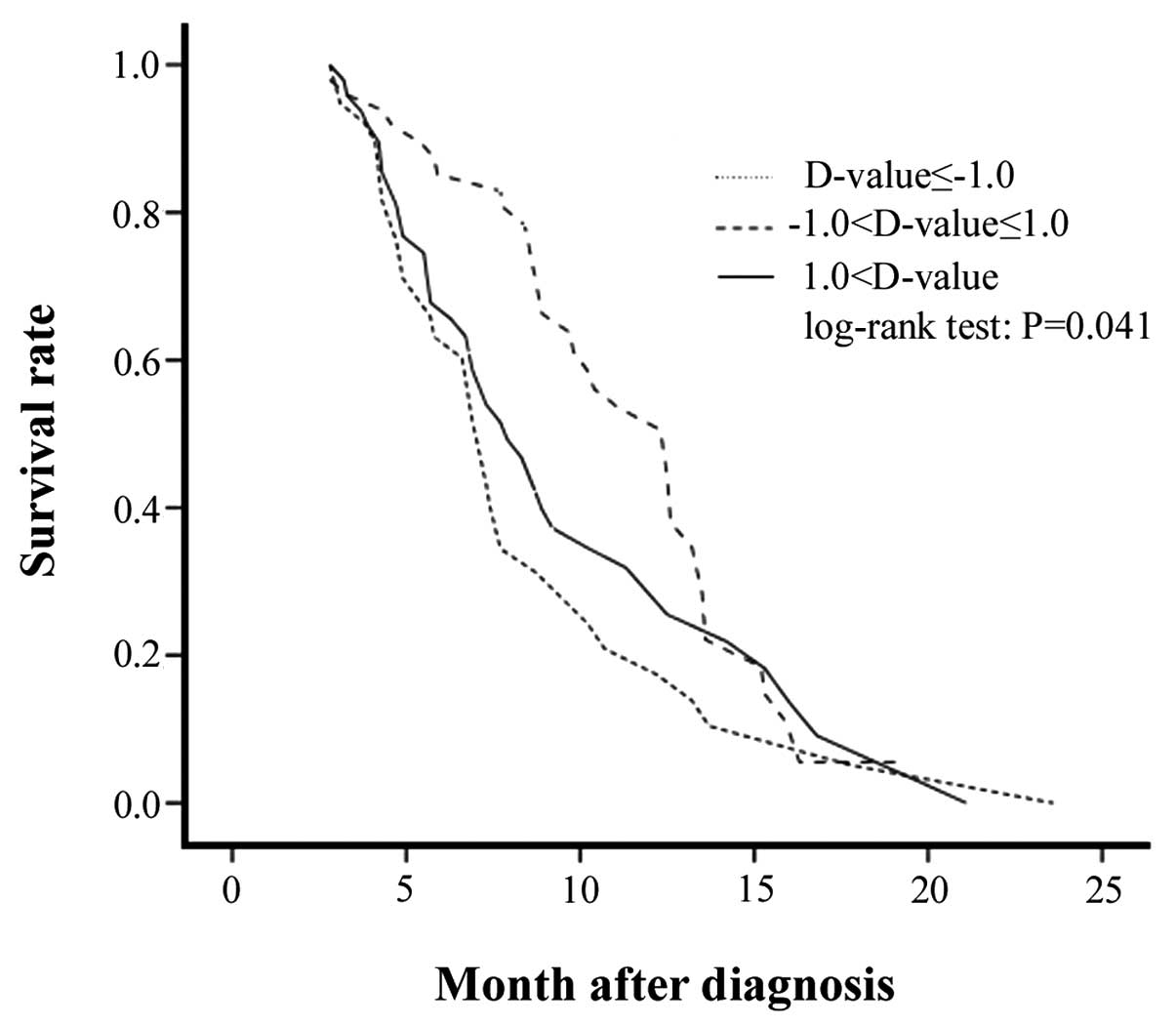
of 7.0 months in the N/L≥2.5 group (P=0.009). In order to assess
the efficacy of the chemotherapy, the D-value was determined by
subtracting the pre-chemo-N/L ratio from the post-chemo-N/L ratio
(Fig. 5), the median survival rate
for patients with a D-value between −1.0 and 1.0 was significantly
increased compared with the patients with D-values outside this
range (9.8 months, P=0.041).
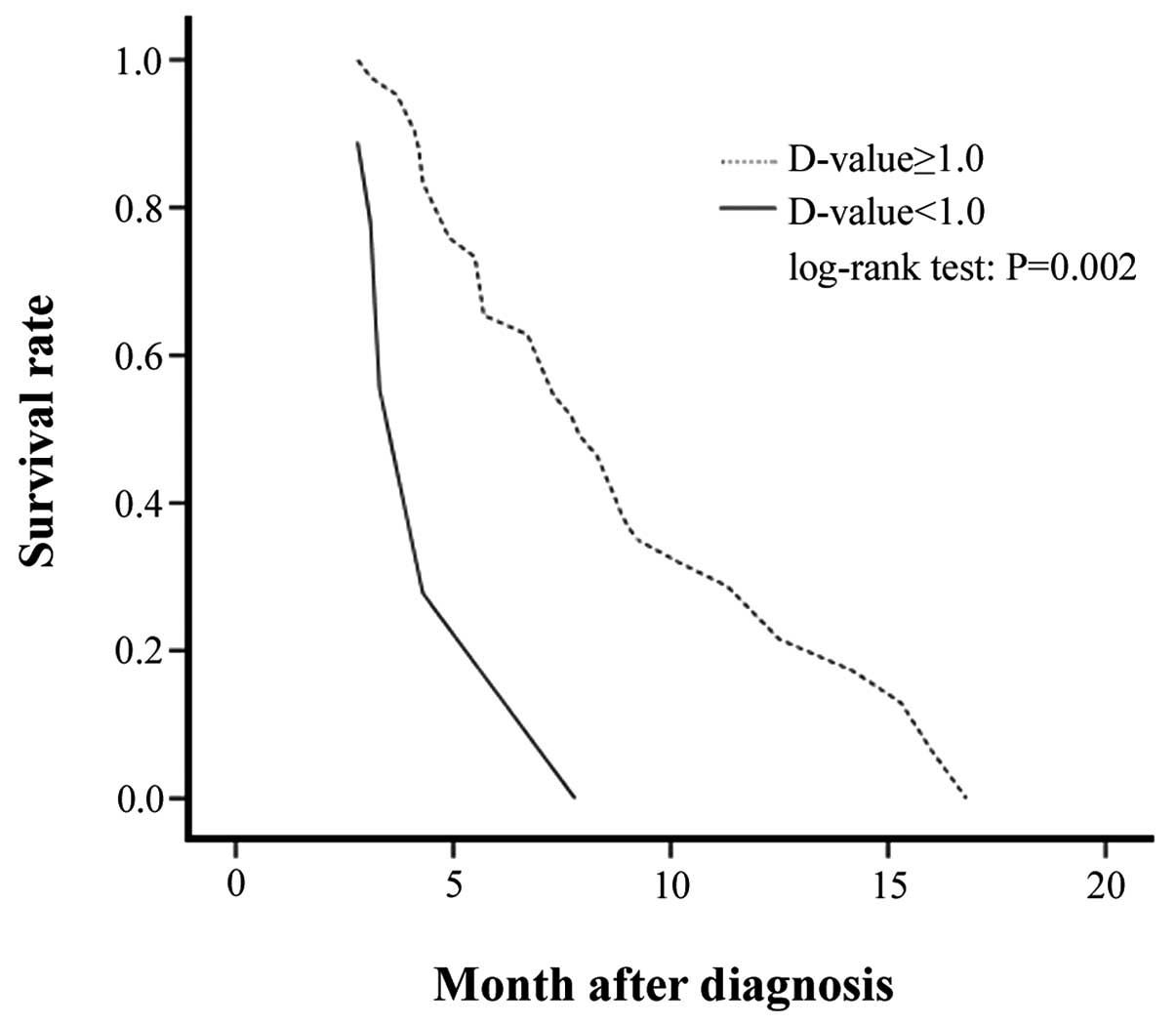
The D-value was also determined by subtracting the
pre-chemo-N/L ratio from the post-chemo-N/L ratio for the patients
who had an N/L ratio ≥4.0 pre-chemotherapy (Fig. 6). The results indicated that the
median survival rate of 7.2 months in patients with a D-value ≥1
was significantly increased compared with the median survival rate
of 3.8 months in patients with a D-value<1 (P=0.002). For the
patients who had an N/L ratio <4.0 pre-chemotherapy, the results
indicated that the median survival rate was 10.9 months in patients
with a D-value <1, which was significantly increased compared
with the 6.9 months for patients with a D-value ≥1 (P=0.001).
Discussion
A number of previous studies have indicated that a
high neutrophil count is correlated with poor prognosis in patients
with various types of cancer, including that of the breast, head
and neck and sarcoma. However, previous findings concerning
advanced cancer types have also demonstrated that a high count of
peripheral neutrophils is an independent prognostic factor for
survival rates (17–22). The prognostic role of the N/L ratio
has also previously been investigated (15).
The N/L ratio is a good indicator for the evaluation
of the condition of a tumor-bearing host (16,23). In
humans, the number of circulating neutrophils (N) are increased in
the daytime (daytime rhythm), while circulating T cells, B cells,
alphabet T cells and CD4+ lymphocytes are increased at
night (24). Fluctuations in the
number of neutrophils are not always in concordance with those of
lymphocytes. The N/L ratio as a relative value may correctly
reflect fluctuations between neutrophils and lymphocytes and the
antitumor efficiency of the host immune mechanism more accurately
than the number of circulating neutrophils alone. In the clinic,
the efficacy of an antibiotic by the neutrophil count may be
predicted, therefore the N/L ratio from a blood test may also
potentially be used as a predictor of chemotherapeutic
efficacy.
In the present study, the baseline N/L ratio in the
peripheral blood of patients with stage IV gastric cancer was
significantly increased compared with the patients who initially
refued chemotherapy (median=3.23). Following chemotherapy, the
baseline N/L ratio was significantly reduced (median=2.55). It may
be that a number of patients benefit simply from the chemotherapy,
thus what type of situation may aid in the prediction of the
effectiveness of chemotherapy remains to be determined. In the
subsequent analysis, an N/L ratio of 4.0 was applied as the cut-off
value for patients prior to chemotherapy. The patients were then
divided into two groups: The patients with an N/L ratio ≥4.0 had a
significantly reduced survival rate compared with those with an N/L
ratio <4.0, which indicates the reduced prognosis of patients
with an increased N/L ratio. In addition, the same results are
observed in the post-chemotherapy group when the N/L ratio is cut
off at 2.5. The D-value was measured by subtracting the
pre-chemo-N/L ratio from the post-chemo-N/L ratio in the high N/L
ratio group (≥4.0); the patients with a D-value ≥1 had a longer
survival rate compared with those with a D-value<1, which
indicates that the former patients benefited from chemotherapy in
contrast to the latter group. In the low N/L ratio group (<4.0),
the patients in D-value<-1 group (pre-chemo-N/L ratio subtracted
the post-chemo-N/L ratio) had a shorter survival rate compared with
those patients with a D-value≥-1, which indicates the former did
not benefit from chemotherapy in the same way as the latter.
However, in all the patients, the survival rates of the patients in
the −1.0<D-value ≤1.0 group was significantly increased compared
to the patients with D-values outside of this range (P=0.041),
which indicates that if the immune system of the host is in good
functioning condition this results in an improved prognosis.
According to the above observations, fluctuations in the N/L ratio
may allow one to predict the efficacy of chemotherapy.
If a treatment is effective against gastric cancer,
the tumor load is reduced following chemotherapy. In a previous
study, a positive linear correlation was observed between tumor
weight and the N/L ratio within an animal model (14), and an increased N/L ratio was
associated with poor prognosis because elevated levels of
granulocytes promote tumor growth by antagonizing tumor-suppressing
lymphocytes. Those results indicate that opposing fluctuations in
the neutrophil and lymphocyte counts may be associated with tumor
progression.
One possible explanation for this association is
that the increased N/L ratio may reflect an enhanced neutrophil
response that promotes tumor growth. Infiltration by lymphocytes
has been reported to indicate the generation of an effective
antitumor cell immune response (25),
and increased lymphocytic infiltration correlates with an improved
prognosis (25–27). However, previous findings have shown
that tumor-infiltrating granulocytes may promote tumor progression
(28), and the involvement of
neutrophils in tumor progression has been investigated. In
vitro and in vivo experiments have demonstrated that an
array of cytokines or other molecules produced by neutrophils
contribute to a growth-stimulating microenvironment for cancer
cells. Notably, in a number of tumor-transplanted animal models,
neutrophils stimulated tumor angiogenesis by increasing
proangiogenic factors, including vascular endothelial growth factor
(29), interleukin-8 (30), matrix metalloproteinase (31) and elastase (32). Therefore, a high density of
circulating neutrophils may exert unfavorable effects on the
tumor-bearing host, leading to a negative correlation between
neutrophil density and patient survival.
Another possible explanation pertaining to the
association of high N/L values and poor prognosis is that
neutrophils may inhibit the immune system. In support of this
theory, neutrophils suppress the cytolytic activity of lymphocytes,
natural killer cells and activated T cells when neutrophils and
lymphocytes from normal healthy donors are cultured together, and
the degree of suppression is proportional to the number of
neutrophils added (11,33). Similarly, an increased N/L ratio has
been demonstrated to be associated with low immunocompetence in
cancer patients (16,34).
In summary, the results of the present study
indicate that the peripheral blood N/L ratio is an independent
indicator of the chemotherapeutic effect on unresectable or
recurrent gastric cancer. The accuracy of risk stratification in
patients with gastric cancer may lead to more appropriate clinical
management in these patients. Therefore, the N/L ratio, which is
measured relatively easily and at low cost, may be utilized as a
potential biomarker of outcome in the clinic. However, further
analyses of the prognostic implications of the N/L ratio in other
types of malignancies are required.
References
|
1
|
Zhang J, Gong F, Li L, Zhao M and Song J:
Diabetes mellitus and the neutrophil to lymphocyte ratio predict
overall survival in non-viral hepatocellular carcinoma treated with
transarterial chemoembolization. Oncol Lett. 7:1704–1710.
2014.PubMed/NCBI
|
|
2
|
Ozdemir Y, Akin ML, Sucullu I, Balta AZ
and Yucel E: Pretreatment neutrophil/lymphocyte ratio as a
prognostic aid in colorectal cancer. Asian Pac J Cancer Prev.
15:2647–2650. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
McNamara MG, Templeton AJ, Maganti M,
Walter T, Horgan AM, McKeever L, Min T, Amir E and Knox JJ:
Neutrophil/lymphocyte ratio as a prognostic factor in biliary tract
cancer. Eur J Cancer. 50:1581–1589. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Williams KA, LabidiGaly SI, Terry KL,
Vitonis AF, Welch WR, Goodman A and Cramer DW: Prognostic
significance and predictors of the neutrophil-to-lymphocyte ratio
in ovarian cancer. Gynecol Oncol. 132:542–550. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Helal TE, Ibrahim EA and Alloub AI:
Immunohistochemical analysis of tumor-infiltrating lymphocytes in
breast carcinoma: Relation to prognostic variables. Indian J Pathol
Microbiol. 56:89–93. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Allard MA, Bachet JB, Beauchet A, Julie C,
Malafosse R, Penna C, Nordlinger B and Emile JF: Linear
quantification of lymphoid infiltration of the tumor margin: A
reproducible method, developed with colorectal cancer tissues, for
assessing a highly variable prognostic factor. Diagn Pathol.
7:1562012. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Slootweg PJ, de Pagter M, de Weger RA and
de Wilde PC: Lymphocytes at tumor margins in patients with head and
neck cancer. Relationship with tumor size, human lymphocyte antigen
molecules, and metastasis. Int J Oral Maxillofac Surg. 23:286–289.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Koshy S, Wu D, Hu X, Tajhya RB, Huq R,
Khan FS, Pennington MW, Wulff H, Yotnda P and Beeton C: Blocking
KCa3.1 channels increases tumor cell killing by a subpopulation of
human natural killer lymphocytes. PLoS One. 8:e767402013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Coussens LM and Werb Z: Inflammation and
cancer. Nature. 420:860–867. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Tabbekh M, MokraniHammani M, Bismuth G and
Mami-Chouaib F: T-cell modulatory properties of CD5 and its role in
antitumor immune responses. Oncoimmunology. 2:e228412013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
el-Hag A and Clark RA: Immunosuppression
by activated human neutrophils. Dependence on the myeloperoxidase
system. J Immunol. 139:2406–2413. 1987.PubMed/NCBI
|
|
12
|
Tabuchi T, Ubukata H, Sato S, Nakata≈ I,
Goto Y, Watanabe Y, Hashimoto T, Mizuta T, Adachi M and Soma T:
Granulocytapheresis as a possible cancer treatment. Anticancer Res.
15:985–990. 1995.PubMed/NCBI
|
|
13
|
Tabuchi T, Ubukata H, Saniabadi AR and
Soma T: Granulocyte apheresis as a possible new approach in cancer
therapy: A pilot study involving two cases. Cancer Detect Prev.
23:417–421. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Liu H and Tabuchi T, Takemura A, Kasuga T,
Motohashi G, Hiraishi K, Katano M, Nakada I, Ubukata H and Tabuchi
T: The granulocyte/lymphocyte ratio as an independent predictor of
tumour growth, metastasis and progression: Its clinical
applications. Mol Med Rep. 1:699–704. 2008.PubMed/NCBI
|
|
15
|
Liu H, Liu G, Bao Q, et al: The baseline
ratio of neutrophils to lymphocytes is associated with patient
prognosis in rectal carcinoma. J Gastrointest Cancer. 41:116–120.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Satomi A, Murakami S, Ishida K, Mastuki M,
Hashimoto T and Sonoda M: Significance of increased neutrophils in
patients with advanced colorectal cancer. Acta Oncol. 34:69–73.
1995. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Donskov F and von der Maase H: Impact of
immune parameters on long-term survival in metastatic renal cell
carcinoma. J Clin Oncol. 24:1997–2005. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Schmidt H, Suciu S, Punt CJ, et al:
American Joint Committee on Cancer Stage IV Melanoma; EORTC 18951:
Pretreatment levels of peripheral neutrophils and leukocytes as
independent predictors of overall survival in patients with
American Joint Committee on Cancer Stage IV Melanoma: Results of
the EORTC 18951 Biochemotherapy Trial. J Clin Oncol. 25:1562–1569.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Négrier S, Escudier B, Gomez F, Douillard
JY, Ravaud A, Chevreau C, Buclon M, Pérol D and Lasset C:
Prognostic factors of survival and rapid progression in 782
patients with metastatic renal carcinomas treated by cytokines: A
report from the Groupe Français d'Immunothérapie. Ann Oncol.
13:1460–1468. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Atzpodien J, Royston P, Wandert T and
Reitz M: DGCIN- German Cooperative Renal Carcinoma
Chemo-Immunotherapy Trials Group: Metastatic renal carcinoma
comprehensive prognostic system. Br J Cancer. 88:348–353. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Hashimoto T, Ohno Y, Nakashima J, Gondo T,
Ohori M and Tachibana M: Clinical significance of preoperative
peripheral blood neutrophil count in patients with non-metastatic
upper urinary tract carcinoma. World J Urol. 31:953–958. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Thavaramara T, Phaloprakarn C,
Tangjitgamol S and Manusirivithaya S: Role of neutrophil to
lymphocyte ratio as a prognostic indicator for epithelial ovarian
cancer. J Med Assoc Thai. 94:871–877. 2011.PubMed/NCBI
|
|
23
|
Hirashima M, Higuchi S, Sakamoto K,
Nishiyama T and Okada H: The ratio of neutrophils to lymphocytes
and the phenotypes of neutrophils in patients with early gastric
cancer. J Cancer Res Clin Oncol. 124:329–334. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Suzuki S, Toyabe S, Moroda T, et al:
Circadian rhythm of leucocytes and lymphocytes subsets and its
possible correlation with the function of the autonomic nervous
system. Clin Exp Immunol. 110:500–508. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Rabinowich H, Cohen R, Bruderman I,
Steiner Z and Klajman A: Functional analysis of mononuclear cells
infiltrating into tumors: Lysis of autologous human tumor cells by
cultured infiltrating lymphocytes. Cancer Res. 47:173–177.
1987.PubMed/NCBI
|
|
26
|
Kloor M: Lymphocyte infiltration and
prognosis in colorectal cancer. Lancet Oncol. 10:840–841. 2009.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Balkwill F and Mantovani A: Inflammation
and cancer: Back to Virchow? Lancet. 357:539–545. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Liu H, Ubukata H, Tabuchi T, et al: It is
possible that tumour-infiltrating granulocytes promote tumour
progression. Oncol Rep. 22:29–33. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Tan KW, Chong SZ, Wong FH, Evrard M, Tan
SM, Keeble J, Kemeny DM, Ng LG, Abastado JP and Angeli V:
Neutrophils contribute to inflammatory lymphangiogenesis by
increasing VEGF-A bioavailability and secreting VEGF-D. Blood.
122:3666–3677. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Chen L, Li Q, Zhou XD, Shi Y, Yang L, Xu
SL, Chen C, Cui YH, Zhang X and Bian XW: Increased pro-angiogenic
factors, infiltrating neutrophils and CD163(+) macrophages in
bronchoalveolar lavage fluid from lung cancer patients. Int
Immunopharmacol. 20:74–80. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Geraghty P, Rogan MP, Greene CM, Boxio RM,
Poiriert T, O'Mahony M, Belaaouaj A, O'Neill SJ, Taggart CC and
McElvaney NG: Neutrophil elastase up-regulates cathepsin B and
matrix metalloprotease-2 expression. J Immunol. 178:5871–5878.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Scapini P, Nesi L, Morini M, Tanghetti E,
Belleri M, Noonan D, Presta M, Albini A and Cassatella MA:
Generation of biologically active angiostatin kringle 1–3 by
activated human neutrophils. J Immunol. 168:5798–5804. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Kay HD and Smith DL: Regulation of human
lymphocyte-mediated natural killer (NK) cell activity. I.
Inhibition in vitro by peripheral blood granulocytes. J
Immunol. 130:475–483. 1983.PubMed/NCBI
|
|
34
|
Ietomi K: A study on the role of
granulocytes in carcinomabearing hosts-G/L ratio as a new host
indicator. Nippon Gan Chiryo Gakkai Shi. 25:662–671. 1990.(In
Japanese). PubMed/NCBI
|