Introduction
Primary central nervous system lymphoma (PCNSL) is
an uncommon intracranial lesion that accounts for <0.7% of all
malignant lymphomas and <1% of intracranial tumors (1). This disease occurs more frequently in
patients who are immunocompromised, including those with diseases
such as acquired immune deficiency syndrome (AIDS), and rarely
occurs in immunocompetent patients (1). In the immunocompetent population, PCNSLs
typically appear in older patients in their fifties and sixties.
However, the incidence of PCNSL in the immunocompetent population
has been reported to have increased >10-fold from 2.5 cases to
30 cases per 10 million population between 1973 and 1992 (2,3). The cause
for the increase in incidence of this disease in the
immunocompetent population is unknown. Surgical resection is
generally ineffective due to the depth of the tumor. Furthermore,
treatment with radiotherapy and corticosteroids often only produce
a partial response, and tumors recur in >90% of patients
(4). Median survival is 10–18 months
in immunocompetent patients, and less in those with AIDS (5). There have been few reports of PCNSL
isolated to the optic nerve without infiltration of the brain,
retina or vitreous, and in the absence of extracranial signs of
non-Hodgkin lymphoma (NHL) (1,6–8).
The current study reports a case of isolated
lymphoma of the optic nerve, optic chiasm and optic tract in an
immunocompetent patient, in whom the diagnosis was determined
postoperatively.
Case report
A 68-year-old female was referred to the
neuro-ophthalmology clinic of Qingdao Municipal Hospital (Qingdao,
China) with bilateral progressive painless loss of vision over a
period of one year leading to blindness in June 2014. The patient's
medical history included open cavity drum-type tympanitis surgery
to the left ear for middle ear cholesteatoma >30 years
previously and a resulting fistula with occasional discharge. No
history of high blood pressure, coronary heart disease or diabetes
mellitus was noted. The patient did not report experiencing any
headaches, fever, nausea, vomiting or weight loss.
The patient developed progressive visual loss in the
right eye for one year without ophthalmalgia, redness or swelling,
and this did not improve following intermittent treatment with
esculin and digitalis glycosides eye drops (one drop, three time a
day) for one year. Blindness had developed in the right eye around
6 months prior to the present admission. Decreased vision was also
reported in the left eye, which did not improve with treatment, and
the left eye had developed blindness 3 days previously. The patient
also reported a sensation of numbness in the legs. Physical
examination revealed no light perception in either eye, and direct
and indirect light reflexes had disappeared. Hearing loss was noted
in the left ear, and limb muscle strength was determined to be
grade 4 (active movement against resistance and gravity), according
to the Manual Muscle Testing grading system (9). A blood test revealed that
triiodothyronine (T3) (1.27 nmol/l; normal range, 1.34–2.73
nmol/l), thyroxine (T4) (64.33 nmol/l; normal range, 78.38–157.4
nmol/l), free T3 (FT3) (3.18 nmol/l; normal range, 3.8–6.0 nmol/l)
and FT4 (7.09 pmol/l; normal range, 7.85–14.41 pmol/l) levels were
reduced, indicating thyroid hypofunction; the results of other
laboratory examinations were within the normal limits, and the HIV
titer was negative.
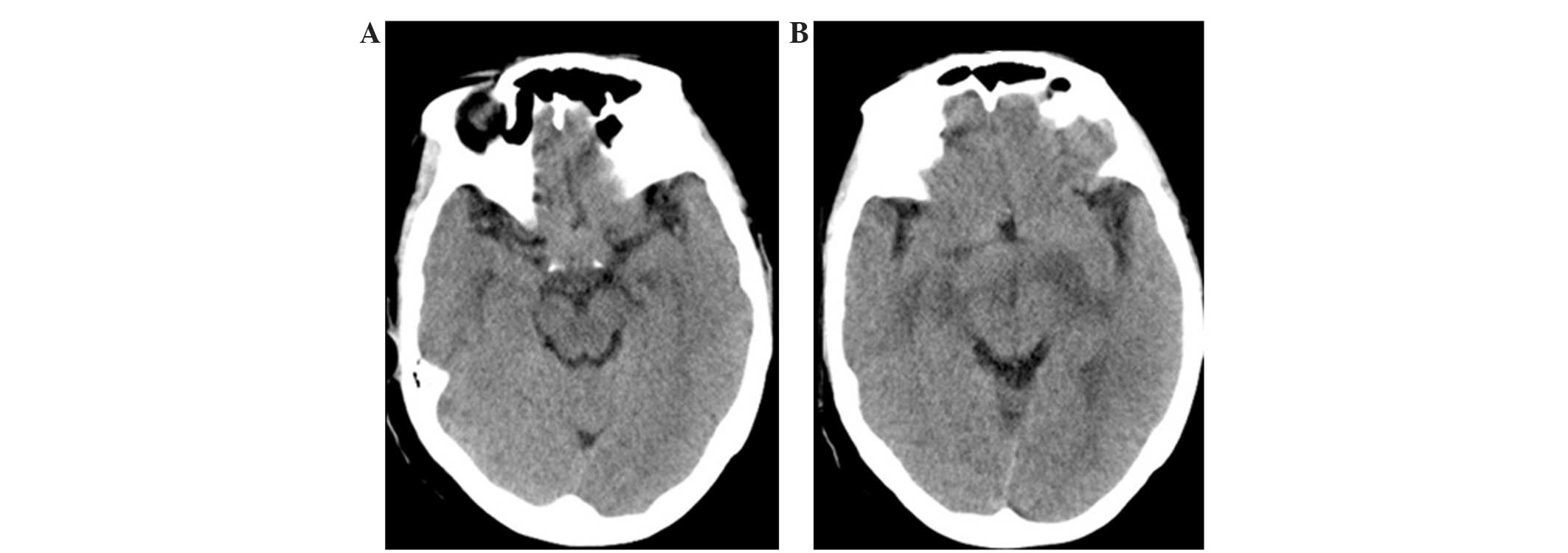
Computed tomography (CT) of the head revealed a
suprasellar isodensity mass (Fig. 1).
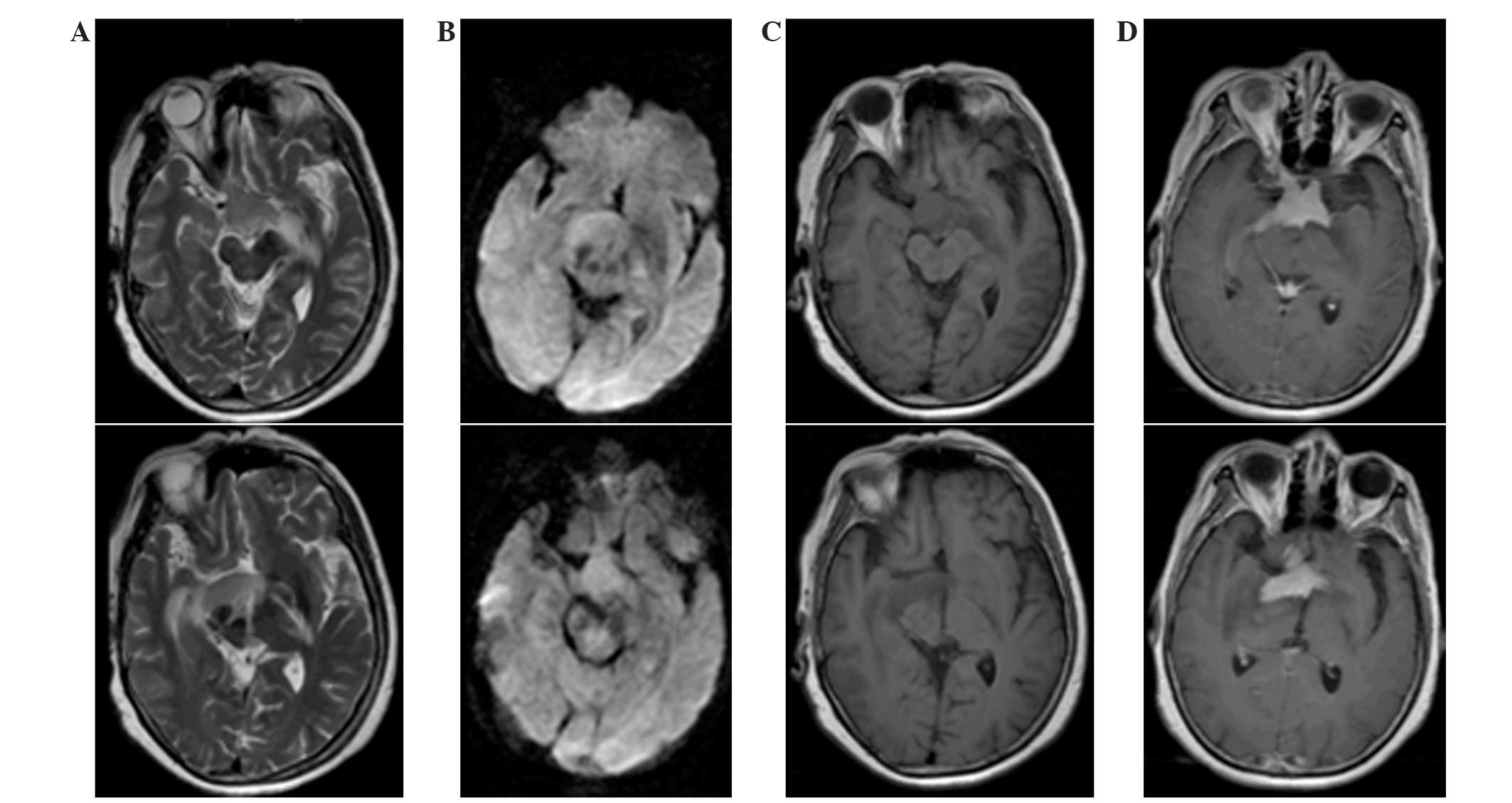
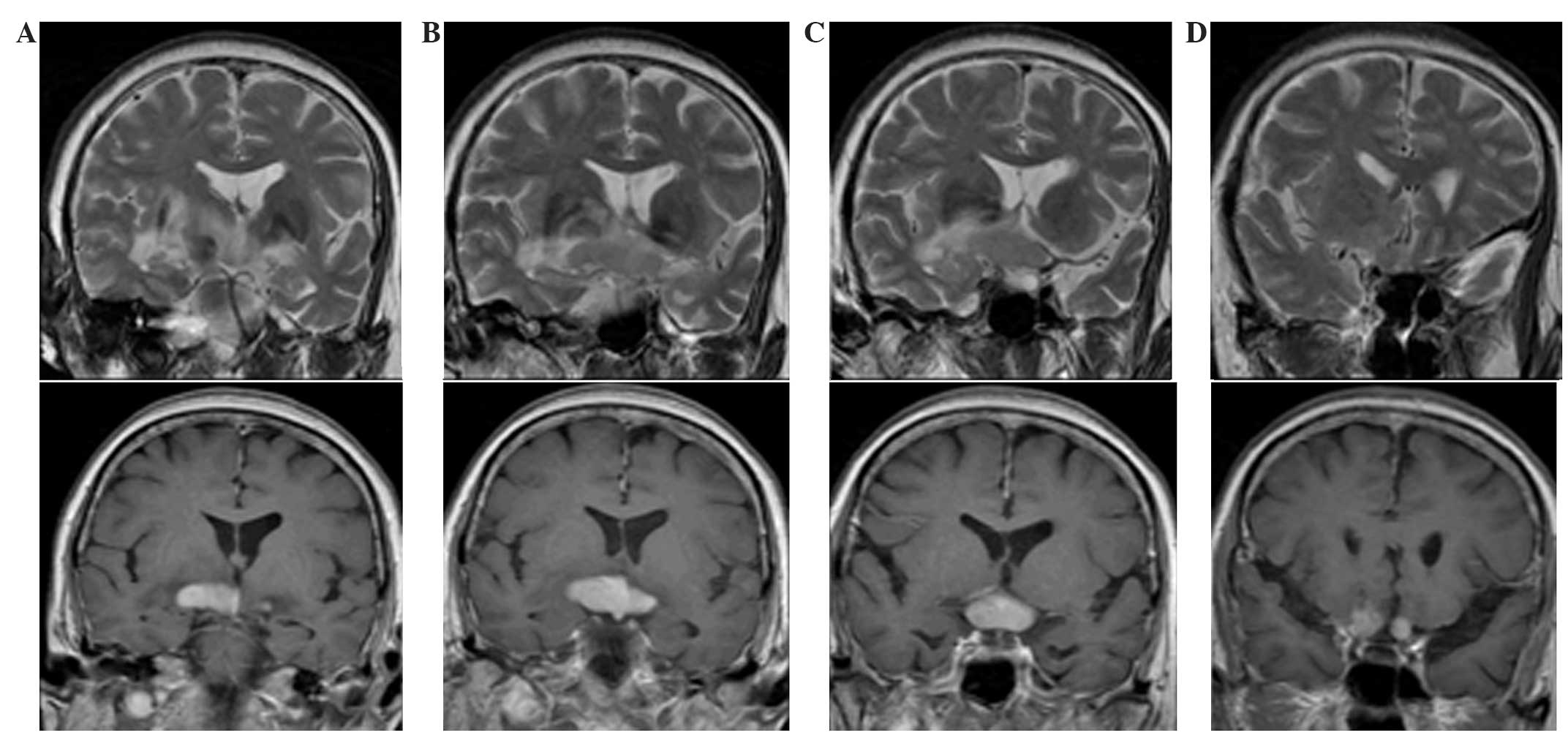
In addition, magnetic resonance imaging (MRI) of the head
demonstrated a suprasellar mass with significant homogenous
enhancement and involvement of the optic chiasm, spreading along
the two optic nerves and the right optic tract (Figs. 2 and 3);
iso-signal intensity to the cortex was observed on T1- and
T2-weighted imaging (WI), and slight hyperintensity on
diffusion-weighted imaging (DWI).
Surgery revealed a thickening of the right optic
nerve, with a diameter of 1 cm. The optic chiasm also appeared
thickened, at 2–3 cm. The tumor was dark red in appearance, with a
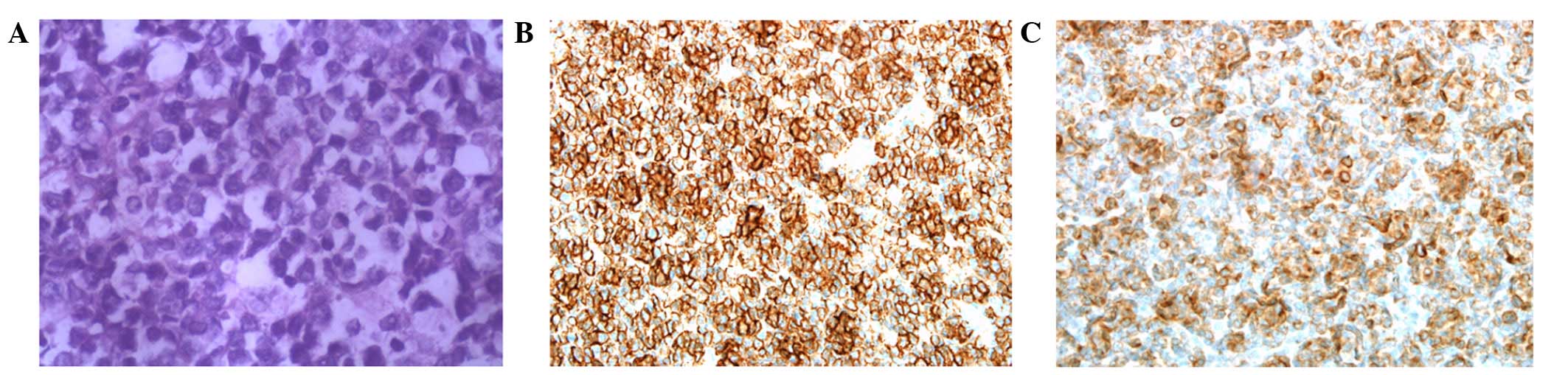
well-defined boundary. Pathological examination of a resected
section of tumor indicated malignancy; complete resection of the
tumor was then performed. Pathology confirmed diffuse malignant
lymphoma type B in the anterior visual pathway: Hematoxylin and
eosin staining revealed macronuclei, less cytoplasm and thickened
chromatin granules, without hemorrhage, necrosis and
calcifications. Immunohistochemical staining revealed that the
tissue was positive for leukocyte common antigen, B lymphocyte
marker CD20 and B-cell antigen receptor Igα CD79a, and negative for
T cell marker CD3 and glial fibrillary acidic protein (Fig. 4).
Postoperative CT of the neck, chest, abdomen and
pelvis revealed no evidence of systemic lymphoma or other medical
conditions. Therefore, the final diagnosis of was PCNSL.
The tumor was completely resected prior to the
administration of radiotherapy (50 Gy in 25 fractions) for five
weeks and eight three-week cycles of the R-CHOP chemotherapy
regimen (375 mg/m2 rituximab, day 1; 750
mg/m2 cyclophosphamide, day 1; 50 mg/m2
doxorubicin, day 1; 1.4 mg/m2 vincristine, day 1; 40
mg/m2 prednisone, days 1–5). The initial response to
radiotherapy was excellent and partial remission was achieved
following the completion of eight cycles of the R-CHOP chemotherapy
regimen. The patient was followed-up by telephone interview, every
three months for one year. At a follow-up examination 12 months
after diagnosis, the patient demonstrated no evidence of
recurrence; however, 14 months after diagnosis the patient
succumbed to the disease.
This study was conducted in accordance with the
declaration of Helsinki and with approval from the Ethics Committee
of Qingdao University. Written informed consent was obtained from
the patient.
Discussion
Imaging findings of PCNSL
Anterior visual pathway involvement from lymphoma
may be divided into three categories: Primary intraocular lymphoma,
PCNSL and secondary metastatic involvement from systemic NHL
(1). PCNSL is predominantly of B cell
origin and is associated with invasion and poor prognosis (10). A number of MRI findings may be
important in the diagnosis of intracranial PCNSL: i) PCNSL is often
observed in the form of focal or multifocal lesions of the cerebral
hemispheres with involvement of the cortical white-matter junction,
the basal ganglia, thalamus and periventricular areas (11); ii) as PCNSL has a high cell density
and high nucleus:cytoplasm ratio on pathology, it may be similar to
other high cell density tumors, such as meningioma, which exhibit
isodense or hyperdense on CT signals and signal intensity close to
the cortical gray matter on T1WI and T2WI MRI (12). However, gliomas often exhibit
hypodensity on CT and hyperintensity on T2WI MRI; iii) PCNSLs
typically exhibit high signal intensity on DWI, as their compact
tumor cells, small extracellular spaces and high nucleus:cytoplasm
ratios restrict diffusion of water in the tumor (13); iv) PCNSLs exhibit moderate homogeneous
enhancement with irregular edges, which may be associated with the
tumor growth along the perivascular space and easy aggregation of
tumor cells (14); v) multifocal
lesions often have regional distribution, and cystic necrosis is
rare (15); and vi) tumors are
sensitive to radiotherapy, and steroid therapy, practical
diagnostic radiotherapy and chemotherapy of suspected cases may aid
in determining a clinical diagnosis if the lesions shrink or
disappear obviously and rapidly (5).
PCNSL may also involve the intraorbital or
intracranial optic nerves, chiasm, radiations or visual cortex. In
addition, studies have reported cavernous sinus or superior orbital
fissure involvement and direct infiltrative or compressive lesions
(e.g., optic nerve, chiasm and tract) (16–22).
Lymphoma involving the chiasm typically occurs due to metastatic
spread of systemic NHL (23–26). PCNSL isolated to the optic chiasm is
extremely rare. Zelefsky et al (7) reported a case of PCNSL in a 72-year-old
previously healthy man. Brain MRI revealed abnormal contrast
enhancement of the intracranial portion of the right optic nerve
and optic chiasm, which extended posteriorly to the right optic
tract and toward the left lateral geniculate body, with the MRI
signal intensity close to that of the cortex (7). Lee et al (1) reported a case of PCNSL involving the
optic chiasm in a patient with AIDS. In the current case, a
suprasellar mass with equal density was identified on CT. The
imaging features included isodensity on plain CT, isointensity to
the cortical gray matter on T1WI and T2WI, and hyperintensity DWI
on plain MRI, while homogeneously marked enhancement of the optic
chiasm, which extended along both optic nerves and the right optic
tract with well-defined boundaries, was observed on enhanced MRI.
The imaging features of the mass involving the optic chiasm in the
current case were generally consistent with the features of
intracranial PCNSL involving other locations as mentioned above,
which suggested the possibility of lymphoma.
Differential diagnosis
With regard to differential diagnosis, there are a
number of other conditions that may be considered. The optic nerve,
optic chiasm and optic tract are collectively known as anterior
visual pathway (27). Whilst the
optic nerve comprises myelinated nerve fibers, no Schwann membranes
are present; therefore, Schwann cell tumors (Schwannomas) seldom
occur in the visual pathway (28).
Meningiomas of the optic chiasm are also extremely rare, and
typically arise from the expansion of optic nerve sheath
meningiomas (29).
Astrocytomas are the most common tumors of the optic
nerve and chiasm, and may be divided into two groups according to
the age of the patient: A pediatric group and an adult group.
Pediatric astrocytomas are more common; pilocytic astrocytoma is
the most common astrocytoma, and such tumors predominantly occur in
children <10 years of age. In adults, astrocytomas are less
common, however, the degree of malignancy is higher than that in
children, and these cases are most frequently anaplastic
astrocytoma or glioblastoma (30). An
association between optic nerve glioma and neurofibromatosis type I
is well established (31). On MRI, an
enlarged optic chiasm, or the formation of mass with a clear
boundary may be observed. The lesions exhibit hypodensity on CT,
whereas equal or high density is observed with PCNSL, and
hypointensity on T1WI and hyperintensity on T2WI, with mild or
significant enhancement, by contrast to the isosignals to the
cortex observed on T1WI and T2WI with significant enhancement in
PCNSL. Furthermore, hyposignal is observed on DWI, whereas
high-signals are exhibited with PCNSL. The cystic lesions can
migrate from the tumor (more common in malignant tumors) (30).
Optic chiasm metastases are rare and predominantly
result from intracranial invasion of retinoblastoma (29). This may appear as a mass spreading
along the optic nerve to the optic chiasm, with an enlarged optic
nerve and chiasm. Distant metastasis to the optic chiasm is very
rare unless the patient has a relevant history of malignant tumor.
MRI may reveal thickening of the optic chiasm with homogeneous and
significant enhancement (32).
Conclusions
Imaging findings of tumors in the optic chiasm are
often similar and it may be difficult to differentiate between them
(29). Gliomas (primarily
astrocytic-origin tumors) are the most common tumor and should
therefore be considered first (30).
Combination of medical history indicating no evidence of other
malignant tumors can help to exclude metastases. Lymphoma in the
optic chiasm is extremely rare; however, optic chiasm tumors with
marked homogeneous enhancement and signals close to the cortex on
T1WI and T2WI, and hyperintensity on DWI in adults, may indicate
lymphoma (1–3,6,7). The inflammatory lesion of the optic
chiasm shows diffuse thickening and significant enhancement, as it
is often associated with inflammation of the surrounding structure,
commonly involving the adjacent dura (29).
In the current case involving relatively rapid and
progressive visual impairment in both eyes in a previously healthy
female and imaging abnormalities, surgery revealed lymphoma. This
case demonstrates the importance of considering such a diagnosis in
this setting.
References
|
1
|
Lee AG, Tang RA, Roberts D, Schiffman JS
and Osborne A: Primary central nervous system lymphoma involving
the optic chiasm in AIDS. J Neuroophthalmol. 21:95–98. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Eby NL, Grufferman S, Flannelly CM, Schold
SC, Vogel FS and Burger PC: Increasing incidence of primary brain
lymphoma in the US. Cancer. 62:2461–2465. 1988. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Corn BW, Marcus SM, Topham A, Hauck W and
Curran WJ: Will primary central nervous system lymphoma be the most
frequent brain tumor diagnosed in the year 2000? Cancer.
79:2409–2413. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Deangelis LM and Hormigo A: Treatment of
primary central nervous system lymphoma. Semin Oncol. 31:684–692.
2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
del Rio M Sierra, Rousseau A, Soussain C,
Ricard D and Hoang-Xuan K: Primary CNS lymphoma in immunocompetent
patients. Oncologist. 14:526–539. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Behbehani RS, Vacarezza N, Sergott RC,
Bilyk JR, Hochberg F and Savino PJ: Isolated optic nerve lymphoma
diagnosed by optic nerve biopsy. Am J Ophthalmol. 139:1128–1130.
2005. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Zelefsky JR, Revercomb CH, Lantos G and
Warren FA: Isolated lymphoma of the anterior visual pathway
diagnosed by optic nerve biopsy. J Neuroophthalmol. 8:36–40. 2008.
View Article : Google Scholar
|
|
8
|
Cantore GP, Raco A, Artico M, Ciappetta P
and Delfini R: Primary chiasmatic lymphoma. Clin Neurol Neurosurg.
91:71–74. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Simon RP, Greenberg D and Aminoff MJ:
Clinical Neurology (7th). McGraw-Hill Medical. New York, NY:
2009.
|
|
10
|
Chimienti E, Spina M, Vaccher E and
Tirelli U: Management of immunocompetent patients with primary
central nervous system lymphoma. Clin Lymphoma Myeloma. 9:353–364.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bühring U, Herrlinger U, Krings T, Thiex
R, Weller M and Küker W: MRI features of primary central nervous
system lymphomas at presentation. Neurology. 57:393–396. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Küker W, Nägele T, Korfel A, Heckl S,
Thiel E, Bamberg M, Weller M and Herrlinger U: Primary central
nervous system lymphomas (PCNSL): Presentation in 100 patients. J
Neuro Oncol. 72:169–177. 2005. View Article : Google Scholar
|
|
13
|
Guo AC, Cummings TJ, Dash RC and
Provenzale JM: Lymphomas and high-grade astrocytomas: Comparison of
water diffusibility and histologic characteristics. Radiology.
224:177–183. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Go JL, Lee SC and Kim PE: Imaging of
primary central nervous system lymphoma. Neurosurg Focus.
21:E42006. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Haldorsen IS, Espeland A and Larsson EM:
Central Nervous system lymphoma: Characteristic findings on
traditional and advanced imaging. AJNR Am J Neuroradiol.
32:984–992. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ikeda T, Hara K, Yamanaka T, Umezu H,
Takahashi H and Nishizawa M: A case of primary central nervous
system malignant lymphoma developing from the optic chiasma and
hypothalamus Rinsho. Shinkeigaku. 46:475–479. 2006.(In
Japanese).
|
|
17
|
Bullock JD, Yanner B, Kelly M and McDonald
LW: Non-Hodgkins lymphoma involving the optic nerve. Ann
Ophthalmol. 11:1477–1480. 1979.PubMed/NCBI
|
|
18
|
Maiuri F: Primary cerebral lymphoma
presenting as steroid-responsive chiasmal syndrome. Br J Neurosurg.
1:499–502. 1987. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Sakai C, Takagi T and Wakatsuki S: Primary
meningeal lymphoma presenting solely with blindness: A report of an
autopsy case. Int J Hematol. 63:325–329. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Strominger MB, Schatz NJ and Glaser JS:
Lymphomatous optic neuropathy. Am J Ophthalmol. 116:774–776. 1993.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Gray RS, Abrahams JJ, Hufnagel TJ, Kim JH,
Lesser RL and Spencer DD: Ghost-cell tumor of the optic chiasm:
Primary CNS lymphoma. J Clin Neuroophthalmol. 9:98–104.
1989.PubMed/NCBI
|
|
22
|
Maiuri F: Visual involvement in primary
non-Hodgkin's lymphomas. Clin Neurol Neurosurg. 92:119–124. 1990.
View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Bolanowski M, Kuliszkiewicz-Janus M and
Sokolska V: Diffuse malignant lymphoma type B with optic chiasm
infiltration, visual disturbances, hypopituitarism,
hyperprolactinaemia and diabetes insipidus. Case report and
literature review. Endokrynol Pol. 57:642–647. 2006.PubMed/NCBI
|
|
24
|
McFadzean RM, McIlwaine GG and McLellan D:
Hodgkin's disease at the optic chiasm. J Clin Neuroophthalmol.
10:248–254. 1990.PubMed/NCBI
|
|
25
|
Sumrall A and Herrin V: Recurrent,
transformed non-Hodgkin's lymphoma presenting as chiasmal syndrome
with hyperprolactinemia and hypopituitarism. J Miss State Med
Assoc. 51:35–36. 2010.PubMed/NCBI
|
|
26
|
Soldevilla HF, Molina RM and Navarra SV:
Breast lymphoma in Sjögren's syndrome complicated by acute
monocular blindness. Int J Rheum Dis. 13:164–170. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Song X, Wang G, Zhang T, Feng L, An P and
Zhu Y: Functional magnetic resonance imaging evaluation of visual
cortex activation in patients with anterior visual pathway lesions.
Neural Regen Res. 7:692–696. 2012.PubMed/NCBI
|
|
28
|
Quesnel AM and Mckenna MJ: Current
strategies in management of intracanalicular vestibular schwanmoma.
Curr Opin Otolaryngol Head Neck Surg. 19:335–340. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Wu R, Wang Z, Xian J, et al: Analysis of
the optic chiasmal lesions by MRI. Zhonghua Fang She Xue Za Zhi.
37:445–448. 2003.(In Chinese).
|
|
30
|
Xian J, Wang Z, Yu W, et al: Imaging
investigations of optic gliomas. Zhonghua Fang She Xue Za Zhi.
38:677–681. 2004.(In Chinese).
|
|
31
|
Listernick R, Louis DN, Packer RJ and
Gutmann DH: Optic pathway gliomas in children with
neurofibromatosis type 1: Consensus statement from the NF1 Optic
Glioma Task Force. Ann Neurol. 41:143–149. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Albert A, Lee BC, Saint-Louis L and Deck
MD: MRI of optic chiasm and optic pathways. AJNR Am J Neuroradiol.
7:255–258. 1986.PubMed/NCBI
|