Introduction
Pulmonary pleomorphic carcinoma (PPC) is a rare
primary malignant tumor in which carcinomatous and sarcomatous
elements occur. The occurrence of the disease is extremely rare,
accounting for only 0.1–0.4% of all reported malignant lung tumors
(1–4).
Patients with PPC are reported to be predominantly male smokers
with a mean age of 66 years (5–8). PPC
generally exhibits an aggressive clinical course, and has a
tendency to grow rapidly and invade adjacent structures in the
early stage. The recurrence after surgical treatment is common, and
systemic metastases are frequently observed in patients with PPC
(8). The prognosis of PPC is
significantly worse than the majority of other subsets of non-small
cell lung cancer (NSCLC) due to its poorer response to chemotherapy
and radiotherapy. The response rate to chemotherapy regimens
commonly used for NSCLC is in the range of 0–17% (2,9) and the
median survival reported for patients with PPC was 5–10 months
(1,2,9). The
present study reports two cases of advanced PPC that were
successfully treated with carboplatin plus paclitaxel chemotherapy
and/or radiotherapy.
Case report
Case 1
A 66-year-old male was admitted to the Otsu Red
Cross Hospital (Otsu, Shiga, Japan) in May 2013, due to a
persistent cough and dyspnea that had persisted for 10 days. The
patient had previously undergone a surgical resection of the colon
due to a gastrointestinal stromal tumor. The patient had also
smoked two packs of cigarettes per day for 37 years. A performance
status score of 1, according to the Eastern Cooperative Oncology
Group (ECOG) scale (10), was
recorded. Computed tomography (CT) of the chest showed a large
tumor, measuring 100×80 mm, in the right lower lobe of the lung,
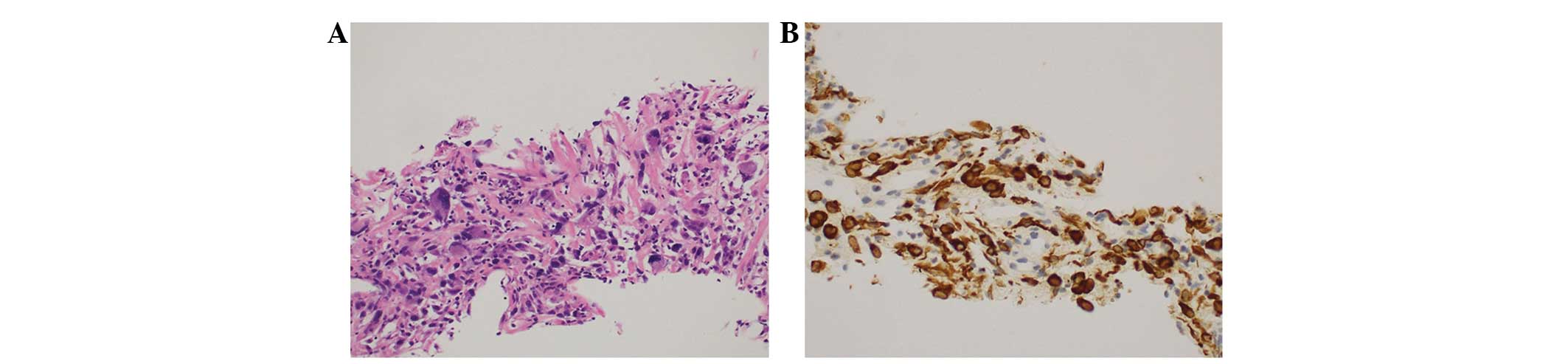
with pleural effusion. An ultrasonography-guided percutaneous lung
biopsy was performed, and the tumor specimen consisted of
epithelioid and sarcomatous cells (Fig.
1A). On immunohistochemical staining, pankeratin was diffusely
positive in the epithelioid and sarcomatous components (Fig. 1B). The patient was diagnosed with PPC
based on the morphological findings of the tumor cells admixed with
sarcomatoid and epithelioid cells. There was no evidence of
metastasis to the other organs, corresponding to a diagnosis of
clinical stage IV (cT4N0M1a) in the TNM classification (11). Subsequent to a thoracentesis, systemic
chemotherapy was administered consisting of carboplatin [area under
the curve (AUC), 6] and paclitaxel (200 mg/m2) on the
first day by intravenous administration every three weeks for four
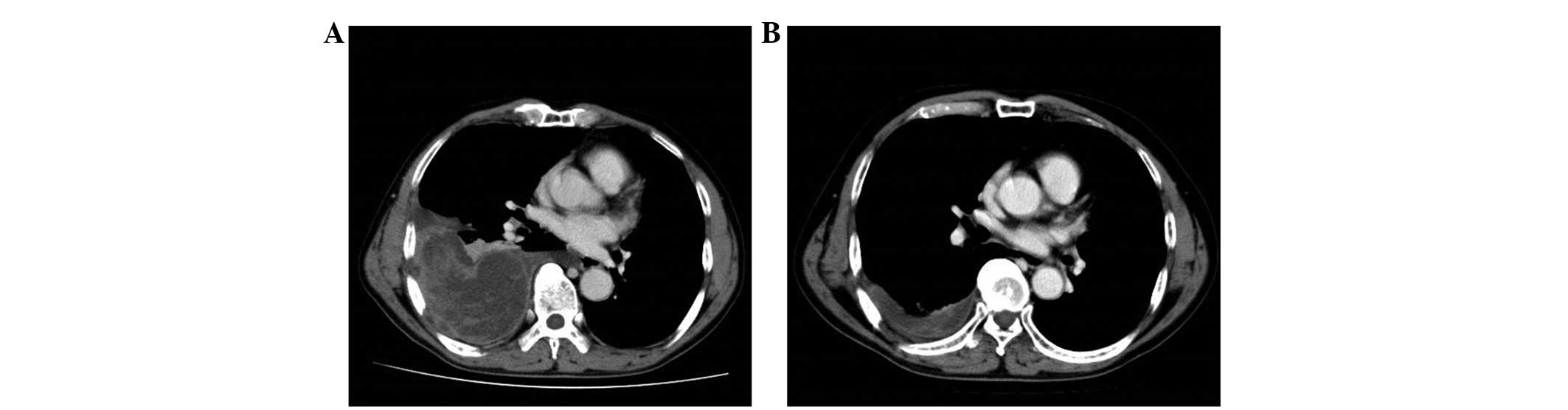
cycles. Following chemotherapy, the tumor was markedly reduced in
size from 100×80 to 75×22 mm, with disappearance of pleural
effusions on chest CT (Fig. 2A and
B), indicating that a partial remission was achieved. Mild
anemia (grade 2), moderate leukopenia (grade 3) and peripheral
neuropathy (grade 3) developed during carboplatin plus paclitaxel
chemotherapy, but were not accompanied by any infectious
complications, and the patient's performance status improved from 1
to 0. The patient is currently alive with no tumor progression at
12 months post-chemotherapy.
Case 2
A 69-year-old male presented with abnormal shadows
in the left middle lung field on a chest X-ray that was taken
during a routine health check, and was admitted to the Otsu Red
Cross Hospital (Otsu, Shiga, Japan) in September 2012. The patient
had a history of chronic obstructive pulmonary disease and was a
smoker of one pack of cigarettes per day for the last 50 years. The
ECOG performance status was 0. CT of the chest showed a lung mass,
measuring 54×42 mm, in the left upper lobe, with enlargement of the
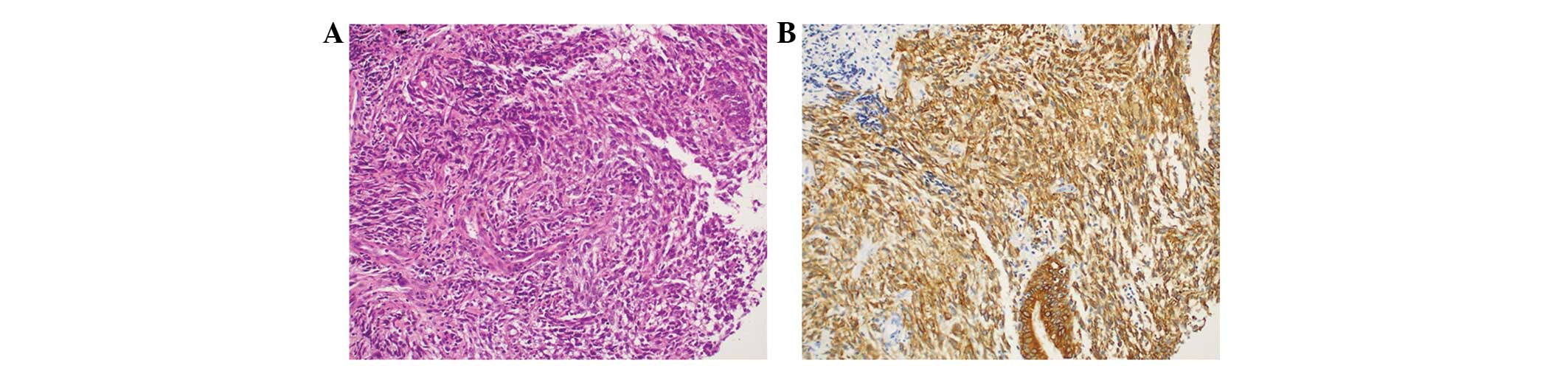
ipsilateral hilar lymph node in addition to emphysema. A
transbronchial lung biopsy was performed, and the tumor cells
exhibited a biphasic appearance, with epithelioid and spindle cell
sarcomatous components (Fig. 3A).
Antibodies against pankeratin were reactive in the epithelioid and
spindle cell sarcomatous components (Fig.
3B), while antibodies against c-kit, carcinoembryonic antigen,
thyroid transcription factor-1 and D2-40 were non-reactive. As a
result, a diagnosis of PPC was made.
18F-fluorodeoxyglucose positron emission tomography
revealed high uptake in the left lung tumor, ipsilateral hilar
lymph node and contralateral mediastinal lymph nodes. There was no
evidence of metastasis to the other organs, corresponding to a
diagnosis of clinical stage IIIB (cT2aN3M0) in the TNM
classification (11). The patient
received carboplatin (AUC, 6) and paclitaxel (200 mg/m2)
every three weeks for three cycles plus concurrent radiation
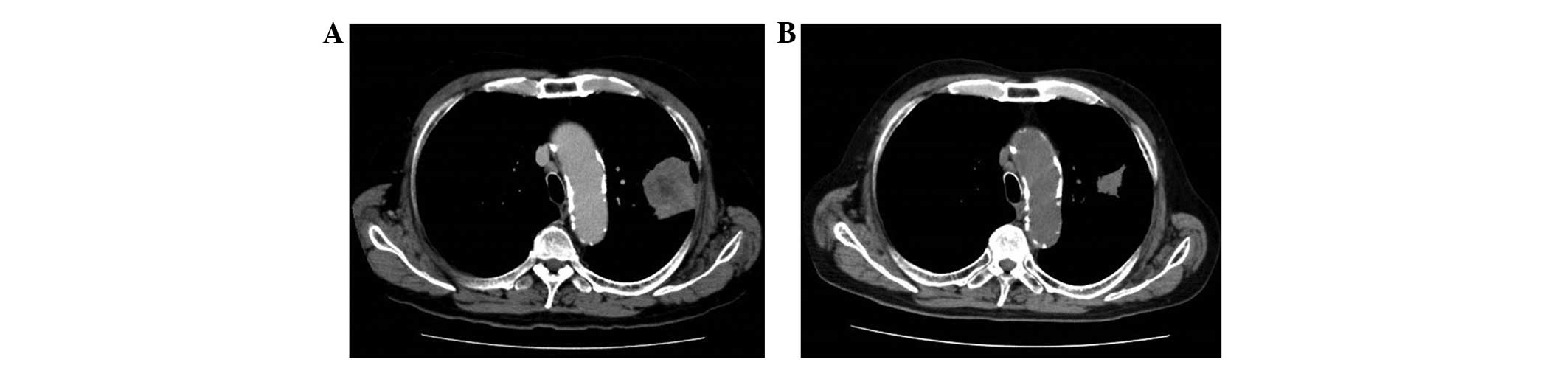
therapy (60 Gy in 30 daily fractions) over a period of 6 weeks. A
marked reduction in tumor size from 54×42 to 18×19 mm was noted
following chemoradiotherapy (Fig. 4A and
B), and a partial remission was achieved. During
chemoradiotherapy, tolerable myelosuppression and neuropathy (grade
2 anemia and leukopenia, and grade 3 neutropenia and peripheral
neuropathy) occurred. The patient is currently alive with no tumor
progression at 21 months post-chemoradiotherapy. The two patients
gave written informed consent to participate in this clinical
study.
Discussion
PPC was first introduced in the third edition of the
World Health Organization (WHO) classifications (12), grouped under the category of
carcinomas with pleomorphic, sarcomatoid or sarcomatous elements.
PPC is defined as a poorly-differentiated NSCLC with ≥10% giant
and/or spindle cell components, or as a carcinoma comprised
completely of giant and spindle cells in the new WHO Classification
of Lung Cancers (13). PPC is
believed to be more aggressive and exhibit a poorer prognosis than
ordinary lung carcinomas (1,3,14). There
are few studies with regard to the chemotherapy of PPC, and its
clinical and pathological characteristics therefore remain unclear.
In patients with advanced or relapsed PPC, the response rate to
chemotherapy regimens that are known to be effective in patients
with NSCLC is only 0–17% (2,9). A previous study reported the cases of
two patients with advanced PPC who showed a partial remission to
chemotherapy with doxorubicin, ifosfamide and dacarbazine. However
these two patients experienced early relapses following cessation
of this combination chemotherapy (15).
The chemosensitivity of surgically-resected PPC has
been evaluated using the histoculture drug response assay in a
previous study (16). The study
demonstrated that taxanes showed a good sensitivity in PPC.
Therefore, it was conceivable that PPC may respond to chemotherapy
that included taxanes. In the present study, two consecutive
patients showed marked responses to carboplatin plus paclitaxel
chemotherapy and/or radiotherapy, and experienced long-term
survival without tumor progression following therapy. In patients
with PPC, it has also been reported that a tumor size of >5 cm,
a clinical stage of greater than stage I and lymph node involvement
confer a significantly poor prognosis (5). Although the two present patients
exhibited these poor prognostic factors, they experienced long-term
survival. The present results suggest that carboplatin plus
paclitaxel chemotherapy and/or radiotherapy may have an important
role in the treatment of patients with advanced PPC.
In conclusion, the present study reported two cases
in which carboplatin and paclitaxel were markedly effective for
PPC. The success with these two cases further suggests that a
multi-institutional study to evaluate treatment with carboplatin
and paclitaxel is warranted.
References
|
1
|
Fishback NF, Travis WD, Moran CA, et al:
Pleomorphic (spindle/giant cell) carcinoma of the lung. A
clinicopathologic correlation of 78 cases. Cancer. 73:2936–2945.
1994. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bae HM, Min HS, Lee SH, et al: Palliative
chemotherapy for pulmonary pleomorphic carcinoma. Lung Cancer.
58:112–115. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Park JS, Lee Y, Han J, et al:
Clinicopathologic outcomes of curative resection for sarcomatoid
carcinoma of the Lung. Oncology. 81:206–213. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Yendamuri S, Caty L, Pine M, et al:
Outcomes of sarcomatoid carcinoma of the lung: A Surveillance,
Epidemiology and End Results Database analysis. Surgery.
152:397–402. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Rossi G, Cavazza A, Sturm N, et al:
Pulmonary carcinomas with pleomorphic, sarcomatoid, or sarcomatous
elements: A clinicopathologic and immunohistochemical study of 75
cases. Am J Surg Pathol. 27:311–324. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Yuki T, Sakuma T, Ohbayashi C, et al:
Pleomorphic carcinoma of the lung: A surgical outcome. J Thorac
Cardiovasc Surg. 134:399–404. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Mochizuki T, Ishii G, Nagai K, et al:
Pleomorphic carcinoma of the lung: Clinicopathologic
characteristics of 70 cases. Am J Surg Pathol. 32:1727–1735. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Ito K, Oizumi S, Fukumoto S, et al:
Clinical characteristics of pleomorphic carcinoma of the lung. Lung
Cancer. 68:204–210. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Hong JY, Choi MK, Uhm JE, et al: The role
of palliative chemotherapy for advanced pulmonary pleomorphic
carcinoma. Med Oncol. 26:287–291. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Oken MM, Creech RH, Tormey DC, et al:
Toxicity and response criteria of the Eastern Cooperative Oncology
Group. Am J Clin Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Goldstraw P, Crowley J, Chansky K, et al:
Proposals for the revision of the TNM stage groupings in the
forthcoming (seventh) edition of the TNM Classification of
malignant tumours. J Thorac Oncol. 2:706–14. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Travis WD, Colby TV, Corrin B, et al:
Histological Typing of Lung Tumors and Pleural Tumors (Third).
Springer Verlag. Berlin: 1999. View Article : Google Scholar
|
|
13
|
Brambilla E, Travis WD, Colby TV, Corrin B
and Shimosato Y: The new World Health Organization classification
of lung tumors. Eur Respir J. 18:1059–1068. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Shannon RL, Ro JY, Grignon DJ, et al:
Sarcomatoid carcinoma of the prostate. A clinicopathologic study of
12 patients. Cancer. 69:2676–2682. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Lee KW, Kim YJ, Kim JH, et al: Two
consecutive cases of platinum-refractory pulmonary pleomorphic
carcinoma that showed dramatic responses to MAID (mesna,
doxorubicin, ifosfamide and dacarbazine) chemotherapy. Jpn J Clin
Oncol. 41:430–433. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kawano R, Hino H, Hoshino T, et al:
Clinicopathological investi- gation of seven resected cases of
pleomorphic carcinoma of the lung and the results of their
chemosensitivity tests. Haigan (Jpn J Lung Cancer). 48:106–111.
2008.(In Japanese). View Article : Google Scholar
|