Introduction
Acute gastrointestinal bleeding is a common medical
emergency, which is most often a result of peptic ulceration,
invasive esophageal inflammation, esophageal and gastric varices,
and malignant tumors (1). Of
colorectal cancers, 34.5% present with chronic melena, commonly
associated with erosion and hemorrhage of the primary tumor
(2). A number of cases of patients
presenting with acute massive hemorrhage from the rectum have been
reported (3–7). Acute massive hemorrhage from the upper
gastrointestinal tract is rare in patients with colorectal cancer.
Thorpe et al (8) reported one
case of a patient with acute gastric bleeding caused by colorectal
cancer involving the distal transverse colon, with a fistulous
communication to the stomach. In patients in whom the primary
colonic tumor has been resected, common reasons for bleeding
include duodenal stress ulcers and anastomotic fistulae (9). The present report discusses a case of
severe esophageal hemorrhage in a patient with colorectal cancer,
with good surgical wound healing and no local recurrence, in whom
anticancer treatment was proposed to be the primary cause of
bleeding.
Case report
A 72-year-old Chinese male underwent a radical right
hemicolectomy for colorectal cancer (pT4N0M0, Stage II) in a Xijing
Hospital (Xi'an, China) in February 2011. The pathology report
revealed an ulcerative adenocarcinoma in the ascending colon with
infiltration to surrounding fatty tissues, without lymph node
involvement and with a negative surgical margin. Genetic analysis
indicated the presence of the K-ras mutation (G12D) and UGT1A1 6/7
type. The patient was considered as high risk stage II, and
therefore received adjuvant chemotherapy with 6 cycles of FOLFOX4
and regular follow-up. Abdominal enhanced CT and PET-CT scans
demonstrated multiple liver nodes in October 2011, two months after
the administration of adjuvant chemotherapy. This confirmed the
presence of unresectable liver metastases. Subsequently,
anti-angiogenesis therapy with bevacizumab, and chemotherapy with
the FOLFIRI regimen [irinotecan, 180 mg/m2 IV over 90
min; folinic acid, 400 mg/m2 IV over 2 h; 5-fluorouracil
(5-FU), bolus of 400 mg/m2 IV; 5-FU, continuous infusion
of 2400 mg/m2 46 h] and bevacizumab (5 mg/kg IV over 90
min) were administered in Xijing Hospital. On day 2, the patient
presented with severe diarrhea, which abated following treatment
with loperamide. The following day, the patient developed abdominal
pain, abdominal bloating and vomiting, and was unable to defecate.
An abdominal X-ray demonstrated intestinal obstruction. Supportive
therapy was administered until the symptoms had resolved. On day 7,
the patient's blood count indicated severe bone marrow toxicity of
grade IV, with white blood cells of 0.9×109/l.
Granulocyte-colony stimulating factor was administered for five
days, and the patient's white blood cell count increased to
10×109/l. On day 12, the patient vomited 600 ml fresh
blood, following a period of nausea, and also excreted 400 ml black
stools. The initial physical examination demonstrated weakness and
pallor, with normal vital signs. The laboratory tests showed that
the fecal occult blood test was positive (3+), the serum albumin
was 28.2 g/l and the initial hemoglobin was 10.1 g/dl. Therefore,
the patient was treated with fluid replacement, octreotide and
losec, and noradrenaline was infused through a nasogastric tube.
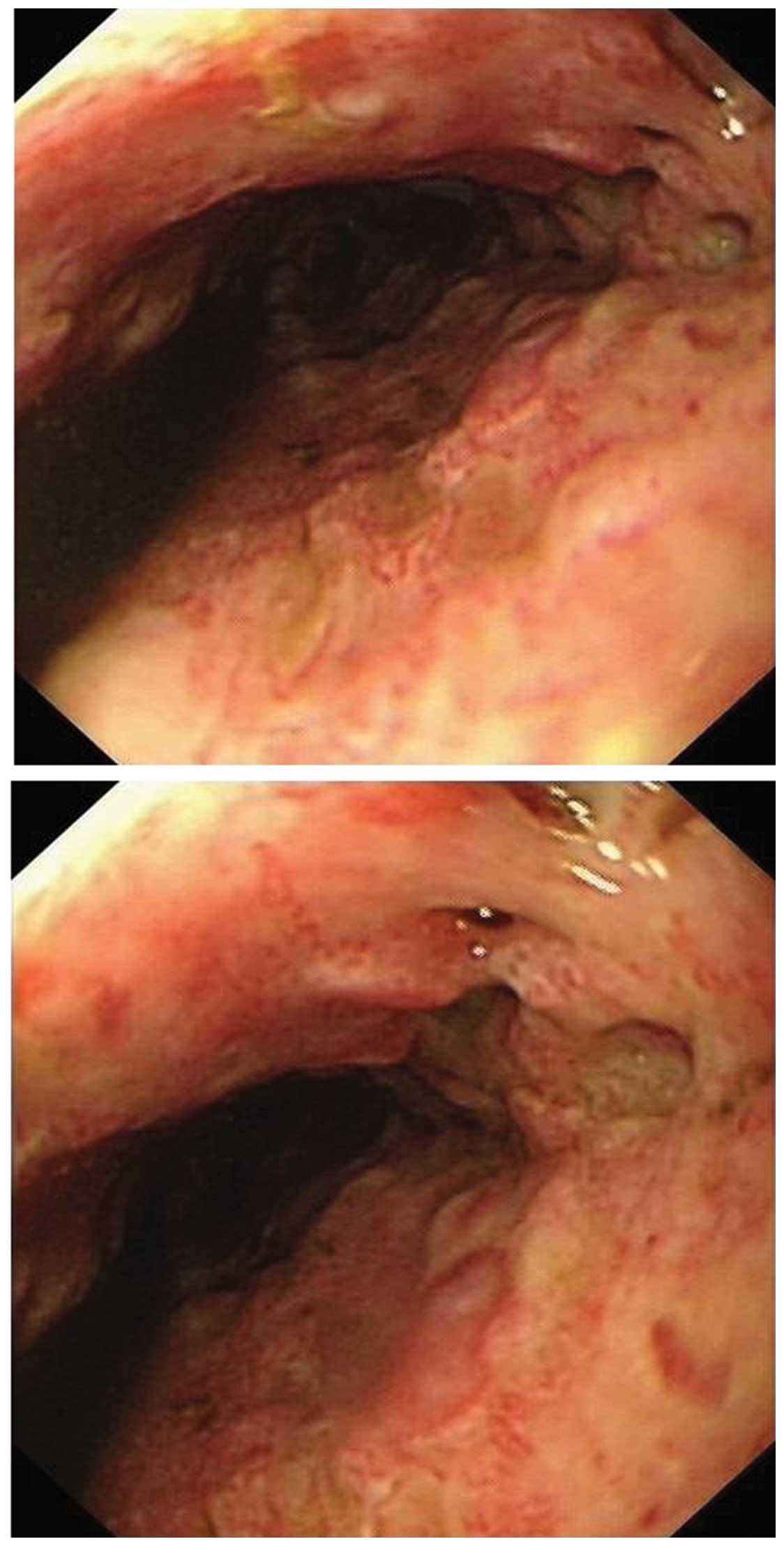
When the patient had been stabilized, an endoscopy was conducted.
This demonstrated diffuse ulceration and fistulae in the submucosa
of the esophagus, old hemorrhage, mild hyperemia and scattered
erosions in the mucosa of the gastric body, as well as in the
gastric antrum and duodenum (Fig. 1).
The patient had undergone an endoscopy in January 2011, during
which no obvious abnormalities were detected. Furthermore, the
colonoscopy did not show any evidence of tumor relapse or a
bleeding lesion. The following day, the patient developed shock,
with a blood pressure of 60/30 mmHg, a temperature of 38.9°C,
tachycardia at 126 beats/min and hemoglobin of 6.9 g/dl. Massive
upper gastrointestinal bleeding was suspected. Following
transfusion with two units of red blood cells, four units of
plasma, and treatment with antibiotics and dopamine, the patient's
condition improved.
Written informed consent for the present study was
obtained from the patient.
Discussion
In the case reported, a patient who had undergone
excision of the primary tumor and exhibited no evidence of local
relapse, developed acute severe esophageal bleeding after one cycle
of the FOLFIRI regimen and bevacizumab. Colonoscopy of the entire
colorectal tract, demonstrated neither relapse nor a bleeding
lesion. Gastroscopy showed diffuse ulceration and fistulae in the
esophageal submucosa, which were presumed to be bleeding lesions.
The occurrence of bleeding may have been a result of mucosal injury
caused by chemotherapy, mucosal vascular dysfunction induced by
bevacizumab or the combined effects of both. Yokoyama et al
(10) reported that during continuous
infusion chemotherapy with 5-FU, two patients presented with bloody
stools secondary to enterocolitis. In a separate report, eight
patients with hepatic cell carcinoma presented with massive
bleeding caused by injury of the gastroduodenal artery, secondary
to extravasation of 5-FU during hepatic arterial chemoperfusion
(11). Chemotherapy with irinotecan
may result in a colonic tumor bleeding directly or indirectly. The
incidence of gastrointestinal bleeding from a primary tumor was 4%,
in a study examining the effect of the AIO regimen (weekly
high-dose 5-FU as a 24-h infusion plus folinic acid) in patients
with colorectal cancer (12).
Yokoyama et al (10) also
reported one patient who developed acute massive gastrointestinal
bleeding on the 31st day after the first cycle of irinotecan-based
chemotherapy, caused by a tumor of the transverse colon that had
metastasized from lung cancer. Irinotecan is known to cause severe
diarrhea, particularly in patients in whom the UGT1A1 gene is of
the 7/7 type, which further induces bleeding, secondary to
enterocolitis (10). Moriwaki et
al (13) reported that the
incidence of bleeding was higher in a group treated with irinotecan
following an oxaliplatin regimen (6/115), compared with that in a
group treated with oxaliplatin following an irinotecan regimen
(0/45). Secondly, bevacizumab, a monoclonal antibody against the
vascular endothelial growth factor receptor, increases the efficacy
when given, in combination with chemotherapy, to patients with
metastatic colorectal cancer. Anti-angiogenesis agents may lead to
dysfunction of vascular endothelial cells and decrease their
capacity for regeneration, which contributes to bleeding. In terms
of adverse effects [categorized according to the Common Toxicity
Criteria of the National Cancer Institute (14)], Hurwitz et al (15) reported that the incidence of grade 3
or 4 bleeding was higher in patients administered the irinotecan,
bolus fluorouracil, and leucovorin (IFL) regimen plus bevacizumab
(3.1%) when compared with those receiving the IFL regimen without
bevacizumab (2.5%). Furthermore, Giantonio et al (16) reported that the incidence of grade 3
or 4 bleeding was higher in patients receiving the FOLFOX4 regimen
plus bevacizumab (3.4%) when compared with patients treated with
the FOLFOX4 regimen alone (0.4%) or bevacizumab alone (2.1%). In
addition, various bleeding locations were reported, including the
primary tumor, articular cavities, the eyeball, and encephalic and
perinephric spaces (17–19). The primary tumor was the most common
bleeding site, accounting for 2.7% of cases. Tsuchida et al
(20) reported a case of a patients
with colorectal cancer, who presented with anal bleeding caused by
shrinkage of an area of local relapse, following treatment with
XELOX and bevacizumab.
Although there are numerous causes of upper
gastrointestinal bleeding, the principles of treatment are similar.
Once hemorrhage occurs, all potentially causative drugs should be
stopped immediately. Vital signs should be closely monitored, and
anticoagulant drugs, fluid infusion and blood transfusion
administered as required. The timing of endoscopy should be
assessed on an individual basis. There are risks associated with
performing an emergency endoscopy. However, it carries diagnostic
and therapeutic benefits when performed by experienced doctors. In
the present case, when bleeding was confirmed, supportive therapy
and endoscopy were instigated appropriately.
In conclusion, during the treatment of advanced
colorectal cancer, particularly in patients treated with
chemotherapy combined with anti-angiogenesis agents, it is
important to remain aware of the possibility of gastrointestinal
bleeding, to consider uncommon sources of such bleeding and to
provide effective and timely management. Once bleeding is
confirmed, intervention should be provided promptly. Even when
severe bleeding occurs, satisfactory outcomes may be achieved with
expeditious active treatment.
Acknowledgements
This study was funded by the National Natural
Science Foundation of China (grant nos. 81102013 and 81201640).
References
|
1
|
El-Tawil AM: Trends on gastrointestinal
bleeding and mortality: Where are we standing? World J
Gastroenterol. 18:1154–1158. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Courtney RJ, Paul CL, Sanson-Fisher RW,
Macrae FA, Attia J and McEvoy M: Factors associated with
consultation behaviour for primary symptoms potentially indicating
colorectal cancer: A cross-sectional study on response to symptoms.
BMC Gastroenterol. 12:1002012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chen CW, Jao SW, Wu CC, Ou JJ, Hsiao CW
and Chao PC: Massive lower gastrointestinal hemorrhage caused by a
large extraluminal leiomyoma of the colon: Report of a case. Dis
Colon Rectum. 51:975–978. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Casarella WJ, Kanter IE and Seaman WB:
Right-sided colonic diverticula as a cause of acute rectal
hemorrhage. N Engl J Med. 286:450–453. 1972. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Leitman IM, Paull DE and Shires GT 3rd:
Evaluation and management of massive lower gastrointestinal
hemorrhage. Ann Surg. 209:175–180. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Al Qahtani AR, Satin R, Stern J and Gordon
PH: Investigative modalities for massive lower gastrointestinal
bleeding. World J Surg. 26:620–625. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Imdahl A, Salm R, Rückauer K and Farthmann
EH: Diagnosis and management of lower gastrointestinal hemorrhage.
Retrospective analysis of 233 cases. Langenbecks Arch Chir.
376:152–157. 1991.(In German). View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Thorpe B, Applebaum B, Esquivel RF, Krouse
RS and Fass R: Colon cancer presenting as upper-GI bleeding.
Gastrointest Endosc. 63:343–345. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gralnek IM: Gastrointestinal bleeding.
Gastrointest Endosc. 76:506–509. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yokoyama T, Kondo H, Yokota T, Tokue Y,
Saito D, Shimada Y and Sugihara K: Colonoscopy for frank bloody
stools associated with cancer chemotherapy. Jpn J Clin Oncol.
27:111–114. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Ross WB, Morris DL and Clingan PR: Major
upper gastrointestinal haemorrhage associated with hepatic arterial
chemoperfusion. Aust NZ J Surg. 66:816–819. 1996. View Article : Google Scholar
|
|
12
|
Koucky K, Wein A, Konturek PC, Albrecht H,
Reulbach U, Männlein G, Wolff K, Ostermeier N, Busse D, Golcher H,
et al: Palliative first-line therapy with weekly high-dose
5-fluorouracil and sodium folinic acid as a 24-hour infusion (AIO
regimen) combined with weekly irinotecan in patients with
metastatic adenocarcinoma of the stomach or esophagogastric
junction followed by secondary metastatic resection after
downsizing. Med Sci Monit. 17:CR248–CR258. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Moriwaki T, Bando H, Takashima A, Yamazaki
K, Esaki T, Yamashita K, Fukunaga M, Miyake Y, Katsumata K, Kato S,
et al: Bevacizumab in combination with irinotecan, 5-fluorouracil,
and leucovorin (FOLFIRI) in patients with metastatic colorectal
cancer who were previously treated with oxaliplatin-containing
regimens: A multicenter observational cohort study (TCTG 2nd-BV
study). Med Oncol. 29:2842–2848. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Trotti A, Colevas AD, Setser A, et al:
CTCAE v3.0: development of a comprehensive grading system for the
adverse effects of cancer treatment. Semin Radiat Oncol.
13:176–181. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Hurwitz H, Fehrenbacher L, Novotny W, et
al: Bevacizumab plus irinotecan, fluorouracil, and leucovorin for
metastatic colorectal cancer. N Engl J Med. 350:2335–2342. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Giantonio BJ, Catalano PJ, Meropol NJ, et
al: Eastern Cooperative Oncology Group Study E3200: Bevacizumab in
combination with oxaliplatin, fluorouracil, and leucovorin
(FOLFOX4) for previously treated metastatic colorectal cancer:
Results from the Eastern Cooperative Oncology Group Study E3200. J
Clin Oncol. 25:1539–1544. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Hayashi H, Okamoto I and Nakagawa K:
Perirenal hematoma associated with bevacizumab treatment. Invest
New Drugs. 30:808–809. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Khasraw M, Holodny A, Goldlust SA and
DeAngelis LM: Intracranial hemorrhage in patients with cancer
treated with bevacizumab: The Memorial Sloan-Kettering experience.
Ann Oncol. 23:458–463. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Uysal M, Goksu SS, Coskun HS, Savas B,
Ozdogan M and Bozcuk H: Intraarticular hemorrhage due to
bevacizumab in a patient with metastatic colorectal cancer: A case
report. J Med Case Rep. 6:1882012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Tsuchida K, Honjoh Y, Asari M, Osawa E,
Numata K, Yoshida T, Osaragi T, Yoneyama K, Kasahara A, Yamamoto Y,
et al: A case of rectal hemorrhage during chemotherapy with
bevacizumab for local recurrence of rectal cancer. Gan To Kagaku
Ryoho. 39:675–677. 2012.(In Japanese). PubMed/NCBI
|