Introduction
Choriocarcinoma is a rare and highly malignant
neoplasm classed among the gestational trophoblastic diseases
(1). Choriocarcinoma is associated
with molar pregnancy, a rapid rate of hematogenous spread to
multiple organs and increased levels of β-human chorionic
gonadotropin (β-HCG), and is also associated with a positive
response to chemotherapy (2,3). Choriocarcinoma primarily occurs in
females of childbearing age and is rarely observed subsequent to
menopause (1). Primary symptoms
outside the uterus, including lung, bone and skin metastases, are
particularly uncommon. The present report outlines a case of
postmenopausal high-risk choriocarcinoma [International Federation
of Gynecology and Obstetrics (FIGO) stage IV, World Health
Organization (WHO) score 13] in a 68-year-old female, who was
identified due to the presence of a pulmonary lesion and surface
masses. Written informed consent was obtained from the patient's
family.
Case report
A 68-year-old female, presenting with a prolonged
cough with expectoration for three months, was admitted to the
Pneumology Department of The Third Affiliated Hospital of Zunyi
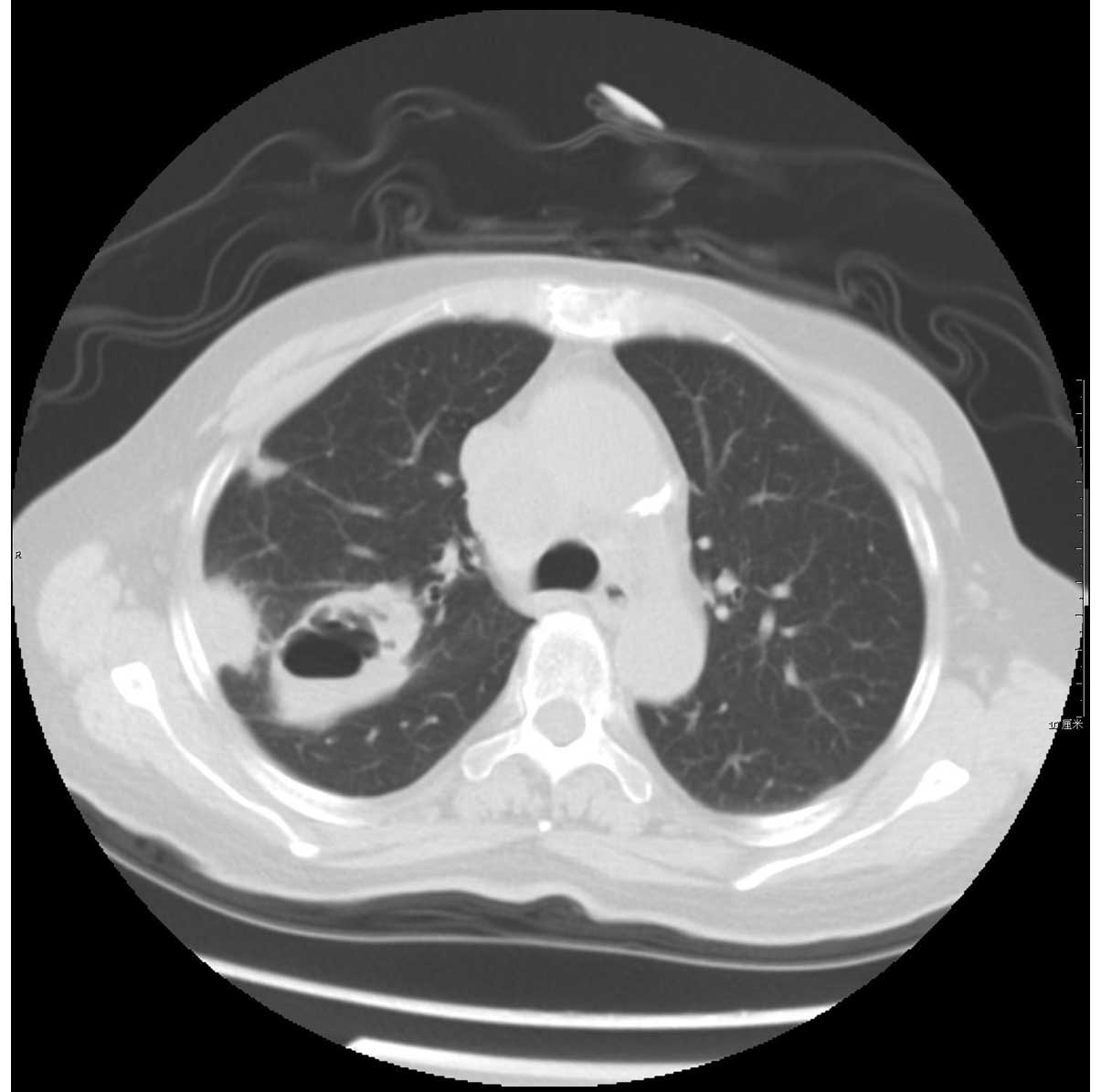
Medical College (Zunyi, China). A chest computed tomography (CT)
scan, performed three months prior to admission, had revealed a
number of nodular opacities with blurred edges in the right upper
lobe of the lung. The largest opacity measured 3.6×3.7 cm, and
exhibited focal cavitation, without enlargement of intrapulmonary
or mediastinal lymph nodes. A diagnosis of a lung abscess due to
secondary pulmonary tuberculosis was reached, and the patient was
administered cefotaxime (2 g, every 12 h) and levofloxacin (0.2 g,
every 12 h) for 2 weeks to treat the infection, and rifampin (0.45
g, once daily), isoniazid (0.3 g, once daily) and ethambutol (0.75
g, once daily) for 3 months to treat the tuberculosis. However, the
patient was subsequently readmitted to hospital three months later,
exhibiting aggravated symptoms, including headaches and anorexia.
Once admitted, the patient continued to receive the therapy regime
comprised of the aforementioned antibiotics and anti-tuberculosis
medication. On day 6 following admission, the patient became
febrile (38–39.7°C). Lymph nodes of the neck were swollen, and two
masses were identified on the patient's scalp, measuring ~3×3 and
3×4 cm, respectively. Consequently, a lymph node biopsy was
performed, during which cytological examination detected the
presence of oncocytes. Serum tumor markers were within normal
ranges, with the exception of β-HCG and carbohydrate antigen 125,
which were elevated (3,171 IU/l and 96.7 U/ml, respectively). At
this point, the patient was transferred to the Department of
Gynecology for the continuation of treatment, due to the
consideration of a diagnosis of choriocarcinoma. Speculum
examination revealed a closed cervix. The uterus was observed to be
anteverted and reduced in size, and the bilateral adnexal region
was normal. A transvaginal ultrasound demonstrated no
abnormalities. A chest CT revealed multiple metastases in the right
upper lobe of the lung, scapula and atlantoaxial joint (Figs. 1–3),
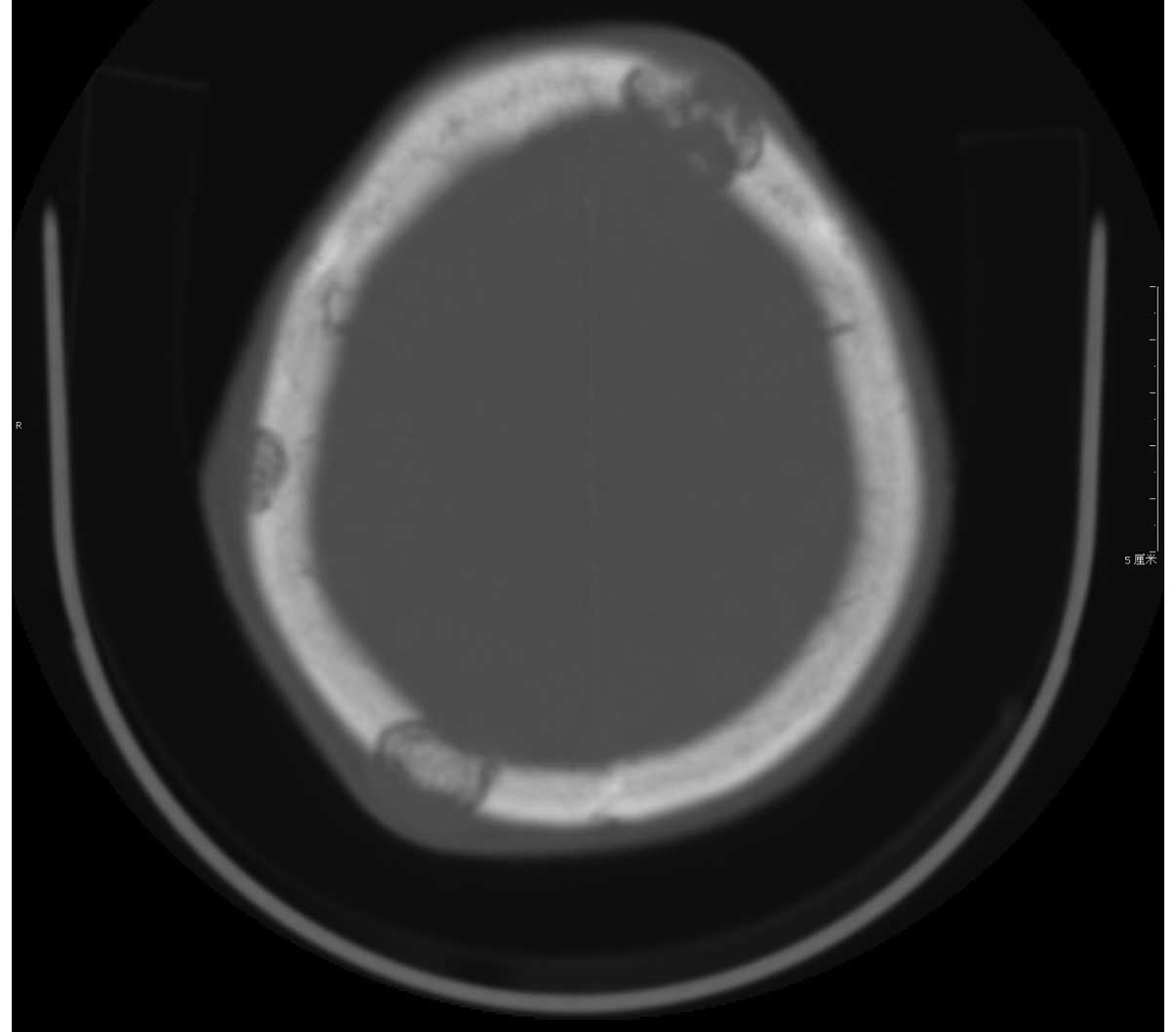
while a CT of the abdomen revealed no abnormalities. A head CT
revealed multiple metastases in the skull, neck and lymph nodes
(Fig. 4). Ultrasound examination of
masses in the scalp and abdomen revealed destruction of the cranial
plate and a hypoechoic mass located in the left flank muscles,
respectively. The patient was assigned FIGO stage IV and a WHO
score of 13, indicating high risk and poor prognosis (4). Typically, a patient with this diagnosis
would be treated with etoposide, methotrexate, actinomycin D,
cyclophosphamide and vincristine (EMA-CO) chemotherapy (5), however as the patient was in a poor
general condition, alternative systemic chemotherapy, comprising
tegafur (800 mg) and actinomycin D (200 µg), was administered.
During the process of chemotherapy, the patient exhibited itchy
skin, a red maculopapular rash, fever and other symptoms. Due to
these significant side-effects, systemic chemotherapy was halted on
day 4. Antibiotics (0.2 g cefotaxime, every 12 h)were administered
for 5 days to prevent infection, and the scalp and left flank
masses were first injected with methotrexate (20 mg), followed by
injection with 5-fluorouracil (250 mg). During chemotherapy, β-HGG
levels decreased from 3,171 IU/l to 1,763 IU/l. Following remission
of the side-effects, the patient completed the last course for four
days. However, at the conclusion of the courses of systemic and
local chemotherapy, β-HCG levels had increased to 3,704 IU/l.
Laboratory tests indicated that hemoglobin levels, platelet numbers
and C-reactive protein levels were 59 g/l, 59×109/l and
86.4 g/l, respectively. The patient and their family elected to end
treatment. Subsequently, the patient succumbed to infection six
months after initial admission, due to tumor consumption and organ
insufficiency.
Discussion
Choriocarcinoma is a highly malignant tumor that is
classified among the gestational trophoblastic diseases (1). Choriocarcinoma is typically present
within a hydatiform mole, and primarily occurs during the fertile
period. Choriocarcinoma incidence is rare following menopause
(1). Trophoblastic cells possess an
affinity for blood vessels; therefore trophoblastic tumors exhibit
a tendency to metastasize via the hematogenous route (6). In the present report, a particularly
rare case of neoplasm, which developed 20 years subsequently to the
onset of menopause and 42 years following the patient's final
pregnancy, was outlined.
Choriocarcinomas are aggressive malignancies, which
may be separated into two groups: Non-gestational choriocarcinoma
(NGCO), which typically arises from the gonadal organs, but may
also occur in extragonadal primary sites; and gestational
choriocarcinoma (GCO), which is derived from any form of previously
normal or abnormal pregnancy, such as a hydatidiform mole,
spontaneous abortion or ectopic pregnancy (7). Due to its poorer prognosis, NGCO
requires more aggressive therapy with numerous chemotherapeutic
agents (8), and may also require
surgical treatment. DNA analysis is a reliable method for
distinguishing between the two categories (8). Exman et al (9) hypothesized that polymorphic analysis of
tumor DNA was necessary for diagnosis. Rare cases of NGCO have also
been reported at multiple locations, including the ovaries
(9), lungs (10), urinary bladder (11), stomach (12) and vulva (13). The current patient presented with
extra-uterine choriocarcinoma, and the primary symptoms exhibited
were pulmonary lesions, bone metastases and skin masses. The
patient was not eligible for surgical treatment of the tumors due
to poor general condition, so it could not be confirmed whether the
patient exhibited NGCO or GCO with multiple lung, skull, neck,
lymph node and skin metastases. The most common sites for
choriocarcinoma metastases are the lungs and vulvovaginal region,
followed by the brain and liver (14). Alternative sites of metastasis,
including the skin, gastrointestinal tract, kidney, breast and
bone, are rarely observed (15).
A total of 75% of FIGO stage IV choriocarcinoma
patients are expected to achieve complete or prolonged remission
when treated with multiagent chemotherapy regimens, including MAC
(methotrexate, actinomycin-D and cyclophosphamide) and CHAMOCA
(cyclophosphamide, hydroxycarbamide, doxorubicin, actinomycin D,
methotrexate, melphalan and vincristine) (16). Currently, the most commonly used
alternatives to the aforementioned multiagent chemotherapy regimens
are EMA-CO or fluorouracil-based chemotherapy regimens. Due to the
poor condition of the current patient, systemic chemotherapy with
tegafur and actinomycin D was administered, and the scalp and left
flank masses were directly injected with methotrexate and
5-fluorouracil. The patient and their family subsequently elected
to end treatment, and the patient succumbed to the disease.
In conclusion, the current case presented unusual
findings with regard to choriocarcinoma, and thus, differentiating
between primary tumors of the lungs or other organs and metastases,
and choriocarcinoma was difficult. This study indicates that in
cases where one isolated lesion in the lung, bone or other organ is
identified in a postmenopausal female, the possibility of
choriocarcinoma must be considered. Subsequently, combination
chemotherapy may be administered with curative intent or with the
aim of prolonging life or to palliate symptoms. However, in certain
cases conservative NGCO therapy may be insufficient and thus,
surgical excision may be required.
References
|
1
|
Morrow CP, Kletzky OA, Disaia PJ, Townsend
DE, Mishell DR and Nakamura RM: Clinical and laboratory correlates
of molar pregnancy and trophoblastic disease. Am J Obstet Gynecol.
128:424–430. 1977.PubMed/NCBI
|
|
2
|
Lee JH, Park CW, Chung DH and Kim WK: A
case of lumbar metastasis of choriocarcinoma masquerading as an
extraosseous extension of vertebral hemangioma. J Korean Neurosurg
Soc. 47:143–147. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Cole LA, Khanlian SA, Muller CY, Giddings
A, Kohorn E and Berkowitz R: Gestational trophoblastic disease: 3.
Human chorionic gonadotrophin-free beta-subunit, reliable marker of
placental site trophoblastic tumors. Gynecol Oncol. 102:160–164.
2006. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Sierra-Bergua B, Sánchez-Marteles M,
Cabrerizo-García JL and Sanjoaquin-Conde I: Choriocarcinoma with
pulmonary and cerebral metastases. Singapore Med J. 49:e286–e288.
2008.PubMed/NCBI
|
|
5
|
El-Helw LM and Hancock BW: Treatment of
metastatic gestational trophoblastic neoplasia. Lancet Oncol.
8:715–724. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Morgan JM and Lurain JR: Gestational
trophoblastic neoplasia: An update. Curr Oncol Rep. 10:497–504.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Guo J, Zhong C, Liu Q, Xu J, Zheng Y, Xu
S, Gao Y, Guo Y, Wang Y, Luo Q and Jiang J: Intracranial
choriocarcinoma occurrence in males: Two cases and a review of the
literature. Oncol Lett. 6:1329–1332. 2013.PubMed/NCBI
|
|
8
|
Jacobs AJ, Newland JR and Green RK: Pure
choriocarcinoma of the ovary. Obstet Gynecol Surv. 37:603–609.
1982. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Exman P, Takahashi TK, Gattás GF,
Cantagalli VD, Anton C, Nalesso F and Diz Mdel P: Primary ovary
choriocarcinoma: Individual DNA polymorphic analysis as a strategy
to confirm diagnosis and treatment. Rare Tumors. 5:89–92. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Di Crescenzo V, Laperuta P, Napolitano F,
Carlomagno C, Garzi A and Vitale M: An unusual case of primary
choriocarcinoma of the lung. BMC Surg. 13(Suppl 2): S332013.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Gallagher L, Lind R and Oyasu R: Primary
choriocarcinoma of the urinary bladder in association with
undifferentiated carcinoma. Hum Pathol. 15:793–795. 1984.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Matsunaga N, Hayashi K, Futagawa S, Fukuda
T, Takahara O, Yoshida K and Maeda H: Primary choriocarcinoma of
the stomach presenting as gastrointestinal hemorrhage: Report of a
case. Radiat Med. 7:220–222. 1989.PubMed/NCBI
|
|
13
|
Weiss S, Amit A, Schwartz MR and Kaplan
AL: Primary choriocarcinoma of the vulva. Int J Gynecol Cancer.
11:251–254. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Milenković V, Lazović B, Mačvanski M,
Jeremić K and Hrgović Z: Clinical outcome of a FIGO stage IV
gestational choriocarcinoma. Case Rep Oncol. 6:504–507. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Singh S, Sardhana M, Sharma S and
Chitralkar P: Choriocarcinoma presenting as an isolated bone marrow
metastasis - a case report. Ecancermedicalscience.
8:3932014.PubMed/NCBI
|
|
16
|
FIGO Committee on Gynecologic Oncology:
Current FIGO staging for cancer of the vagina, fallopian tube,
ovary, and gestational trophoblastic neoplasia. Int J Gynaecol
Obstet. 105:3–4. 2009. View Article : Google Scholar : PubMed/NCBI
|