Introduction
Osteosarcoma is the most common type of primary bone
malignancy with an incidence rate of 4–5% in the USA (1). It most commonly occurs in the femur
(42%), then the tibia (19%), the humerus (10%), the skull or jaw
(8%), the pelvis (8%), and the ribs (1.25%). Osteosarcomas are
classified into various subtypes, according to certain
characteristics: Intramedullary, cortical, periosteal and parosteal
osteosarcoma, according to tumor location; well differentiated or
poorly differentiated according to tumor differentiation;
osteoblastic, chondroblastic, fibroblastic, telangiectatic and
small cell osteosarcoma, according to cell type; and single or
multiple, according to tumor number (2). The global incidence of secondary
osteosarcoma is <1% and surgery is the treatment of choice for
this tumor. Patients often exhibit local pain at metastatic sites
and symptoms associated with primary disease. Limb salvage surgery
may be performed to relieve symptoms of secondary osteosarcoma and
to prevent local recurrence (3).
Surgery and chemotherapy are used to treat osteosarcoma patients
without metastasis. However, additional radiotherapy is not
recommended for patients without metastasis due to the risk of
radiation-induced necrosis of surrounding structures (4). As 80% of osteosarcoma patients exhibit
metastatic disease at diagnosis, the majority are treated with
multi-agent chemotherapy in addition to surgical resection. As
expected, patients who present with metastases have a worse
prognosis and the 5-year survival rate of these patients is only
20–40% (3). The aim of the present
study was to increase knowledge with regard to osteosarcoma and to
discuss the clinical presentation, diagnosis, treatment and
prognosis of the disease.
Case report
A 53-year-old female was admitted to the Department
of Orthopedics, The First Affiliated Hospital of Soochow University
(Suzhou, Jiangsu, China) with increasing pain in the right knee
that had been present for 1 month on February 10, 2014. The patient
had undergone a lower right femoral tumor resection and knee joint
arthrodesis 20 years previously. The patient then received
chemotherapy, which consisted of 4.0 g methotrexate (MTX) and 2.0
mg vincristine (VCR) three times every 2 weeks. The post-operative
pathological results showed a fibrosarcoma with muscle and bone
destruction. Additional chemotherapy (4.0 g MTX and 2.0 mg VCR) was
performed post-operatively. On January 29, 1996, a local lesion
resection was performed due to recurrence. The post-operative
pathological results confirmed this diagnosis, and the patient
subsequently received post-operative chemotherapy (4.0 g MTX and
2.0 mg VCR). The patient also received high-dose radiotherapy, with
daily doses of radiation of up to 65 Gy lasting for 5 weeks. On
November 25, 1996, a local resection of the lesion was again
performed due to recurrence. To complicate matters, the patient
also suffered from more than one type of cancer. The patient also
underwent surgery due to thyroid papillary carcinoma in 1991.
Physical examination showed that there was tenderness and
percussion pain on the right knee, and the skin temperature was
slightly higher than normal. The movement of the right knee joint
was lost.
Upon the current admission, several diagnostic
techniques were used, including a blood routine test, a urine
routine test, a stool routine test, analysis of the erythrocyte
sedimentation rate, C-reactive protein level and serum
procalcitonin level, and an electrocardiogram, chest X-ray, and
thyroid and inguinal lymph node ultrasound. The results showed an
elevated alkaline phosphatase level of 192.0 U/l (normal range,
50–135 U/l). Pre-operative X-ray showed that there was a
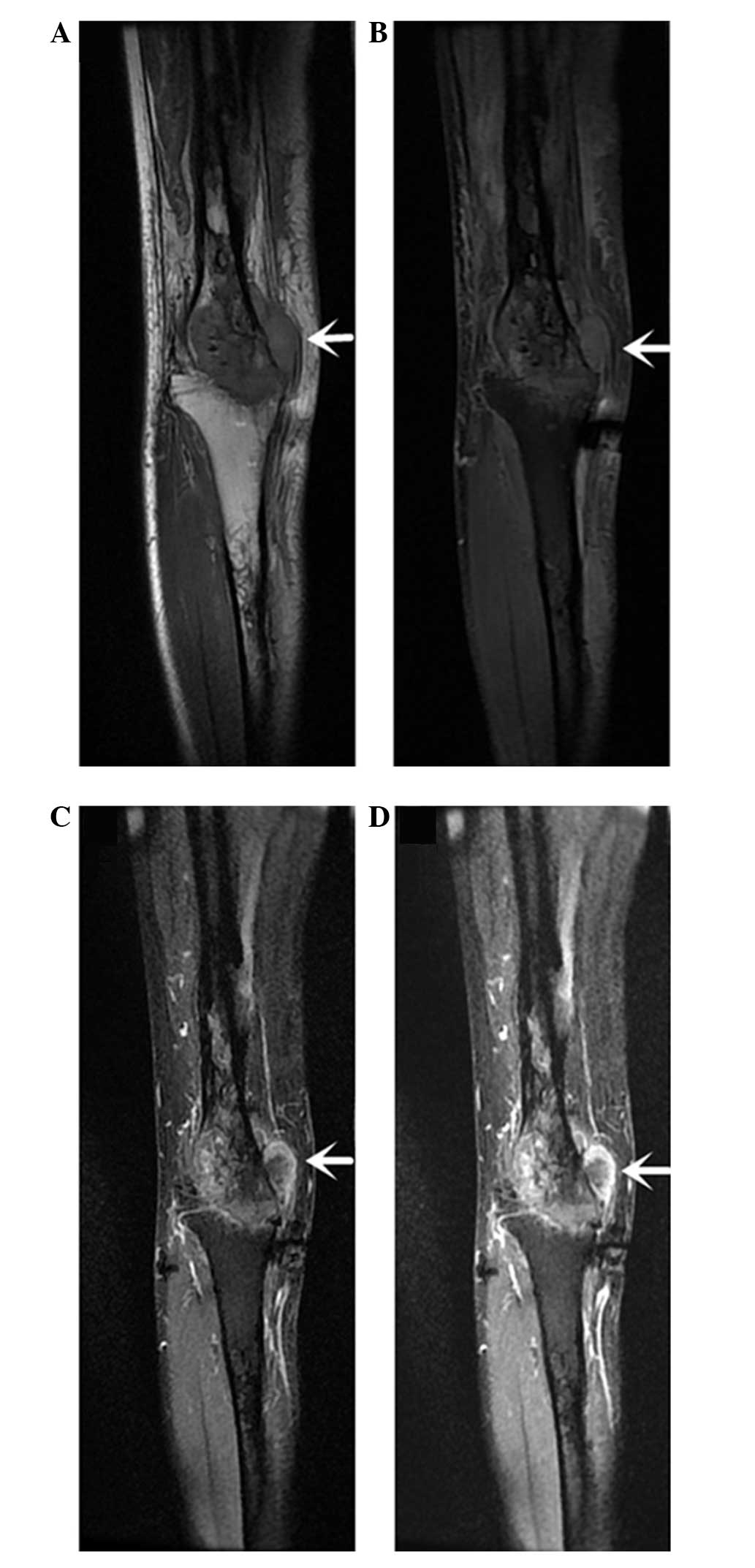
soft-tissue shadow at the medial side of the distal femur (Fig. 1). Magnetic resonance imaging (MRI)
showed the mass with a high signal intensity on diffusion-weighted
imaging (Fig. 2), a medium to low
signal intensity on T1-weighted imaging (Fig. 3A), high signal intensity on
T2-weighted imaging (Fig. 3B), high
signal intensity on short time inversion recovery imaging (Fig. 3C), unequal enhancement (Fig. 3D). Furthermore, the results of a
computed tomography-guided puncture biopsy were suspicious of
chondroblastic osteosarcoma.
On March 5, 2014, the patient underwent a thigh
amputation through the right femur. The texture of the resected
tumor was relatively soft with a scarlet color. Furthermore, the
tumor had an irregular shape and measured 1.5×1×3cm3.
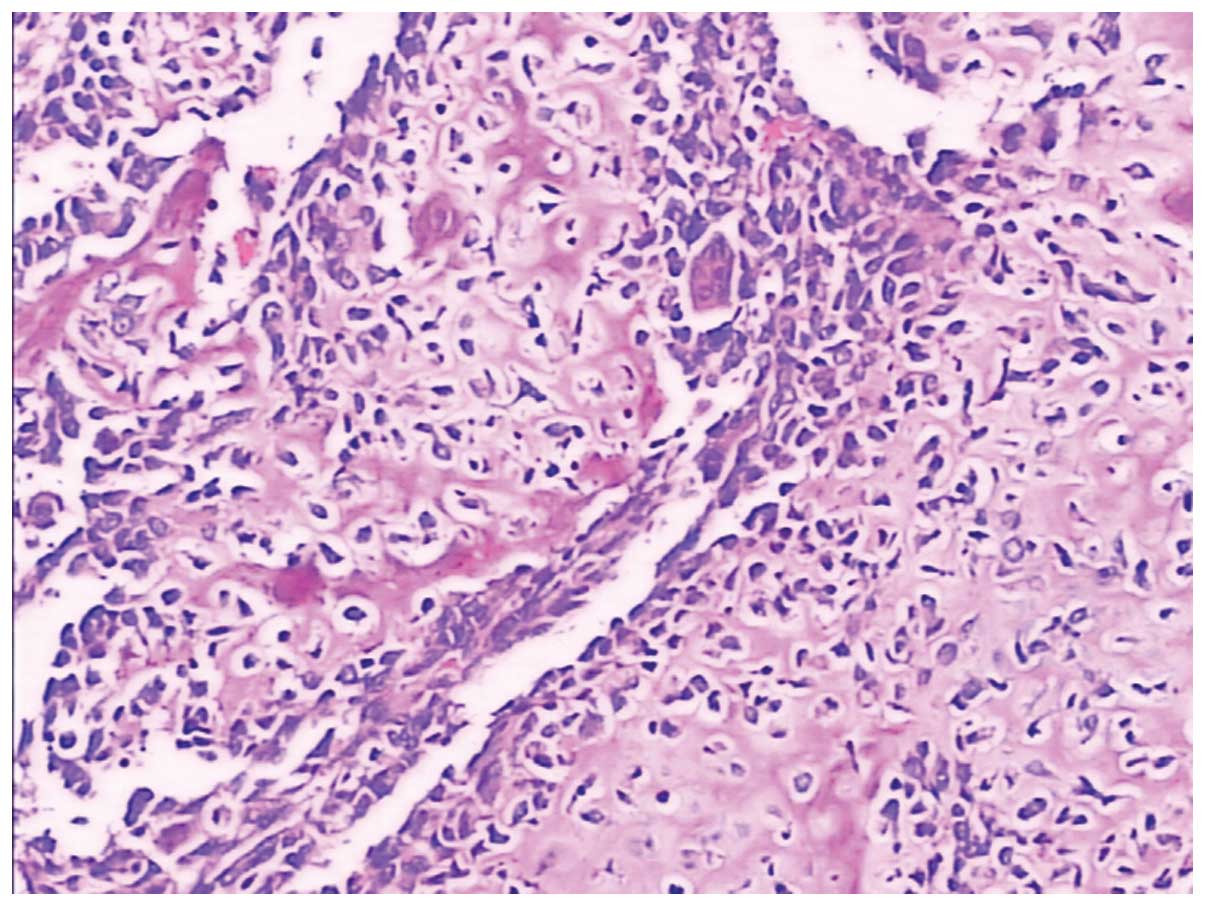
The final pathological examination confirmed the diagnosis of a
chondroblastic osteosarcoma without involvement of the para-tumor
tissues (Fig. 4). Following the
surgery, the patient received anti-infection (2.0 g cefonicid
sodium) and fluid therapy for 3 days. The patient recovered well,
and could walk slowly with a crutch ~3 weeks after surgery. The
patient's condition was discussed with oncologists and
subsequently, the patient was administered chemotherapy with
methotrexate (4.0 g) and vincristine (2.0 mg) once, 3 weeks after
surgery. In addition, it was recommended that long-term follow-up
was continued. Follow-up performed in April 2015 revealed that the
patient was well, however the patient subsequently developed lung
metastases and refused further treatment. On June 28, 2015, the
patient succumbed to the disease due to lung metastasis.
Discussion
Osteosarcoma, the most common primary malignant
tumor that can develop in the bones, can be classified into a
number of sub-types, although there is no uniform standard of
classification. Previous studies have divided this lesion based on
its position, degree of differentiation and components.
Osteosarcoma has a well-recognized double peak of incidence, with
peak one in children aged 10–14 years, coinciding with the pubertal
growth spurt, and peak two in adults aged >65 years, which is
more likely to be attributed to previous radiotherapy or Paget's
disease (4).
In recent years, associated studies have reported
that primary osteosarcoma still accounts for the vast majority of
primary bone malignancies, while the incidence of secondary
osteosarcoma is <1%. In the present study, a rare case of
chondroblastic osteosarcoma secondary to fibrosarcoma is reported.
The patient was relatively young and suffered from more than one
type of cancer. The course of the disease lasted for >20
years.
The aims of modern orthopedic oncology are an
optimal tumor resection and a resultant functional residual limb,
with increased patient survival (5).
With the improvement of technology and treatments, particularly
chemotherapy, the opportunity to perform limb salvage has been
increased to include 80% of patients, with an increase in
disease-free survival rate from <20% prior to the use of
effective chemotherapy to 55–75% following this (6). The advantages and disadvantages of a
marginal resection or amputation were therefore carefully analyzed
in the present study. In consideration of the gradually improving
prostheses and the possibility of local recurrence, an amputation
was finally selected. In the view Goorin et al, there is no
advantage in event-free survival for patients administered with
neoadjuvant chemotherapy (7).
However, neoadjuvant chemotherapy can improve the safety of limb
salvage (8). The medullary scope of
osteosarcoma invasion diagnosed by MRI has clear advantages and has
become the main method for determining a reasonable resection plane
of bone (9).
Through a review of the pertinent literature, stage
can be observed to be the most significant predictive factor,
followed by tumor volume, old age, gender and possibly
p-glycoprotein expression (10–16). In
addition, The present study the response to chemotherapy is the
only proven independent factor for the prediction of survival
(17). Therefore, after the surgery
in the present case, individual chemotherapy and multimodality
therapy was performed, as this has been shown to increase the
survival rate when compared with surgery alone (18). It is noteworthy that the best time for
resuming chemotherapy is within 21 days of definitive surgery. All
doctors and patients are required to work together to ensure that
chemotherapy is resumed in a timely manner following surgery
(19). Osteosarcoma is not sensitive
to radiotherapy. For an intralesional surgical margin or where
excision is not possible, additional radiotherapy has a positive
effect on the prognosis (20). The
study by Nakase et al suggested that p-53 gene therapy via
cationic liposome modification with transferrin is an effective
strategy for the treatment of osteosarcoma. However, further
research is required to improve the clinical efficacy (21). Immunotherapy has great potential for
treating osteosarcomas, promising improved patient survival rates
and quality of life (22).
The current study presents a rare case of
osteosarcoma secondary to fibrosarcoma. According to the previous
literature, and clinical and radiological findings, this patient
could be diagnosed with chondroblastic osteosarcoma. In contrast to
other studies, this case is quite rare due to the age of the
patient, the fact that the patient suffered from more than one type
of cancer and the disease course of >20 years. The current study
indicates that when a patient with a history of tumor develops
clinical symptoms, such as local pain, clinicians should pay
attention as this may be an indicator of recurrence or metastasis.
Furthermore, the present study indicates that a marginal resection
may be a good choice for treating fibrosarcoma. However, when the
histopathological result is confirmed as osteosarcoma, amputation
may be the better choice of treatment.
Acknowledgements
This study was supported by the Jiangsu Provincial
Special Program of Medical Science (grant no. BL2012004), the
Jiangsu Provincial Clinical Orthopedic Center and the Priority
Academic Program Development of Jiangsu Higher Education
Institutions.
References
|
1
|
Damron TA, Ward WG and Stewart A:
Osteosarcoma, chondrosarcoma, and Ewing's sarcoma: National Cancer
Data Base Report. Clin Orthop Relat Res. 459:40–47. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Canale ST and Beaty JH: Campbell's
Operative Orthopaedics (12th). Philadelphia, PA: Elsevier. 2013.
View Article : Google Scholar
|
|
3
|
Briccoli A, Rocca M, Salone M, Guzzardella
GA, Balladelli A and Bacci G: High grade osteosarcoma of the
extremities metastatic to the lung: long-term results in 323
patients treated combining surgery and chemotherapy, 1985–2005.
Surg Oncol. 19:193–199. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ottaviani G and Jaffe N: The epidemiology
of osteosarcoma. Cancer Treat Res. 152:3–13. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Marulanda GA, Henderson ER, Johnson DA,
Letson GD and Cheong D: Orthopedic surgery options for the
treatment of primary osteosarcoma. Cancer Control. 15:13–20.
2008.PubMed/NCBI
|
|
6
|
Jaffe N: Osteosarcoma: Review of the past,
impact on the future. The American experience. Cancer Treat Res.
152:239–262. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Goorin AM, Schwartzentruber DJ, Devidas M,
et al: Presurgical chemotherapy compared with immediate surgery and
adjuvant chemotherapy for nonmetastatic osteosarcoma: Pediatric
oncology group study POG-8651. J Clin Oncol. 21:1574–1580. 2003.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Arpaci F, Ataergin S, Ozet A, et al: The
feasibility of neoadjuvant high-dose chemotherapy and autologous
peripheral blood stem cell transplantation in patients with
nonmetastatic high grade localized osteosarcoma: Results of a phase
II study. Cancer. 104:1058–1065. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Bacci G, Forni C, Longhi A, Ferrari S,
Mercuri M, Bertoni F, Serra M, Briccoli A, Balladelli A and Picci
P: Local recurrence and local control of non-metastatic
osteosarcoma of the extremities: A 27-year experience in a single
institution. J Surg Oncol. 96:118–123. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bramer JA, Van Linge JH, Grimer RJ and
Scholten RJ: Prognostic factors in localized extremity
osteosarcoma: A systematic review. Eur J Surg Oncol. 35:1030–1036.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Clark JC, Dass CR and Choong PF: A review
of clinical and molecular prognostic factors in osteosarcoma. J
Cancer Res Clin Oncol. 134:281–297. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Bacci G, Longhi A, Versari M, Mercuri M,
Briccoli A and Picci P: Prognostic factors for osteosarcoma of the
extremity treated with neoadjuvant chemotherapy 15-year experience
in 789 patients treated at a single institution. Cancer.
106:1154–1161. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Bielack SS, Kempf-Bielack B, Delling G,
Exner GU, Flege S, Helmke K, Kotz R, Salzer-Kuntschik M, Werner M,
Winkelmann W, et al: Prognostic factors in high-grade osteosarcoma
of the extremities or trunk: An analysis of 1,702 patients treated
on neoadjuvant cooperative osteosarcoma study group protocols. J
Clin Oncol. 20:776–790. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Harting MT, Lally KP, Andrassy RJ,
Vaporciyan AA, Cox CS Jr, Hayes-Jordan A and Blakely ML: Age as a
prognostic factor for patients with osteosarcoma: An analysis of
438 patients. J Cancer Res Clin Oncol. 136:561–570. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Shalaby S, Shalaby H and Bassiony A: Limb
salvage for osteosarcoma of the distal tibia with resection
arthrodesis, autogenous fibular graft and llizarov external
fixator. J Bone Joint Surg Br. 88:1642–1646. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Smeland S, Müller C, Alvegard TA, Wiklund
T, Wiebe T, Björk O, Stenwig AE, Willén H, Holmström T, Follerås G,
et al: Scandinavian sarcoma group osteosarcoma study SSG VIII:
prognostic factors for out-come and the role of replacement salvage
chemotherapy for poor histological responders. Eur J Cancer.
39:488–494. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Davis AM, Bell RS and Goodwin PJ:
Prognostic factors in osteosarcoma: A critical review. J Clin
Oncol. 12:423–431. 1994.PubMed/NCBI
|
|
18
|
Manoso MW, Healey JH, Boland PJ,
Athanasian EA, Maki RG, Huvos AG and Morris CD: De novo osteogenic
sarcoma in patients older than forty: Benefit of multimodality
therapy. Clin Orthop Relat Res. 438:110–115. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Imran H, Enders F, Krailo M, Sim F, Okuno
S, Hawkins D, Neglia J, Randall RL, Womer R, Mascarenhas L and
Arndt CA: Effect of time to resumption of chemotherapy after
definitive surgery on prognosis for non-metastatic osteosarcoma. J
Bone Joint Surg Am. 91:604–612. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Ozaki T, Flege S, Kevric M, Lindner N,
Maas R, Delling G, Schwarz R, von Hochstetter AR, Salzer-Kuntschik
M, Berdel WE, et al: Osteosarcoma of the pelvis: Experience of the
cooperative osteosarcoma study group. J Clin Oncol. 21:334–341.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Nakase M, Inui M, Okumura K, Kamei T,
Nakamura S and Tagawa T: P53 gene therapy of human osteosarcoma
using a transferrin-modified cationic liposome. Mol Cancer Ther.
4:625–631. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Mori K, Rédini F, Gouin F, Cherrier B and
Heymann D: Osteosarcoma: Current status of immunotherapy and future
trends (Review). Oncol Rep. 15:693–700. 2006.PubMed/NCBI
|