Introduction
Mesonephric carcinoma of the uterine corpus is a
rare malignancy that originates from the mesonephric remnant of the
female reproductive tract (1). The
mesonephric duct, which parallels the paramesonephric duct during
the embryonic stage, forms the male epididymis, vas deferens,
seminal vesicles, partial prostate and urethra (2). Due to the lack of androgens, the
mesonephric duct degenerates in female embryos. The mesonephric
remnant in females is typically located in the ovary, broad
ligament and cervical sidewalls, although it may rarely be located
in the vaginal wall or myometrium (2). Due to the limited number of cases
reported of mesonephric carcinoma occurring within the myometrium,
there is limited information regarding the diagnosis and treatment
of this malignancy. In the present report, 2 cases of mesonephric
carcinoma diagnosed in the Tianjin Central Hospital of Gynecology
and Obstetrics (Tianjin, China) are presented.
Case report
Case 1
A 55-year-old female was admitted to the Tianjin
Central Hospital of Gynecology and Obstetrics (Tianjin, China) in
October 2013 for postmenopausal bleeding. The dilation and
curettage pathology report from another hospital revealed
poorly-differentiated endometrial adenocarcinoma with mucinous
degeneration and local mesenchymal dysplasia with sarcomatoid
carcinoma in the uterine cavity. Histological analysis of the
uterus by a pathologist at the Tianjin Central Hospital of
Gynecology and Obstetrics indicated a diagnosis of mesonephric
carcinoma. The patient had been diagnosed with diabetes mellitus 5
years earlier, according to the medical history. The physical
examination of the patient was normal, and the bimanual vaginal
examination indicated that the vulva, vagina and cervix were
normal, and the uterus was anteverted, large, mobile, bilateral,
and free of parametrial involvement. Pelvic ultrasonography
revealed a vesicle in the left ovary and a hypoechoic area in the
posterior uterine wall, although blood flow was not observed.
Pelvic magnetic resonance imaging revealed the presence of an
abnormally enhanced signal in the uterine cavity, hypervascular
lesions in the uterine corpus and isthmus and free fluid in the
pelvis. Regarding the analysis of tumour markers, the levels of
carbohydrate antigen (CA) 125, CA19-9 and α-fetoprotein (AFP) were
163.8 U/ml (normal, 0–35 U/ml), 193.6 U/ml (normal, 0–27 U/ml) and
16.8 ng/ml (normal, 0–7 ng/ml), respectively. In consequence,
extra-fascia hysterectomy, bilateral salpingo-oophorectomy and
pelvic lymphadenectomy were performed. The intraoperative findings
revealed ascites (~300 ml) and a large uterus. The bilateral
ovaries and oviducts, pelvic lymph nodes, liver, spleen and
diaphragmatic surface were all normal. A nodular mass of
3.5×2.0×2.5 cm in size was observed in the lower one-third of the
uterus and the cervix. The mass invaded the myometrium, and the
deepest part of the invasion almost reached the serous layer. The
microscopic analysis of the tumour resulted in a diagnosis of
mesonephric carcinoma with a sarcomatoid component, which involved
the cervical stroma and >50% of the uterine myometrium near the
serosa. No involvement of the bilateral ovaries and oviducts,
lymphovascular space, bilateral parametrium or pelvic lymph nodes,
was observed. On immunohistochemical analysis, the tumour specimen
was positive for cluster of differentiation (CD) 10, calretinin,
vimentin, cytokeratin (CK) and epithelial membrane antigen; and
negative for estrogen receptor (ER), progesterone receptor (PR),
CD99, and Wilms tumour-1. Furthermore, the ascites cytology was
positive, showing the presence of tumour cells. Therefore, the
postoperative diagnosis was mesonephric carcinoma. Chemotherapy,
consisting of paclitaxel (270 mg) on day 1, and cisplatin (20 mg)
and ifosfamide (2 g) on days 2–5, was subsequently administered to
the patient. After the first cycle of chemotherapy, the patient's
CA125 and CA19-9 levels had normalized to 31.02 U/ml and 25.24
U/ml, respectively. The second cycle of chemotherapy, comprising
paclitaxel and cisplatin, was modified due to severe
myelosuppression, resulting in the administration of 4 cycles of
paclitaxel (270 mg; day 1) and cisplatin (50 mg; days 2–3)
chemotherapy. Subsequent to treatment, the patient received regular
follow-up examinations. At 8 months post surgery, a pelvic
ultrasonogram revealed a hypoechoic mass in the pelvis of 58×36×33
mm in size. The patient's CA125 and CA19-9 levels had risen to
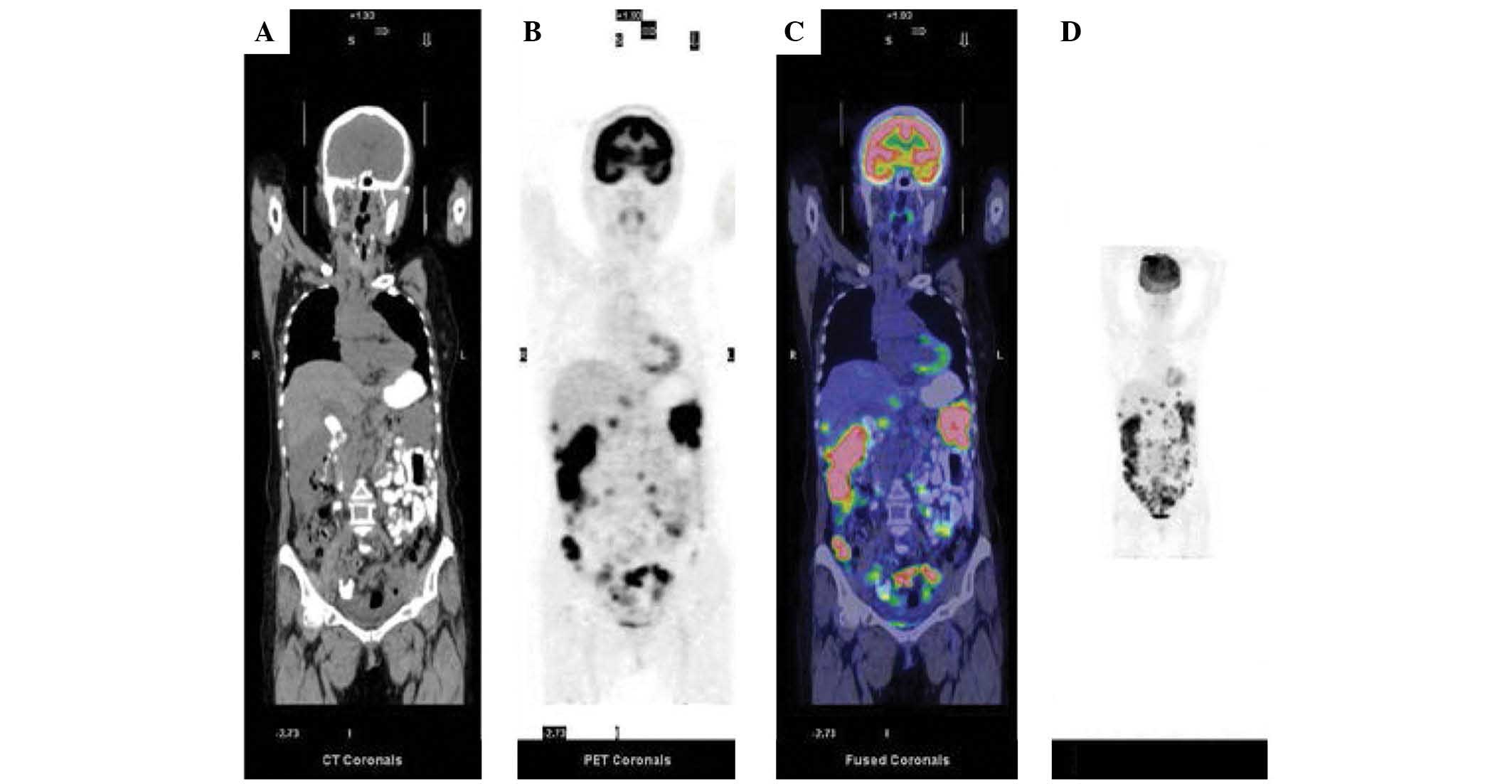
305.90 U/ml and 60.78 U/ml, respectively. Positron emission
tomography (PET)-computed tomography performed at the Tianjin
Medical University Cancer Institute and Hospital (Tianjin, China)
in April 2014 revealed possible metastasis to the mediastinal lymph
nodes, liver capsule, splenic capsule, liver falciform ligament,
hepatogastric ligament, lesser omentum, peritoneum, mesentery and
Douglas fossa (Fig. 1). Therefore, a
re-challenge chemotherapy regimen of pirarubicin (50 mg; day 1),
cisplatin (20 mg; days 2–5) and ifosfamide (2 g; days 2–5) was
subsequently administered. The patient succumbed to the disease in
April 2014, after an overall survival time of almost 12 months.
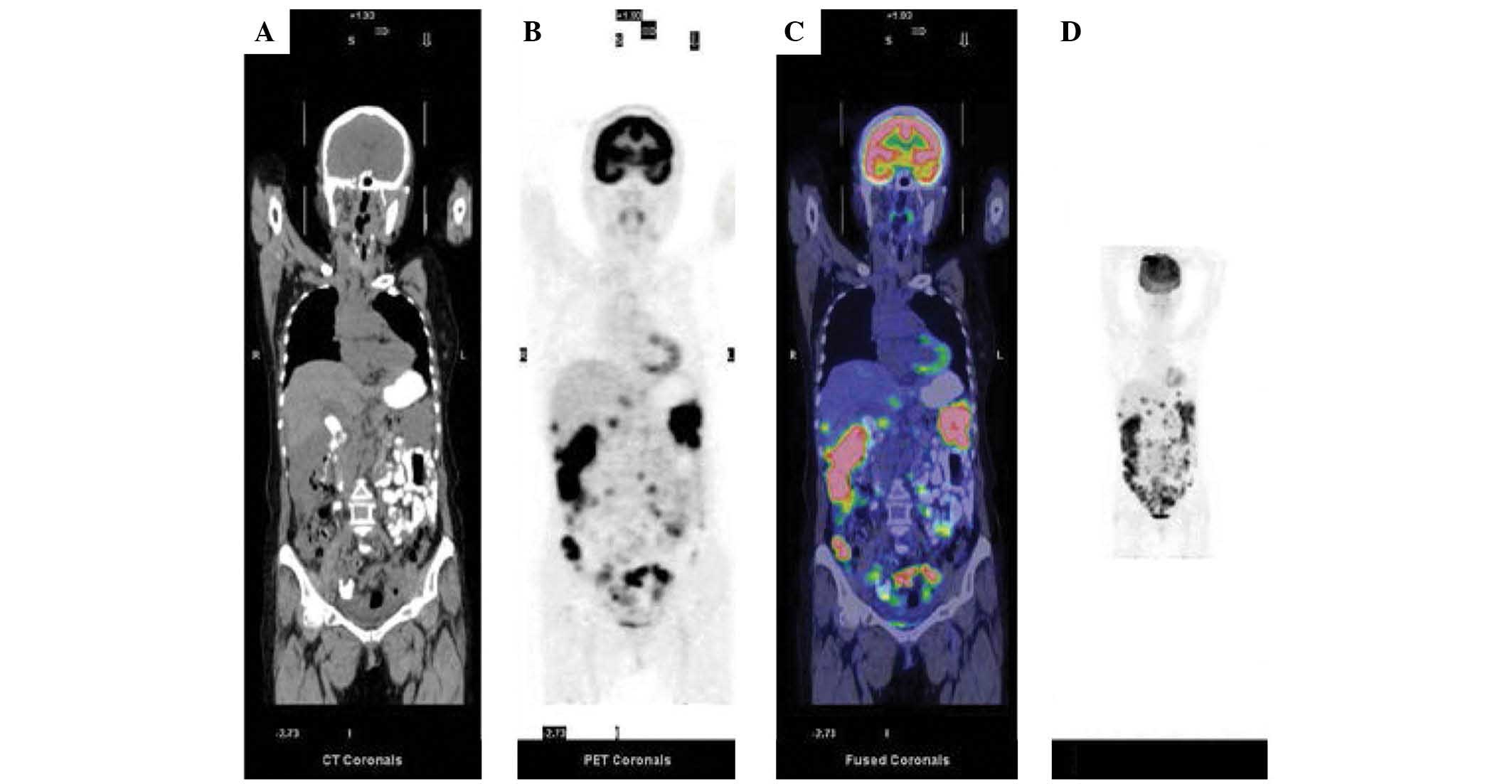 | Figure 1.Case 1: Whole body 18F-flutemetamol
contrast-enhanced PET/CT imaging following surgery. (A) Coronal CT
showing multiple lesions, (B) coronal PET imaging showing abnormal
radioactive accumulation and (C) coronal combined PET and CT
imaging showing enhanced 18F-flutemetamol uptake, in the abdomen
and pelvis, including the liver capsule, lesser omentum, splenic
capsule, peritoneummesentery, right paracolic sulci, the pouch of
Douglas and the pelvic peritoneum. (D) Maximum intensity projection
of PET/CT imaging showing metastatic lesions (black areas) in the
abdominal and pelvic cavity. PET, positron emission tomography; CT,
computed tomography. |
Case 2
A 62-year-old female was admitted to the Tianjin
Central Hospital of Gynecology and Obstetrics for postmenopausal
bleeding in April 2014. Based on the dilation and curettage
pathology report, a diagnosis of mesonephric carcinoma was
considered. The patient presented with a 20-year history of
hypertension. The physical examination was normal, and the bimanual
vaginal examination revealed that the vulva, vagina and cervix were
normal, and the uterus was anteverted, large, mobile, bilateral,
and free of parametrial involvement. An intrauterine mass of
58×38×37 mm in size was observed by pelvic ultrasonography, and
submucosal uterine fibroids were considered. Pelvic magnetic
resonance imaging revealed abnormal signal enhancement in the
uterine cavity, which was indicative of malignancy. In addition,
multiple small lymph nodes were observed around the iliac vessels
and in the groin. The levels of carcinoembryonic antigen were 10.52
ng/ml (normal, 0–7 ng/ml), while the levels of other tumour markers
were normal (CA125, 31.02 U/ml; CA19-9, 25.24 U/ml; AFP, 3.7
ng/ml). In consequence, extra-fascia hysterectomy, bilateral
salpingo-oophorectomy and pelvic lymphadenectomy were performed.
The intraoperative findings revealed mild bloody ascites and a
large uterus. The bilateral ovaries and oviducts, pelvic lymph
nodes, liver, spleen and diaphragmatic surface were all normal. The
pathological analysis resulted in a diagnosis of mesonephric
carcinoma of the uterine corpus with sarcomatoid components and no
lymphovascular involvement. On immunohistochemical analysis, the
tumour specimen was positive for CK, CK8/18, CD10, P16 and
vimentin, and negative for ER, PR, CD15, P53 and calretinin. In
addition, the tumour was partially positive for Ki-67 (<5% in
the epithelial area and 60% in the spindle cell sarcoma area). The
tumour involved the left internal iliac lymph node, but not the
bilateral ovaries, oviducts or parametrium. Tumour cells were not
detected in the ascites. Postoperatively, CEA levels returned to
normal values. The patient subsequently received chemoradiation
therapy with docetaxel (100 mg; day 1) and cisplatin (50 mg; days
2–3). The patient has shown no evidence of disease to date.
Discussion
Mesonephric carcinoma is a rare malignancy of the
female genital tract. Compared with mesonephric carcinoma of the
uterine corpus, cervical mesonephric carcinoma is more frequently
observed, with 27 of the 29 cases of mesonephric carcinoma reported
in the English literature occurring in the cervix, and 2 in the
corpus (2). In 2013, Meguro et
al (3) summarized 42 cases of
cervical mesonephric adenocarcinoma, including 10 cases with
sarcomatous components and 4 cases with exogenous or polypoid
tumours. At present, only 3 cases of uterine corpus mesonephric
carcinoma have been reported in the literature (Table I) (1,2,4). Furthermore, to the best of our
knowledge, no cases of mesonephric carcinoma accompanied by sarcoma
components have been reported thus far.
 | Table I.Clinical features of mesonephric
adenocarcinoma of uterine corpus from five cases. |
Table I.
Clinical features of mesonephric
adenocarcinoma of uterine corpus from five cases.
| Author
(reference) | Age, years | Symptoms | Ascites | FIGO stage | CA125 | Surgery | Additional
therapy | Outcome |
|---|
| Ordi et al
(4) | 33 | Lower abdominal pain;
hypermenorrhea | NA | Ic | NA | TAH + BSO + PLA | Carboplatin +
paclitaxel | Recurrence (10
months, intra-abdominal + lung); AWD, 3 months |
| Marquette et
al (2) | 81 | Postmenopausal
bleeding | NA | Ic | 55 U/ml | LAVH + BSO + OMT +
PLA | No | NED, 9 months |
| Wani et al
(1) | 73 | Multiple lung
nodules | NA | IV | Normal | TAH + BSO | Carboplatin +
paclitaxel | AWD, 28 months |
| Present study | 55 | Postmenopausal
bleeding | 300 ml; positive
cytology | II | 305.9 U/ml | TAH + BSO + PLA | Carboplatin +
paclitaxel + ifosfamide | Recurrence (8 months,
intra-abdominal + lymph node); overall survival, 12 months |
|
| 62 | Postmenopausal
bleeding | Mild bloody
ascites | IIIc1 | 12.91 U/ml | TAH + BSO + PLA | Docetaxel +
cisplatin; radiotherapy | NED, 16 months |
In the 3 previous cases of mesonephric carcinoma of
the uterine corpus, the ages of the patients at the time of
diagnosis were 33, 73 and 81 years, respectively (1,2,4). The symptoms at presentation included
abnormal vaginal bleeding, lower abdominal pain and presence of an
abdominal mass. As mesonephric carcinoma of the uterine corpus
originates from the mesonephric remnant in the myometrium, growth
of the tumour into the uterine cavity may cause abnormal vaginal
bleeding, as observed in these patients. A pelvic ultrasound may
reveal deformation of the uterus, presence of an intrauterine mass
or other pelvic abnormalities. However, in order to obtain a
definitive pathological diagnosis, tumour tissue must be obtained
through dilation and curettage or hysteroscopy. If the tumour grows
into the myometrium, an abdominal mass, abdominal pain, menorrhagia
and other symptoms may develop. Thus, it is not easy to
differentiate mesonephric carcinoma from adenomyosis; although a
pelvic ultrasound may reveal an enlarged uterus, the morphology of
the uterine cavity may be normal, and a hysteroscopic examination
may also be normal; and if the tumour tissue is lost then a
pathological diagnosis cannot be made. Mesonephric carcinoma of the
uterine corpus has been previously reported not to exhibit any
ultrasonographic manifestation. However, ultrasonographic
indications of mesonephric carcinoma in the appendages have been
previously reported in the literature, including a mixed mass in
the annex area (5). In addition,
blood vessels may or may not be displayed on Doppler imaging
(5). The 2 patients of the present
case report, who were aged 55 and 62 years old, respectively,
presented with the same symptom of postmenopausal bleeding. In the
first patient, ultrasonography indicated possible uterine fibroids;
however, no abnormal mass appeared within the uterine cavity, and
the uterine fibroids presented without vessel a signal. In the
second patient, ultrasonography suggested possible submucosal
fibroids. These findings indicate that there are certain
limitations to the diagnosis of mesonephric carcinoma by
ultrasonography alone.
The serum levels of CA125 have been reported to be
slightly increased in cases of mesonephric carcinoma of the uterine
corpus. However, serum CA125 is not a specific indicator of this
malignancy (2), as normal levels of
CA125 were observed in a previous case of mesonephric carcinoma of
the uterine corpus presenting with lung metastases (1). In the present case report, the levels of
CA125 were 163.8 U/ml in the first patient, and normal in the
second patient, indicating that serum CA125 is not a specific
marker for the diagnosis of corpus mesonephric carcinoma. Since
mesonephric carcinoma originates from the mesonephric remnant
present during the embryonic period, which is homologous with
differential tissue from the endoderm (1), we hypothesize that the levels of other
tumour markers such as AFP and carcinoembryonic antigen may also be
elevated in mesonephric carcinoma, due to homology. The patient of
the first case described in the present report experienced disease
recurrence, as indicated by her elevated levels of CA125.
Therefore, monitoring the levels of CA125 may be beneficial for
assessing possible recurrence in patients with mesonephric
carcinoma.
Due to the limited number of cases of uterine corpus
mesonephric carcinoma reported to date, no standard surgical
guidelines to treat this condition have been established thus far.
Since the tumours of the 2 patients of the present case report were
located in the uterine myometrium, the patients were accordingly
subjected to the same type of surgery that is usually performed to
treat endometrial cancer. This procedure differs from omentectomy,
which has been previously reported to be conducted on a patient
with corpus mesonephric carcinoma (2). Omentectomy remains a controversial
procedure for the treatment of corpus mesonephric carcinoma;
however, there has been one case report of a patient undergoing
this procedure (2). Although it is
considered that the omentum and the mesonephric remnant are
homologous in terms of embryology (2), if the tumor does not invade the serous
layer or if there is no omental involvement, then there is no
mesonephric remnant located in the omentum (1,4).
Therefore, removal of the omentum may not be required. In the first
patient of the present case report, the peritoneal ascites was
positive for malignancy, and the patient experienced postoperative
recurrence. Therefore, we believe that omentectomy should be
performed in those patients with positive peritoneal lavage.
On microscopic examination of the tumour tissue, a
small, tubular, mesh, solid, sex cord-like structure may be
observed in cases of mesonephric carcinoma (1,2,4). In addition, various cellular
morphologies may also coexist within the same tumour (1). In particular, a tubular luminal
epithelium and glandular cavity filled with eosinophilic material
may be observed. Previous immunohistochemical analyses have
revealed that tumour cells derived from mesonephric carcinoma are
generally positive for vimentin, calretinin, inhibin and CD10, and
tend to be negative for epithelial membrane antigen, ER, PR and
CK20 (1,4). In the first case of the present report,
the tumour specimen was positive for CD10, calretinin and vimentin,
and negative for ER and PR; whereas the tumour specimen for the
second case was positive for CD10 and vimentin, and negative for
calretinin, ER and PR. These results were similar to those
previously reported in the literature (4).
The most effective adjuvant chemotherapeutic regimen
for the treatment of mesonephric carcinoma remains unclear.
However, in previous reports, patients have been treated with
regimens that included paclitaxel and carboplatin (1,6). Among the
cases of mesonephric carcinoma previously reported in the
literature, 1 patient experienced local recurrence in the pelvis
and metastasis to the lung 10 months post-surgery; 1 patient who
presented lung metastases prior to surgery survived 28 months with
the disease; and 1 patient demonstrated no evidence of recurrence
within 9 months of follow-up (1,2). In
another report (3), a patient with
cervical mesonephric carcinoma with a sarcomatous component was
treated with radical hysterectomy, bilateral salpingo-oophorectomy
and pelvic lymph node dissection. The patient did not receive
postoperative adjuvant chemotherapy, and presented with disease
recurrence on the vaginal vault 7 months later. Subsequently,
radiotherapy and chemotherapy were concurrently administered to the
patient, and the recurrent tumour disappeared 3 months later.
Montagut et al (6) reported a
case of corpus mesonephric carcinoma treated with radical
hysterectomy, bilateral salpingo-oophorectomy, para-aortic lymph
node dissection and local postoperative radiotherapy, who developed
pelvic-abdominal recurrence and lung metastasis 10 months later.
Following 3 cycles of paclitaxel and carboplatin and surgical
removal of the lesion, the patient achieved partial remission, and
complete remission was achieved following 3 additional courses of
chemotherapy. The patient in the first case of the present report
experienced relapse 8 months post surgery, similar to the outcomes
of other patients with mesonephric carcinoma previously reported in
the literature (6); however, her
overall survival time was almost 12 months post surgery. The second
patient of the present case report, who presented with positive
pelvic lymph nodes, demonstrated no evidence of recurrence within
16 months of follow-up.
In conclusion, female genital mesonephric carcinoma
is a rare malignant tumour derived from embryonic mesonephric
remnants. According to the literature, mesonephric carcinoma occurs
more commonly in the cervix than in the uterus and vagina. The
clinical symptoms associated with mesonephric carcinoma are not
specific. In addition, imaging is unable to differentiate between
this malignancy and common female reproductive system tumours, and
no specific tumour markers for mesonephric carcinoma have been
identified thus far. Therefore, the surgical treatment and staging
of this malignancy may require to be based on the existent
guidelines for endometrial cancer. Furthermore, patients with
mesonephric carcinoma who exhibit risk factors should receive
appropriate postoperative treatments.
Acknowledgements
The authors wish to thank Editage (http://online.editage.cn/) for English language
editing, and the Department of Molecular Imaging and Nuclear
Medicine, Tianjin Medical University Cancer Institute and Hospital,
for providing PET images.
References
|
1
|
Wani Y, Notohara K and Tsukayama C:
Mesonephric adenocarcinoma of the uterine corpus: A case report and
review of the literature. Int J Gynecol Pathol. 27:346–352. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Marquette A, Moerman P, Vergote I and
Amant F: Second case of uterine mesonephric adenocarcinoma. Int J
Gynecol Cancer. 16:1450–1454. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Meguro S, Yasuda M, Shimizu M, Kurosaki A
and Fujiwara K: Mesonephric adenocarcinoma with a sarcomatous
component, a notable subtype of cervical carcinosarcoma: A case
report and review of the literature. Diagn Pathol. 8:74–78. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ordi J, Nogales FF, Palacin A, Márquez M,
Pahisa J, Vanrell JA and Cardesa A: Mesonephric adenocarcinoma of
the uterine corpus: CD10 expression as evidence of mesonephric
differentiation. Am J Surg Pathol. 25:1540–1545. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kuper SG, Wright DR, Callahan MJ and Hiett
AK: Ultrasound presentation of a female adnexal tumor of probable
wolffian origin (FATWO). J Diagn Med Sonogr. 29:282–284. 2013.
View Article : Google Scholar
|
|
6
|
Montagut C, Mármol M, Rey V, Ordi J,
Pahissa J, Rovirosa A, Gascón P and Mellado B: Activity of
chemotherapy with carboplatin plus paclitaxel in a recurrent
mesonephric adenocarcinoma of the uterine corpus. Gynecol Oncol.
90:458–461. 2003. View Article : Google Scholar : PubMed/NCBI
|