Introduction
Mantle cell lymphoma (MCL) is a non-Hodgkin's
lymphoma composed of small lymphoid cells. MCL usually occurs in
males with a median age of 60 years; however, its frequency
accounts for ~4% of all lymphomas in the Western countries
(1). It commonly involves the
gastrointestinal (GI) tract and may present as multiple
lymphomatous polyposis (MLP), which frequently occurs in the colon
and small bowel (2). However,
numerous sessile or polypoid lesions may be identified throughout
the GI tract (3).
Malignant lymphoma is an uncommon cause of
intussusception, which is estimated to cause <1% of all
intussusception cases (4). MLP
combined with intussusception is rare in MCL patients. Only a
limited number of MCL cases with intussusception have been
previously reported (5–7). The current study presented a case of GI
tract MCL with MLP and ileocecal intussusception that was
effectively treated with surgery and chemotherapy.
Case report
A 54-year-old male was referred to the Division of
Gastroenterology and Hepatology (Korea University College of
Medicine, Seoul, Korea) with abnormal computed tomography (CT)
findings in the right lower abdomen (June 2012). The patient had
been diagnosed with stage I bladder cancer 2 years earlier, and had
undergone transurethral resection of the bladder tumor and
intracavitary instillation of mitomycin. No evidence of bladder
cancer recurrence was observed during the 2 years of follow-up.
Upon referral to the Division of Gastroenterology and Hepatology,
intussusception and a mass in the terminal ileum were identified by
performing contrast-enhanced abdominal CT scans (Fig. 1). Physical examination revealed normal
vital signs and a soft distended abdomen with normoactive bowel
sounds. The initial laboratory findings were as follows: hemoglobin
level, 14.2 g/dl (normal range: 12.0–17.0 g/dl); white blood cell
count, 8,000/µl (normal range: 4,500–11,000/µl); platelet count,
171,000/µl (normal range: 150,000–400,000/µl); and C-reactive
protein level, 0.6 mg/dl (normal range: 0–5.0 mg/dl). Blood
biochemical analyses revealed no pathological findings, while the
β2-microglobulin and lactate dehydrogenase (LDH) levels
were normal. Written informed consent was obtained from the
patient.
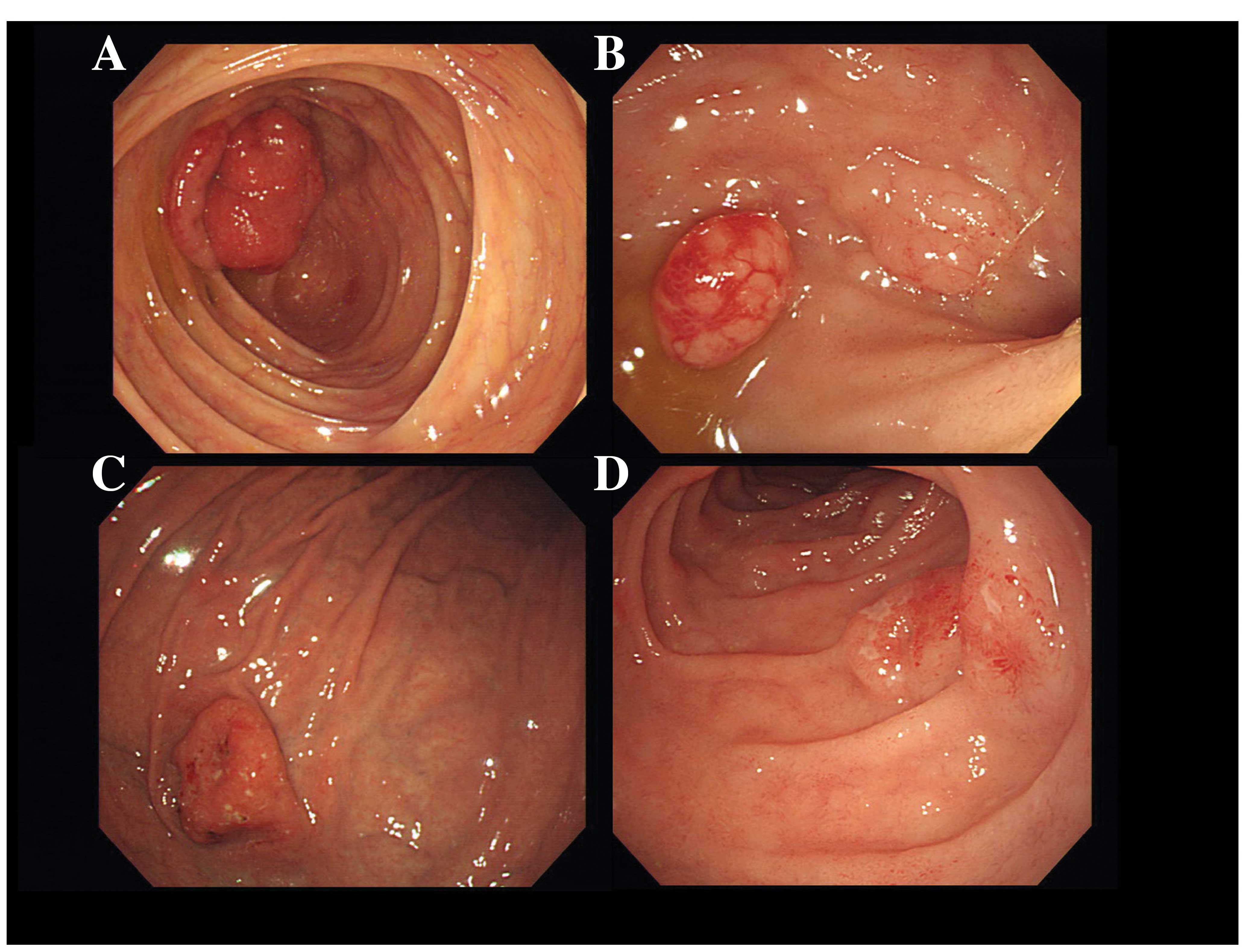
A total colonoscopy (CF-H260AL; Olympus Optical,
Tokyo, Japan) revealed ileocolic intussusception and a large mass
in the distal ileum (Fig. 2A). The
mass had a smooth rubber-like surface, fungating shape with
multilobular contour and a diameter of ~4–8 mm. Multiple round
nodules were also identified in the distal ileum (Fig. 2B) and rectum.
Esophagogastroduodenoscopy (GIF-H260; Olympus Optical) revealed a
polypoid tumor that measured ~30 mm in the high body of the stomach
(Fig. 2C) and multiple small
subepithelial nodular lesions from the bulb to the second portion
of the duodenum (Fig. 2D). Multiple
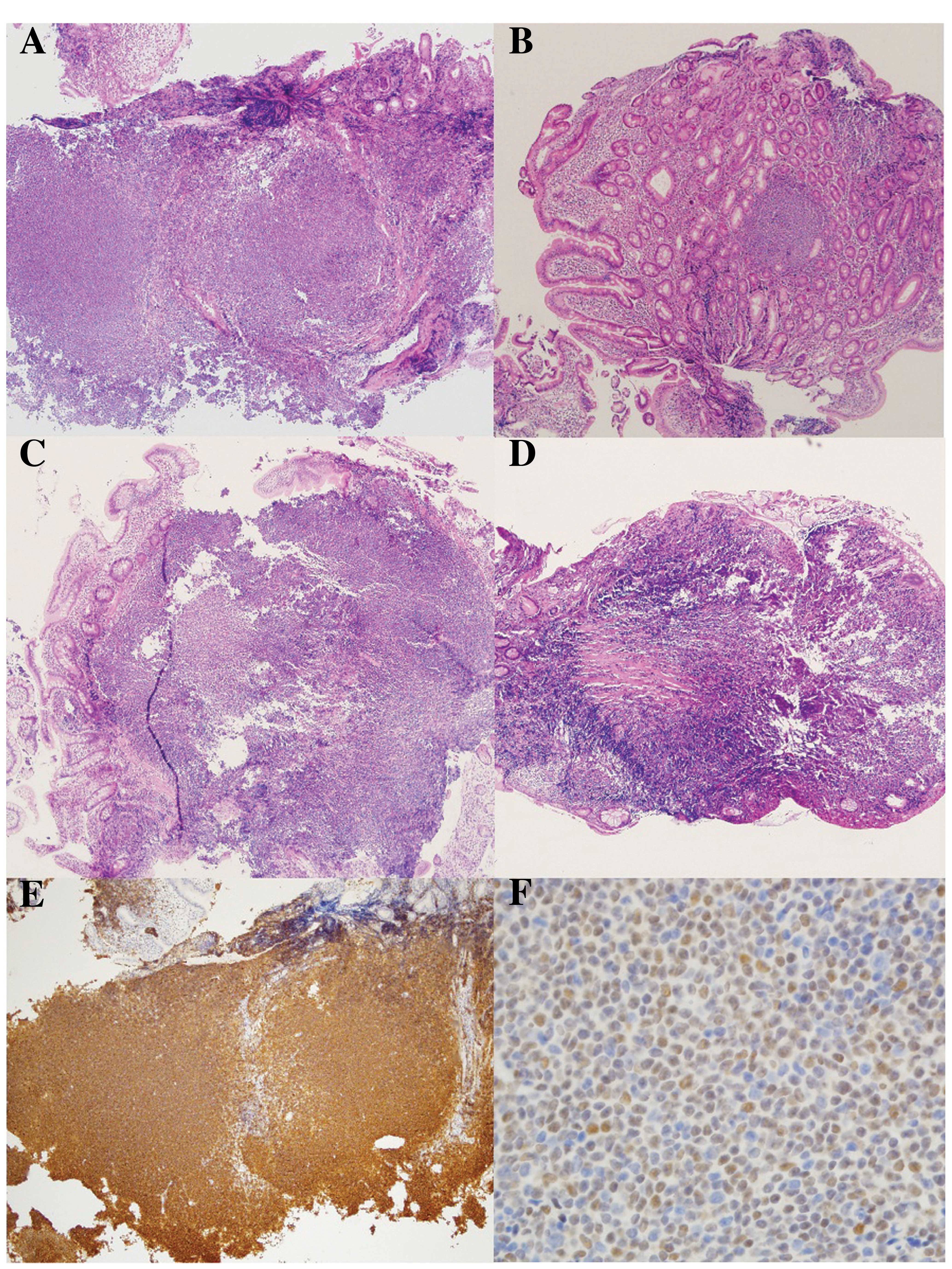
biopsies of the complete GI tract presented diffuse infiltration of
monotonous small-to-medium sized, lymphoid cells. In addition,
immunohistochemical analysis of the biopsy tissues demonstrated
positive staining for CD20, CD5, Bcl-2, CD43 and cyclin D1
(Fig. 3); therefore, the diagnosis
was confirmed to be MCL. A positron emission tomography (PET) scan
indicated intense hyper-metabolism of all digestive structures,
extending from the stomach to the rectal wall. Furthermore, a bone
marrow biopsy and chromosomal study were also performed; however,
no abnormal results were observed. The MCL International Prognostic
Index score (8) was 8.1, and the
disease was classified as stage IV according to the Ann Arbor
staging system (9).
The patient underwent right hemicolectomy with
distal ileum resection and ileocolic anastomosis (Fig. 4). After 20 days, chemotherapy with
rituximab plus hyper-CVAD (R-hyper-CVAD) was administered, with
alternating course A and B regimens for cycles during 6 months
[course A: Rituximab (375 mg/m2, intravenous, IV, day
1), cyclophosphamide (300 mg/m2, IV, day 2–4),
vincristine (1.4 mg/m2, IV, day 5 and 12), doxorubicin
(1.6 mg/m2, IV, day 5–7) and dexamethasone; course B:
Rituximab (375 mg/m2, IV, day 1), methotrexate (1,000
mg/m2, IV, day 2), leucovorin (15 mg every 6 h, IV, 10
times, day 3–5) and cytarabine (3 g/m2, every 6 h, IV,
day 3 and 4)]. Following 6 planned cycles of R-hyper-CVAD, upper
and lower endoscopic examinations demonstrated complete remission
and absence of polypoid lesions in the GI tract. The remission
lasted over 18 months and a follow-up PET scan revealed no abnormal
hypermetabolic lesions. There was no evidence of recurrence in
abdominal CT and endoscopic examination until the present time.
Discussion
MCL is a mature B-cell non-Hodgkin's lymphoma that,
according to previous epidemiological data, comprises up to 4% of
all lymphoma cases (1). Although
various studies have demonstrated improvement of the median
survival using aggressive chemotherapeutic strategies, the
prognosis of MCL remains unfavorable (10–13). MCL
generally occurs in adults with a median age of 60 years and has a
male predominance (14).
Overexpression of cyclin D1 is a typical characteristic of MCL.
MLP was initially defined by Cornes in 1961
(15). It involves numerous polypoid
lesions throughout the GI tract, caused by malignant lymphoma.
Diffuse and nodular polypoid lesions are a characteristic feature
at presentation; therefore, involvement of the GI tract must be
investigated by endoscopic examination in lymphoma patients. Common
clinical symptoms include abdominal pain, diarrhea and weight loss,
while protein-losing enteropathy, chylous ascites, intestinal
malabsorption and perforation are less frequently observed
(16). In rare cases, MCL with MLP
results in intestinal obstruction or intussusception. Several
previous studies have analyzed the clinical features and outcome of
MLP (16); however, no standardized
therapeutic options exist for GI cases of MCP with MLP.
Only a limited number of MCL cases presenting with
intussusception have been reported (5–7). In the
majority of cases, patients were treated with the R-CHOP
chemotherapy regimen (cyclophosphamide, doxorubicin, vincristine
and prednisone, in combination with rituximab) and surgical
resection. However, it has been suggested that the R-Hyper-CVAD
regimen (cyclophosphamide, vincristine, doxorubicin, dexamethasone,
cytarabine and methotrexate, in combination with rituximab) is
associated with improved response rates in MCL (17). The main concern in the present case
was the risk of remission failure or severe complications, such as
intestinal obstruction due to unresolved intussusception.
Therefore, prior to chemotherapy, the patient underwent right
hemicolectomy for tumor debulking and prevention of complications.
Subsequently, R-hyper-CVAD chemotherapy was administered.
In asymptomatic patients, it remains unclear whether
surgery prior chemotherapy is required and whether 6 cycles of
chemotherapy are appropriate to treat MCL with intussusception.
However, the therapeutic strategy in the present study demonstrated
marked results and good response. Progress in the current patient
suggested that complete remission may be achieved in MCL with MLP
following the administration of R-hyper-CVAD. In conclusion,
operative bowel resection may be a feasible option in MCL, when MLP
is associated with asymptomatic intussusception.
Acknowledgements
This study was supported by the Technology
Innovation Program (or Industrial Strategic technology development
program; grant no. 10049743), for establishing a medical device
development open platform, as a hub for accelerating close
firm-hospital communication) funded by the Ministry of Trade,
Industry and Energy (South Korea).
References
|
1
|
Schmidt C and Dreyling M: Therapy of
mantle cell lymphoma: Current standards and future strategies.
Hematol Oncol Clin North Am. 22:953–963. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim JH, Jung HW, Kang KJ, et al:
Endoscopic findings in mantle cell lymphoma with gastrointestinal
tract involvement. Acta Haematol. 127:129–134. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chung K, Tomowiak C, Yacoub M, et al: A
rare case of mantle cell lymphoma as lymphomatous polyposis with
widespread involvement of the digestive tract. Clin Res Hepatol
Gastroenterol. 35:74–78. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Chiang JM and Lin YS: Tumor spectrum of
adult intussusception. J Surg Oncol. 98:444–447. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kella VK, Constantine R, Parikh NS, et al:
Mantle cell lymphoma of the gastrointestinal tract presenting with
multiple intussusceptions-case report and review of literature.
World J Surg Oncol. 7:602009. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Grin A, Chetty R and Bailey D: Mantle cell
lymphoma as a rare cause of intussusception: A report of 2 cases.
Ann Diagn Pathol. 13:398–401. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Sucker C, Klima KM, Doelken G, et al:
Unusual sites of involvement in non-Hodgkin's lymphoma: Case 3.
Intussusception as a rare complication of mantle-cell lymphoma. J
Clin Oncol. 20:4397–4398. 2002.PubMed/NCBI
|
|
8
|
Carbone PP, Kaplan HS, Musshoff K, et al:
Report of the Committee on Hodgkin's disease staging
classification. Cancer Res. 31:1860–1861. 1971.PubMed/NCBI
|
|
9
|
Hoster E, Dreyling M, Klapper W, et al:
German Low Grade Lymphoma Study Group (GLSG); European Mantle Cell
Lymphoma Network: A new prognostic index (MIPI) for patients with
advanced stage mantle cell lymphoma. Blood. 111:558–5652008.
View Article : Google Scholar
|
|
10
|
Herrmann A, Hoster E, Zwingers T, et al:
Improvement of overall survival in advanced stage mantle cell
lymphoma. J Clin Oncol. 27:511–518. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Kluin-Nelemans HC, Hoster E, Hermine O, et
al: Treatment of older patients with mantle-cell lymphoma. N Engl J
Med. 367:520–531. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Rummel MJ, Niederle N, Maschmeyer G, et
al: Study group indolent Lymphomas (StiL): Bendamustine plus
rituximab versus CHOP plus rituximab as first-line treatment for
patients with indolent and mantle-cell lymphomas: An open-label,
multicentre, randomized, phase 3 non-inferiority trial. Lancet.
381:1203–1210. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Visco C, Finotto S, Zambello R, et al:
Combination of rituximab, bendamustine, and cytarabine for patients
with mantle-cell non-Hodgkin lymphoma ineligible for intensive
regimens or autologous transplantation. J Clin Oncol. 31:1442–1449.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
The Non-Hodgkin's Lymphoma Classification
Project: A clinical evaluation of the International Lymphoma Study
Group classification of non-Hodgkin's lymphoma. Blood.
89:3909–3918. 1997.PubMed/NCBI
|
|
15
|
Cornes JS: Multiple lymphomatous polyposis
of the gastrointestinal tract. Cancer. 14:249–257. 1961. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Ruskoné-Fourmestraux A, Delmer A, Lavergne
A, et al: Multiple lymphomatous polyposis of the gastrointestinal
tract: Prospective clinicopathologic study of 31 cases. Groupe
D'etude des Lymphomes Digestifs. Gastroenterology. 112:7–16. 1997.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Vose JM: Mantle cell lymphoma: 2012 update
on diagnosis, risk-stratification and clinical management. Am J
Hematol. 87:604–609. 2012. View Article : Google Scholar : PubMed/NCBI
|