Introduction
Differentiated thyroid cancer (DTC) is one of the
most commonly observed types of endocrine cancer, and includes
papillary TC (PTC) and follicular TC (FTC) (1). TC incidence rates have increased
significantly in recent years for various reasons (1). In general, the prognosis of DTC is
positive, however, patients exhibiting distant metastases at the
time of diagnosis demonstrate a markedly worse prognosis (1). The lungs are the most frequent distant
metastatic sites, with an incidence rate of 2–20% (2). The treatment options for adult DTC
include surgery, radioiodine therapy (RAI) and thyroid hormone
suppression, while long-term monitoring is essential following
treatment (3). The current treatment
plan is based on total or near-total thyroidectomy, followed by
radioiodine remnant ablation and subsequent hormone replacement
therapy (3). Measurement of serum
thyroglobulin (Tg) levels, ultrasonography or single-photon
emission computed tomography (SPECT)/CT and radioiodine diagnostic
whole-body scanning (DxWBS) are generally performed during
follow-up examination (4). The
majority of patients exhibiting lung metastases are diagnosed using
chest CT and 131I-WBS prior to RAI (2,4). DxWBS is
frequently performed for the early detection of metastases,
however, it remains controversial whether DxWBS is sensitive enough
to detect early pulmonary metastases, and whether treatment dosage
is affected due to its effect of reducing 131I uptake
(5). By contrast, increased Tg levels
following thyroidectomy and radioiodine remnant ablation indicate
the persistence or recurrence of an active tumor (6,7). However,
there are patients who produce negative CT scans and
131I-WBS positivity for metastases, and it remains to be
elucidated whether RAI is effective in these patients. Another
issue to be elucidated is whether increased Tg levels are a
prerequisite for the performance of DxWBS. The present study is a
retrospective report analyzing 131I therapy in 21 DTC
patients exhibiting lung metastases that were undetected by CT.
Materials and methods
Clinical data
A total of 3,802 patients received RAI for the
treatment of DTC in the Department of Nuclear Medicine at Zhejiang
Cancer Hospital (Hangzhou, China) between January 2007 and
September 2012. Among these patients, 419 exhibited lung
metastases, identified by clinical examination, imaging and
laboratory examination. A total of 21 patients demonstrated no
evidence of lung metastases, as revealed by chest CT prior to the
initial administration of RAI, and these patients exhibited
abnormal lung iodine uptake in post-therapeutic WBS (RxWBS). Among
these 21 patients, 11 were male and 10 were female, and the median
age was 35.4±13.5 years (range, 17–59 years). All patients were
treated with a near-total or total thyroidectomy, and the
pathological tumor classification was PTC (8). The patients exhibited no lung disease or
secondary malignant tumors prior to iodine treatment, and follow-up
times ranged between 18 and 84 months (median, 36 months).
Treatment plan
All 21 DTC patients who exhibited lung metastases
undetected by chest CT scans were initially treated with
radioiodine ablation of thyroid remnants, and subsequent
pretreatment required an iodine-free diet and thyroid hormone
withdrawal for 3–4 weeks. All patients exhibited a clinical
hypothyroid state, with serum thyroid-stimulating hormone levels
(TSH) of >30 mU/l (normal range, 0.38–4.34 mU/l). Routine chest
CT was performed prior to 131I treatment without DxWBS,
for which the dosage was 3.7 GBq. RxWBS was performed 3–5 days
after the oral administration of 131I, with SPECT/CT
fusion imaging if required. The interval time between rounds of
repeated 131I treatment was 4–6 months, and the single
treatment dosage was 5.55–7.4 GBq.
Instruments and materials
An 131I solution was purchased from
Chengdu Zhonghe Radioisotope, Inc., (Chengdu, China) and
131I imaging was performed using an Infinia Hawkeye 4
(GE Healthcare Bio-Sciences, Pittsburgh, PA, USA) with SPECT/CT.
Chest CT was independently performed by the
radiologists/technicians from the Department of Radiotherapy in
Zhejiang Cancer Hospital. Serum Tg and Tg-antibody blood tests were
performed using chemiluminescence (Kit Tg, cat no. 16909903; Kit
TgAb, cat no. 16826601; Roche Diagnostics, Ltd., Burgess Hill, UK),
with a normal range of 1.4–78 ng/ml and 0–115 U/ml,
respectively.
Diagnosis of DTC lung metastasis
undetected by chest CT scan
A lung 131I uptake value higher than the
normal basal level, excluding the physiological uptake and
contamination from the body surface, was considered to be
RxWBS-positive. Lung CT (with 5-mm scanning depth) results
demonstrating no evident bulky nodules or other abnormal high
intensity bulk were considered negative. RxWBS and chest CT results
were independently assessed by two doctors/radiologists from the
Department of Nuclear Medicine and the Department of Radiology
(Zhejiang Cancer Hospital), respectively.
Assessment of therapeutic
effectiveness
The following criteria were used to assess
therapeutic effectiveness: i) Complete response (CR), no clinical
symptoms of lung metastases, no abnormal lung uptake in
131I-WBS and other imaging examinations, and Tg
negativity (serum Tg levels <1 ng/ml with TSH stimulation); ii)
partial response (PR), lung uptake reduced in 131I-WBS
and negative lung metastases in other imaging examinations, with
decreased Tg levels (compared with either TSH inhibition or
stimulation); iii) no response (NR), no improvement or no change in
lung uptake or other imaging examinations, with lung metastases in
other imaging examinations and increased Tg levels. CR and PR were
considered to indicate effective 131I therapy.
Statistical analysis
Data were analyzed using SPSS (version 19.0; IBM
SPSS, Armonk, NY, USA), and the quantitative data are presented as
the mean ± standard deviation. Distribution was analyzed using
Fisher's exact test. P<0.05 was considered to indicate a
statistically significant difference.
Results
Clinical characteristics
Among the 21 patients investigated, there were 9
cases of tumor metastasis. All patients demonstrated lymph node
metastasis, and the average number ratio for neck lymph node
metastasis (percentage of lymph node metastasis cases out of the
total number of lymph node dissection) was 46.2%
(312/675×100=46.2%). A total of 15 patients underwent surgery once,
5 patients underwent surgery twice and 1 patient underwent surgery
6 times, prior to RAI. Pathological tumor-node-metastasis staging
results were as follows: Stage I, 15 patients; stage III, 3
patients; and stage IVa, 3 patients. The interval between initial
RAI and final surgery was <3 months in the majority of patients
(81.0%; 17/21). All 21 patients were administered 131I
treatment 1–5 times, and the average Tg level was 131.8 ng/ml
(range, 0.2–500 ng/ml) pre-TSH stimulation. A total of 3 patients
exhibited neck lymph node metastasis, confirmed by RxWBS together
with local SPECT/CT imaging, and 4 patients exhibited mediastinal
lymph node metastasis. There were 18/21 patients who underwent RAI
<3 times (85.7%), and 2 patients who underwent RAI 4 times
(9.5%). The accumulated dosage for all patients was 3.7–30.34 GBq
(mean, 17.39 GBq).
131I therapy effectiveness
does not demonstrate statistical significance between CR and
NR
The following response rates were observed: CR,
23.8% (5/21); PR, 71.4% (15/21); and NR, 4.8% (1/21). The observed
overall effectiveness was 95.2% (20/21). The difference in
effectiveness was not statistically significant between the CR and
NR groups for gender, age ≥45 years (age at diagnosis), interval
between initial RAI and final surgery, RAI frequency, presence or
absence of extrathyroidal invasion and extrapulmonary metastasis
(Table I).
 | Table I.Independent prognostic factors
predicting radioiodine treatment efficacy in 21 differentiated
thyroid cancer patients with computed tomography-negative pulmonary
metastasis. |
Table I.
Independent prognostic factors
predicting radioiodine treatment efficacy in 21 differentiated
thyroid cancer patients with computed tomography-negative pulmonary
metastasis.
| Clinicopathological
feature | Total patients, n
(%) | CR, n | PR/NR, n | P-value |
|---|
| Gender |
|
|
| 0.450 |
| Male | 11 (52.4) | 2 | 9 |
|
|
Female | 10 (47.6) | 3 | 7 |
|
| Age at diagnosis,
years |
|
|
| 0.557 |
|
<45 | 14 (66.7) | 3 | 11 |
|
| ≥45 | 7
(33.3) | 2 | 5 |
|
| Interval between
intial RAI and final surgery, months |
|
|
| 0.696 |
| ≤3 | 17 (81.0) | 4 | 13 |
|
|
>3 | 4
(19.0) | 1 | 3 |
|
| Total RAI
treatments |
|
|
| 0.421 |
| ≤3 | 18 (85.7) | 5 | 13 |
|
|
>3 | 3
(14.3) | 0 | 3 |
|
| Extrathyroidal
invasion |
|
|
| 0.353 |
| Yes | 9
(42.9) | 3 | 6 |
|
| No | 12 (57.1) | 2 | 10 |
|
| Extrapulmonary
metastasis |
|
|
| 0.098 |
| Yes | 7
(33.3) | 0 | 7 |
|
| No | 14 (66.7) | 5 | 9 |
|
Lung uptake and treatment
effectiveness does not demonstrate statistical significance between
diffuse and focused uptake patients
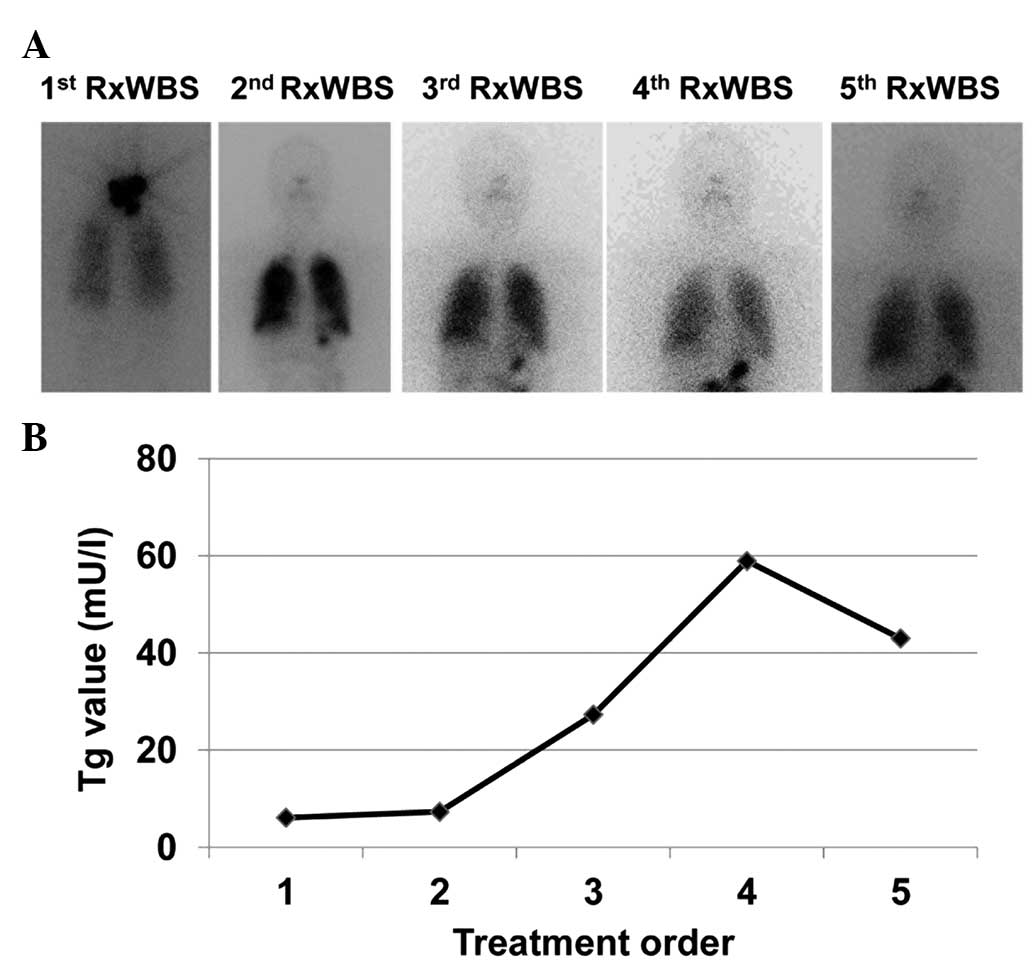
A total of 12 patients demonstrated diffuse uptake,
and the remaining 9 exhibited focused uptake with decreased
131I deposition, with no CR. There were 5 cases of I-WBS
negativity among the diffuse uptake patients, and 6 cases
demonstrated reduced uptake compared with pre-treatment levels,
with 1 patient demonstrating a progressive increase of Tg and Tg
antibody levels during 5 treatments, and exhibiting diffuse nodules
on chest CT (Fig. 1). The CR rate was
41.7% (5/12), and the difference in CR rate between the diffuse
uptake and focused uptake patients was not statistically
significant (P=0.123).
A correlation exists between Tg levels
and extrapulmonary metastasis
All 21 patients were administered treatment 1–5
times, and 7 demonstrated extrapulmonary metastases in RxWBS. Among
these 7 patients, 3 were identified to have neck lymph node
metastases and 4 possessed mediastinal lymph node metastases. There
was a correlation between Tg levels and extrapulmonary metastasis.
All patients demonstrated extrapulmonary metastasis when Tg levels
were >87.5 ng/ml (area under curve, 1.0; P<0.001).
Discussion
The 10-year survival rate of PTC and FTC patients
following ‘thyroidectomy + 131Iodine radiotherapy + TSH
inhibition’ has been observed to be 93 and 85%, respectively
(9). However, almost 2% of PTC
patients and 6% of FTC patients were diagnosed with distant
metastases during their initial hospital visit or follow-up visit,
and the survival rate is <50% for these patients (10). The lungs are the most common
metastatic sites for DTC, and the diagnosis is primarily dependent
on medical imaging (10,11). However, DTC lung metastases typically
progress slowly and frequently present with a spotty lung
distribution, various tumor sizes and tumor nodules with homogenous
density (12,13). Chest X-ray may frequently lead to an
incorrect or missed diagnosis due to the detection limit (11). Relapsed DTC or metastatic DTC is
frequently 131I-enriched. Therefore, 131I-WBS
is one of the most specific methods for DTC diagnosis, not only for
assessment of the therapeutic effect of 131I, but
additionally for the diagnosis of DTC relapse or metastasis
(4). In the present study, all
patients underwent chest CT scanning prior to 131I
treatment, and 21 patients demonstrated no metastases, however,
these patients were subsequently diagnosed with lung metastases
during 131I radiotherapy. Thus, 131I therapy
is more accurate for DTC staging, and contributes significantly to
early diagnosis, early treatment and an improved prognosis.
The exact efficacy of 131I treatment for
DTC lung metastases has not been consistent, and the response and
CR rates vary widely among studies (range, 10–90%) (6,14–16). In the present study, the response rate
was 95.2%, and the CR rate was 23.8%, which were higher than the
previously reported response rates. The reason underlying these
superior response rates may be ascribed as due to several aspects.
The survival time for 131I-treated DTC patients,
including patients with lung metastases, is relatively long
(17,18). The criteria for specific studies may
be different. Furthermore, although the 131I treatment
plan for DTC patients is relatively standard, the pre-treatment
status of patients, the dosage choice, the follow-up design and the
response standard may be different (12). In addition, current CT scanning is
able to detect tumor nodules with diameters of 3–5 mm. In patients
with metastasis that is not detected by CT, the nodule size is
likely to be <3 mm in diameter and is possibly in the early
stages of metastasis. However, the penetration distance of
β-irradiation from 131I inside the tissue is relatively
short (average distance, 1 mm) (18).
For these patients, the lung deposits of 131I are
primarily located within the DTC tumor nodules, which allows the
achievement of maximum local irradiation. This may explain why the
131I treatment time and accumulated dosages were lower
in the present study compared with previous studies, and is
consistent with reports that the prognosis of patients exhibiting
diffuse lung metastases is superior to that of patients with
focused lung metastases, following 131I treatment
(13).
Serum Tg is exclusively produced by the thyroid
gland, and serum Tg will fall to markedly reduced levels following
thyroidectomy or partial thyroidectomy and residual tissue removal
with iodine radiotherapy. The return or increase of serum Tg levels
indicates DTC treatment failure, reoccurrence or metastasis
(6). Thus, serum Tg monitoring is a
simple and reliable detection method for monitoring DTC
reoccurrence, metastasis and therapy efficacy (14). In the present study, 20/21 patients
demonstrated decreased serum Tg levels following 131I
therapy, and no new metastases were identified by follow-up CT
scanning. American Thyroid Association guidelines have indicated
that an increase in serum Tg levels [>10 mg/l following the end
of levothyroxine (LT4) administration] in the follow-up monitoring
of DTC patients who received radioiodine therapy suggests
metastasis, and 131I therapy is recommended (3). However, there was no specific analysis
concerning the significance of such an increase in Tg levels. In
the present study, it was identified that 16/21 patients
demonstrated an increase in serum Tg levels (>10 ng/ml) in the
initial RAI, following the conclusion of LT4 intake, and 7 patients
(Tg levels, >87.85 ng/ml) were confirmed to exhibit lung
metastases in the subsequent RxWBS, with a statistically
significant difference. Thus, it was suggested that DxWBS may not
be essential for DTC patients demonstrating low serum Tg levels,
but that it is necessary for patients exhibiting high levels of
serum Tg. This result requires additional investigation with a
larger sample size. In the present study, no DxWBS was performed
pre-RAI due to concerns regarding the ‘stunning’ effect, and it is
possible that an insufficient RAI dosage was administered during
the initial treatment. This hypothesis requires additional
investigation with a larger sample size.
In conclusion, DTC patients exhibiting lung
metastasis not detected by CT scanning responded well to
131I radiotherapy and demonstrated a positive prognosis
in the present study. Serum Tg levels prior to 131I
treatment may correlate with metastasis, and this may suggest the
importance of diagnostic WBS prior to radiotherapy. This hypothesis
requires additional investigation with a larger sample size.
References
|
1
|
Kim TY, Kim WG, Kim WB and Shong YK:
Current status and future perspectives in differentiated thyroid
cancer. Endocrinol Metab (Seoul). 29:217–225. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Lin JD, Chao TC, Chou SC and Hsueh C:
Papillary thyroid carcinomas with lung metastases. Thyroid.
14:1091–1096. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
American Thyroid Association (ATA)
Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid
Cancer. Cooper DS, Doherty GM, Haugen BR, Kloos RT, et al: Revised
American Thyroid Association management guidelines for patients
with thyroid nodules and differentiated thyroid cancer. Thyroid.
19:1167–1214. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Ilgan S, Karacalioglu AO, Pabuscu Y, et
al: Iodine-131 treatment and high-resolution CT: Results in
patients with lung metastases from differentiated thyroid
carcinoma. Eur J Nucl Med Mol Imaging. 31:825–830. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tachi Y, Iwano S, Kato K, Tadokoro M and
Naganawa S: Diagnostic whole-body scanning before radioiodine
therapy for pulmonary metastases of differentiated thyroid cancer:
Predictive value and recommendations. Clin Nucl Med. 33:845–851.
2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Phan HT, Jager PL, van der Wal JE, Sluiter
WJ, Plukker JT, Dierckx RA, Wolffenbuttel BH and Links TP: The
follow-up of patients with differentiated thyroid cancer and
undetectable thyroglobulin (Tg) and Tg antibodies during ablation.
Eur J Endocrinol. 158:77–83. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Pace L, Klain M, Albanese C, Salvatore B,
Storto G, Soricelli A and Salvatore M: Short-term outcome of
differentiated thyroid cancer patients receiving a second
iodine-131 therapy on the basis of a detectable serum thyroglobulin
level after initial treatment. Eur J Nucl Med Mol Imaging.
33:179–183. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Edge SB, Byrd DR, Compton CC, et al: AJCC
Cancer Staging Manual. (7th). (New York, NY, USA). Springer-Verlag.
2010.
|
|
9
|
Hundahl SA, Fleming ID, Fremgen AM and
Menck HR: A National Cancer Data Base report on 53,856 cases of
thyroid carcinoma treated in the U.S., 1985–1995 [see comments].
Cancer. 83:2638–2648. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Shaha AR, Shah JP and Loree TR:
Differentiated thyroid cancer presenting initially with distant
metastasis. Am J Surg. 174:474–476. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bal CS, Kumar A, Chandra P, Dwivedi SN and
Mukhopadhyaya S: Is chest x-ray or high-resolution computed
tomography scan of the chest sufficient investigation to detect
pulmonary metastasis in pediatric differentiated thyroid cancer?
Thyroid. 14:217–225. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Lang BH, Wong KP, Cheung CY, Wan KY and Lo
CY: Evaluating the prognostic factors associated with
cancer-specific survival of differentiated thyroid carcinoma
presenting with distant metastasis. Ann Surg Oncol. 20:1329–1335.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Casara D, Rubello D, Saladini G, et al:
Different features of pulmonary metastases in differentiated
thyroid cancer: Natural history and multivariate statistical
analysis of prognostic variables. J Nucl Med. 34:1626–1631.
1993.PubMed/NCBI
|
|
14
|
Ma C, Xie J and Kuang A: Is empiric 131I
therapy justified for patients with positive thyroglobulin and
negative 131I whole-body scanning results? J Nucl Med.
46:1164–1170. 2005.PubMed/NCBI
|
|
15
|
Shaha AR, Shah JP and Loree TR: Low-risk
differentiated thyroid cancer: The need for selective treatment.
Ann Surg Oncol. 4:328–333. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Pitoia F, Bueno F and Cross G: Long-term
survival and low effective cumulative radioiodine doses to achieve
remission in patients with 131Iodine-avid lung metastasis from
differentiated thyroid cancer. Clin Nucl Med. 39:784–790. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Higashi T, Nishii R, Yamada S, et al:
Delayed initial radioactive iodine therapy resulted in poor
survival in patients with metastatic differentiated thyroid
carcinoma: A retrospective statistical analysis of 198 cases. J
Nucl Med. 52:683–689. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Grosev D, Loncarić S, Huić D and Dodig D:
Geometric models in dosimetry of thyroid remnant mass.
Nuklearmedizin. 47:120–126. 2008.PubMed/NCBI
|