Introduction
The most frequent site of bone metastasis is the
spine, and 39% of patients with bone metastases exhibit axial bone
lesions (1,2). The most common location for spinal
metastases is the thoracic spine (40–50%); however, all spinal
column levels may be affected and >70% of spinal metastases may
involve more than one vertebral level at presentation (3). The predominant symptom in spinal
metastases is pain, including constant localized, radicular and
axial pain (4). In addition to pain,
spinal metastases may lead to pathological fractures of the
vertebrae and paraplegia caused by spinal cord compression
(5). Advances in diagnosing and
treating patients with spinal metastases have improved the survival
time and quality of life (QOL) of patients, therefore, controlling
the pain that is experienced has become a major focus (6). Conservative treatments, including the
use of analgesics, chemotherapy and radiotherapy, can be transient
and ineffective, and traditional invasive surgery is typically
unsuitable for patients with spinal metastases due to the high risk
of surgical complications and the associated short life expectancy.
More recent technological advances in combination with innovative
interventional radiology techniques have provided less invasive
treatment therapy for patients with spinal metastases. Percutaneous
kyphoplasty (PKP) is used to treat patients with painful metastases
in the spine (7). PKP is a minimally
invasive, radiologically-guided procedure that involves injecting
bone cement into target vertebrae following the insertion of a
balloon into the vertebral body to create a cavity. This allows
relatively low pressure and high-viscosity bone cement disposition,
which lowers the cement leakage rate (8–10).
The current study retrospectively reviewed the
clinical and radiological outcomes of PKP in patients with
osteolytic-associated spinal metastases in the thoracic or lumbar
vertebrae, with an aim to evaluate the efficacy and safety of PKP
in the treatment of these patients.
Patients and methods
Patient characteristics
Between April 2009 and June 2014, 282 patients with
399 vertebral lesions (thoracic vertebrae, 223; lumbar vertebrae,
176) received PKP at the First Affiliated Hospital of China Medical
University (Shenyang, China) in our hospital. The majority of the
patients received systemic chemotherapy or radiotherapy prior to
PKP; however, the severe pain these patients experienced remained
following the treatments. All the patients met the following
inclusion criteria: Presence of a primary malignant tumor, which
was diagnosed by pathology or cytology; grade D-E spinal cord
function, according to the Frankel grading system (11); adequate hematological, hepatic, renal,
neuronal and cardiac functions, and the ability to maintain a prone
position for ≥2 h; a Karnofsky performance score (KPS) of ≥60; an
expected survival time of ≥3 months; vertebral destruction, which
was dominated by osteolytic lesions; thoracic and lumbar vertebral
fractures confirmed by physical and imaging examinations; and a
lesion region located below the 6th thoracic vertebra. The
characteristics and tumor data of the patients are presented in
Table I. All patients were informed
of the future publication of this study and provided their consent.
The study was approved by the Institutional Board at the First
Affiliated Hospital of China Medical University.
 | Table I.Clinical characteristics of 282
patients with spinal metastases. |
Table I.
Clinical characteristics of 282
patients with spinal metastases.
| Characteristics | Value |
|---|
| Age in years, n
(%) |
|
|
25–34 | 11 (3.90) |
|
35–44 | 12 (4.26) |
|
45–54 | 84
(29.79) |
|
55–64 | 60
(21.28) |
|
65–74 | 96
(34.04) |
|
75–84 | 12 (4.26) |
|
85–94 | 7
(2.48) |
| Gender, n (%) |
|
|
Female | 156 (55.32) |
| Male | 126 (44.68) |
| Primary tumor, n
(%) |
|
|
Liver | 60
(21.28) |
| Lung | 132 (46.81) |
|
Breast | 24 (8.51) |
|
Cervical | 24 (8.51) |
|
Prostate | 13 (4.61) |
|
Kidney | 12 (4.26) |
|
Bladder | 12 (4.26) |
|
Lymph | 5
(1.77) |
| No. of vertebral
lesions treated, n (%) |
|
| 1 | 180 (63.83) |
| 2 | 84
(29.79) |
| 3 | 14 (4.96) |
| 4 | 4
(1.42) |
| VAS |
6.85±0.97 |
| KPS |
70.42±10.83 |
| QOL | 67.74±9.33 |
| Kyphotic angle,
° | 16.68±1.46 |
| Anterior vertebral
height, mm | 18.45±5.62 |
Evaluating the efficacy of PKP
The efficacy of PKP was evaluated using the visual
analog scale for pain (VAS), KPS and QOL scores [short form with 36
questions (SF-36)]. In addition, radiographical data, including the
degree of restoration of the kyphotic angle and anterior vertebral
height, and the leakage of bone cement, were measured. The safety
of PKP was assessed by evaluating the complications and side
effects reported during or post-surgery. A clinical assessment of
the patients was performed on the day prior to the surgery and at
24 h, 3 months, 6 months and 1-year post-surgery, as well as at the
last follow-up date. The KPS and QOL scores were calculated 3
months after PKP, and baseline KPS and QOL scores were assessed
prior to the procedure. A clinical follow-up examination of the
patients was conducted by Dr Feng Chen, Dr Wei Shan and Dr Yang Gao
(Department of Interventional Radiology, First Hospital of China
Medical University), and diagnostic images were independently
evaluated by Mr. Xiang Wang (Department of Geriatrics, The First
Affiliated Hospital of China Medical University). All the patients
received conventional chemotherapy following the surgery, which was
specific to the primary tumor.
PKP procedure
The following instruments were used in the PKP
procedure: Puncture needles (3.2–4.0 mm in diameter), hollow
diamond and solid diamond tipped needles, precision injector
pressure device (Longguan Co., Jinan, China) to assess cement
pressure during injection, surgical balloon, bone cement injection
gun (Longguan Co.); bone cement (Heraeus Medical GmbH, Wehrheim,
Germany); and surgical hammer (Beijing Operation Apparatus Factory,
Beijing, China).
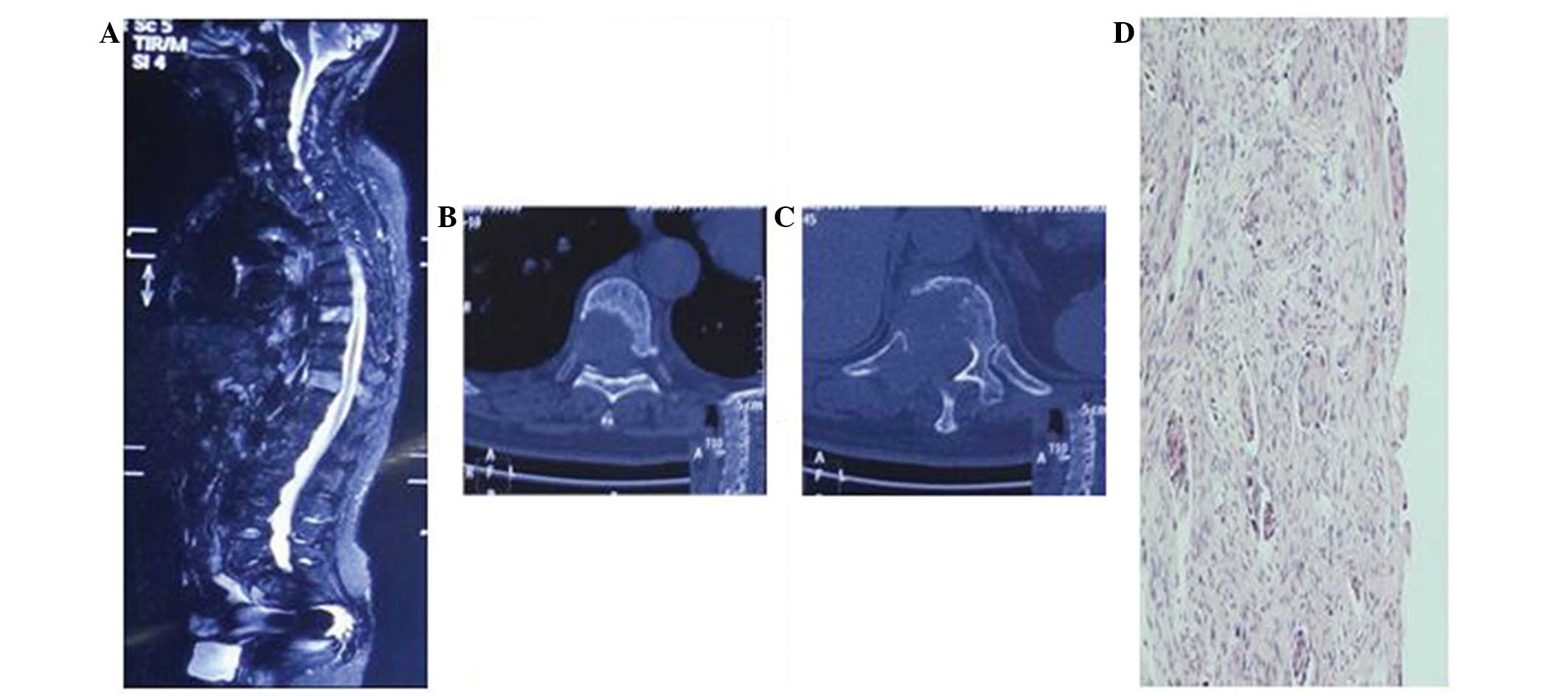
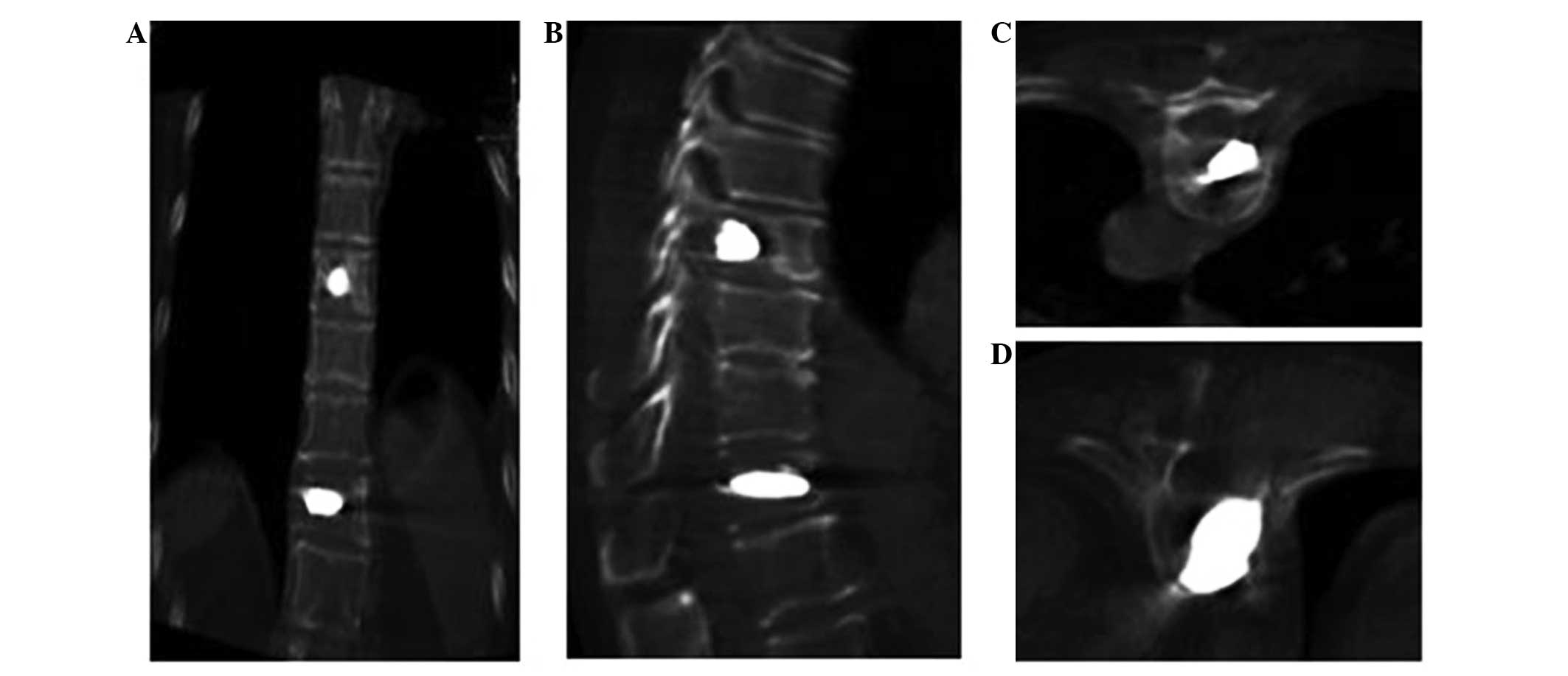
X-ray, computed tomography (CT) and magnetic
resonance imaging (MRI) were performed prior to surgery to
determine the location and number of lesions, and the degree of
collapse of the vertebrae (Fig. 1).
In addition, CT and MRI established if the back wall of the
vertebral body was intact and if the spinal cord was compressed.
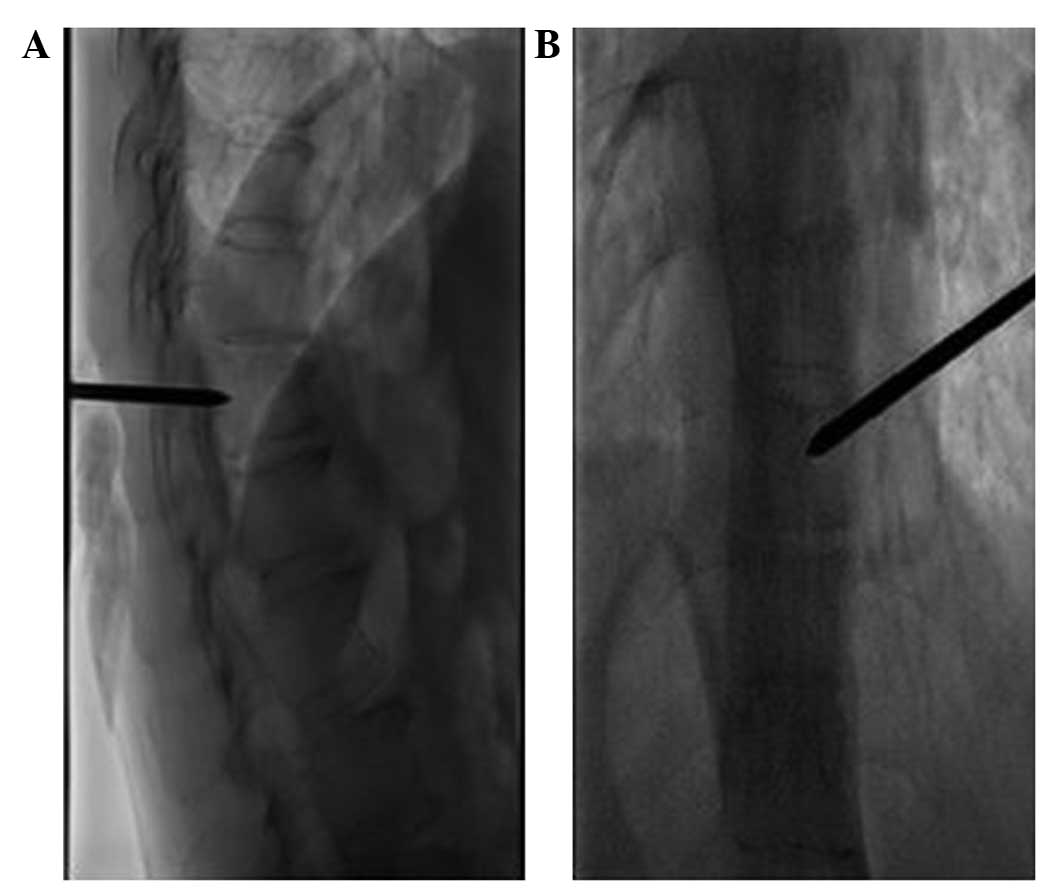
PKP was guided by a Digital Subtraction Angiology (DSA) machine (GE
Healthcare Bio-Sciences, Pittsburgh, PA, USA) in the interventional
radiology suite following an analysis of the radiological images.
Local anesthesia (2% lidocaine; 5 ml) was administered to the
patient prior to the surgery. The patient was placed in the prone
position and injection needles were used to puncture unilaterally
or bilaterally through the pedicle of the vertebral arch (if the
metastasis was located in a lumbar vertebra) or rib vertebral
joints (if the metastasis was located in a thoracic vertebra).
When the needle tip reached the back wall of the
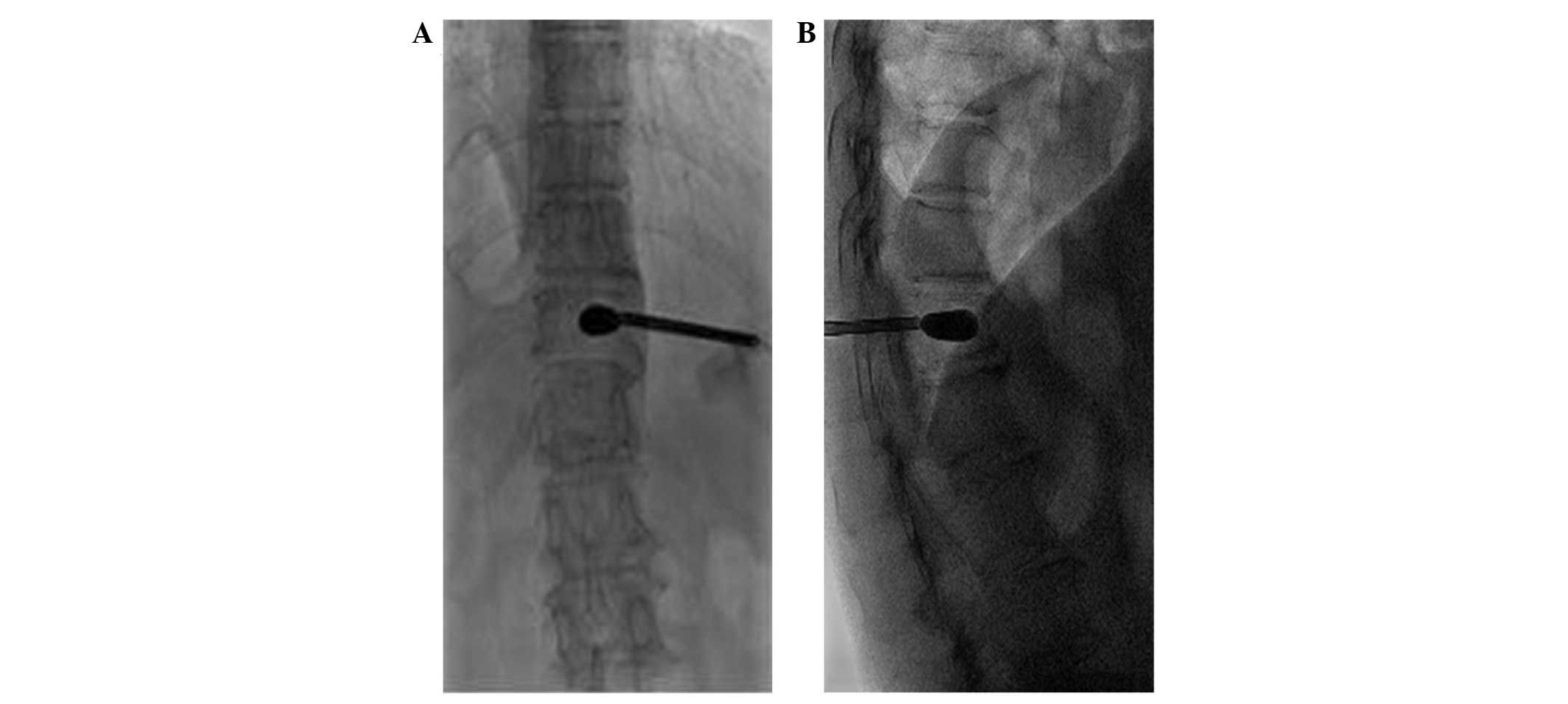
vertebra (Fig. 2), 3-dimensional CT
scanning was used, in combination with DSA, to ensure that the
spinal cord was not punctured and the procedure was effective
(Fig. 3). A surgical hammer was used
to aid the needle placement into the anterior quadrant of the
targeted vertebral body. Hollow and solid diamond tipped needles
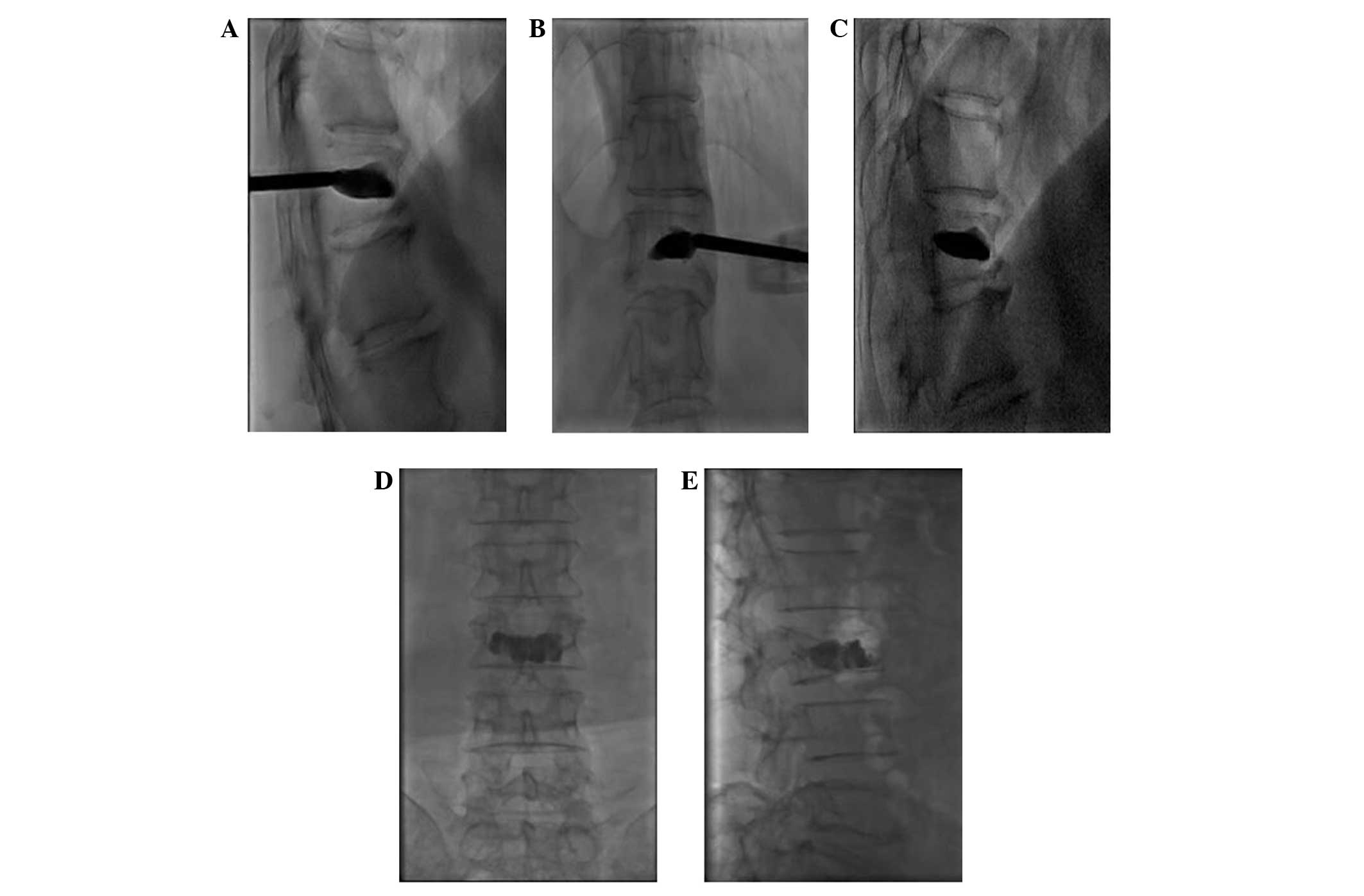
were used to polish the tract. Subsequently, a balloon, which was
used to restore vertebral body height and create a cavity in the
vertebra for the injection of bone cement, was inserted into the
vertebra using fluoroscopic monitoring. The balloon was inflated
and viewed using a contrast agent. If it was challenging to inflate
the balloon or a portion of the balloon reached the vertebral
margin, inflation was terminated and the balloon was removed
(Fig. 4). Bone cement, a mixture of
polymethyl methacrylate (PMMA) and non-ionic contrast medium, was
injected into the vertebra using a bone cement injecting gun and
fluoroscopic monitoring. When the PMMA had solidified the injection
needles were removed. The volume of bone cement injected into the
vertebra was 1–5 ml, with a mean of 1.9 ml for the thoracic
vertebrae and 1.97 ml for the lumbar vertebrae (Figs. 5 and 6).
Following the surgery, the patients were required to rest for 6 h,
and during this period the vital signs, neurology, urine volume,
bowel movement, sensory motor functions of the lower limbs, and
alterations in routine blood tests and CD4+ and
CD8+ T cell subpopulations were monitored. The patients
received mannitol (250 ml injection, daily) and solu-medrol (80 mg
injection, daily) for three days to treat spinal cord edema.
Statistical analysis
Continuous data were expressed as the mean ±
standard deviation (SD). A comparison of continuous variables pre-
and post-surgery was performed using a one-way analysis of
variance. P≤0.05 was considered to indicate a statistically
significant difference.
Results
Patient follow-up
The PKP procedures performed on 282 patients with
spinal metastases were successful and without severe complications.
The success rate of the puncture surgery was 100%. The clinical
assessment of the patients was performed at 24 h, 3 months, 6
months and 1 year post-surgery, and the last follow-up assessment
was performed via outpatient review or telephone. All 282 patients
underwent follow-up assessments 24 h and 3 months post-surgery, and
272 patients were evaluated at 6 months post-surgery. A total of 60
patients were lost to follow-up at 1-year post-surgery. The
follow-up duration ranged between 105 days and 15 months (mean, 401
days).
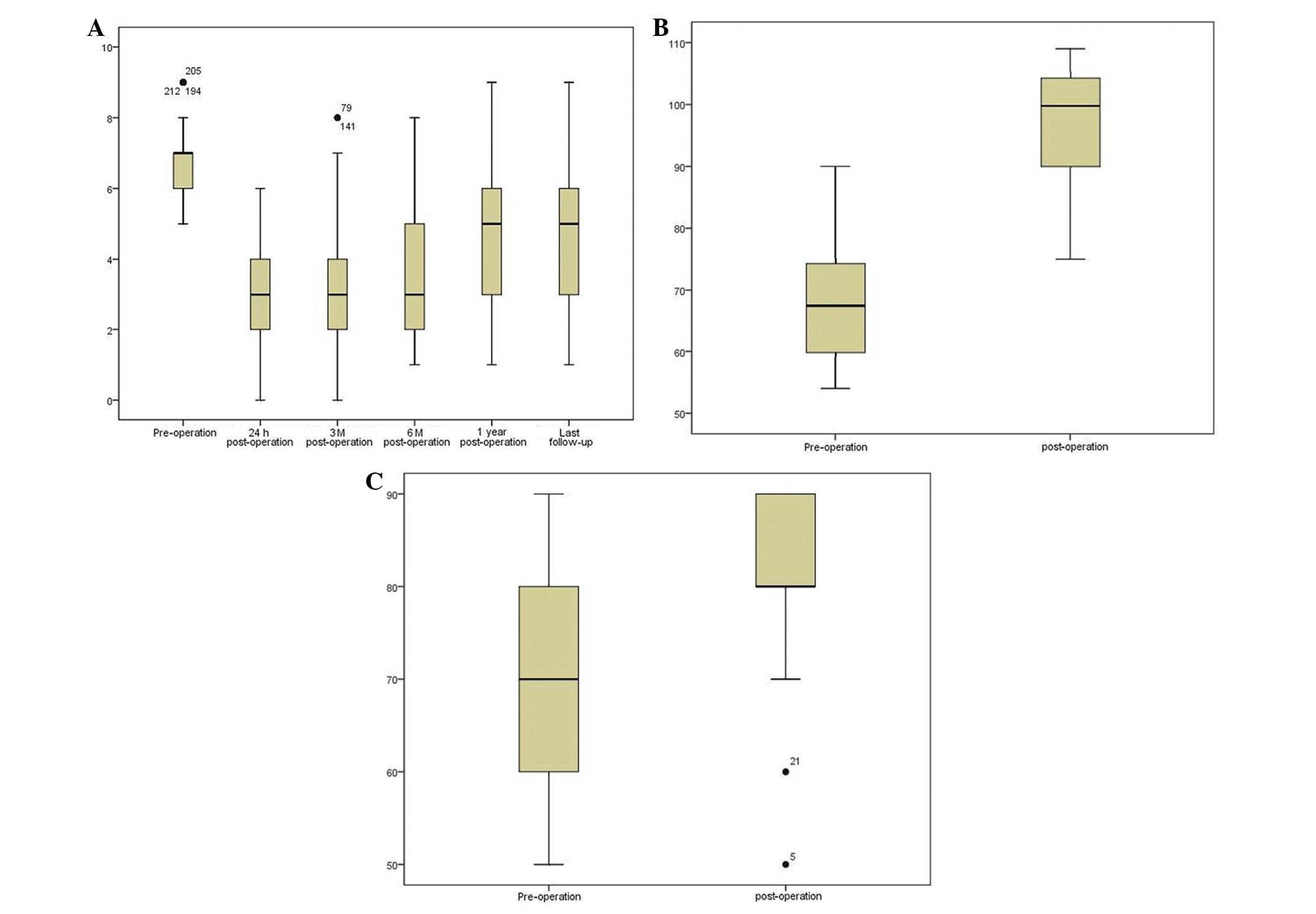
VAS
For pain evaluation, the patients were asked to
evaluate their degree of pain, according to VAS, which uses a score
of 0–10 to indicate levels of pain between mild and severe (0, no
pain; 10, severe pain). All the patients exhibited pain relief
following the surgery. The pre-operative VAS was 6.85±0.97, which
decreased to 3.11±1.38 24 h post-operatively (P<0.001). The VAS
of the patients remained largely unaltered at 3 months (3.17±1.521;
P<0.001; 282 patients), 6 months (3.58±1.63; P<0.001; 272
patients) and 1 year (4.61±1.65; P<0.001; 222 patients), and at
the last follow-up (4.91±1.99; P<0.001; 219 patients) (Fig. 7A). In addition, the analgesic intake
of the patients decreased following PKP (data not shown).
KPS
The physical condition of the patients was assessed
by KPS. KPS score is used to assess how the disease of a patient is
progressing, how it affects the daily living abilities of the
patient, and determines the appropriate treatment and prognosis of
the patient. A patient with a KPS score of 100, exhibits no signs
and symptoms, while a score of 0 indicates patient mortality. Thus,
the higher the score, the better the health status. In the present
study, the pre-operative KPS was 70.42±10.83, which increased at 3
months post-surgery (80.83±10.59; P<0.001) (Fig. 7B).
QOL
QOL (SF-36) was developed by a USA Boston health
study (12,13), and was based on a previous study
concerning the medical outcomes (14). The QOL health questionnaire is widely
used in the evaluation of clinical trials and health policies. The
questionnaire consists of 9 topics: Physical functioning,
role-physical, bodily pain, general health, vitality, social
functioning, role-emotional, mental health and reported health
transition. A patient with a score of 100, exhibits no signs and
symptoms, while a score of 0 indicates patient mortality. Thus, the
higher the score, the better the health status. In the present
results, the pre-operative QOL score was 67.74±9.33, which then
increased to 97.41±9.55 at 3 months post-surgery (P<0.001;
Fig. 7C).
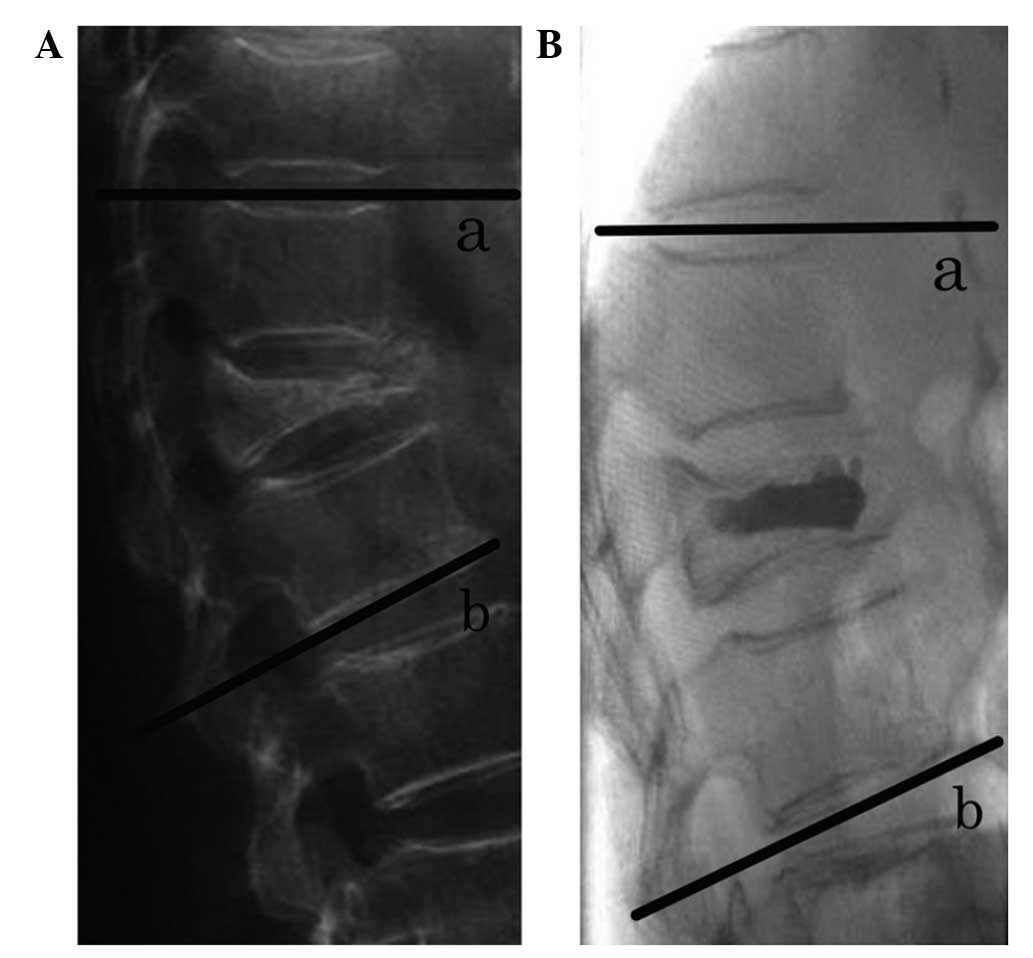
Radiographical evaluation
The kyphotic angle is defined as the Cobb angle
measured between the superior endplate of the vertebra one level
above the treated vertebra and the inferior endplate of the
vertebral body one level below the treated vertebra, using a
lateral X-ray image (Fig. 8)
(15). In the present study, the
pre-operative kyphotic angle was 15.68±1.46°, which decreased at 3
months post-surgery (7.71±1.51°) (P<0.05). In addition, the
pre-operative anterior vertebral height (18.40±5.59 mm) increased
to 24.20±6.261 mm at 3 months post-surgery (P<0.05).
Complications
Complications reported consisted of minor
paravertebral leakage of bone cement, which occurred in 10 patients
due to a cortical defect. Spinal cord compression, pulmonary
embolism, leukopenia, decreased immunological function and nerve
root compression were not detected in any patient.
Discussion
Intractable pain is a common symptom of bone
metastases (16). Even following the
administration of analgesics and chemotherapy, the alleviation of
pain may be challenging (17). This
leads to a poor QOL and decreased survival time of patients with
bone metastases. The majority of treatment is palliative (18). Surgery and radiation therapy or a
combination of the two may be used, but often, such patients with a
limited life expectancy do not undergo surgery due to the long
recovery period, and high morbidity and mortality rates that may
result from surgery (19). Surgery is
not suitable for treating patients with multiple metastatic spinal
tumors (19–21). Radiotherapy is the most usual
treatment for spinal metastases; however, pain relief is delayed
and not always absolute (22).
Therefore, PKP, which is a minimally invasive technique, is a
potential treatment option for patients with spinal metastases, and
is currently used for pain relief and spinal stabilization. Due to
the development of interventional radiology, PKP has become widely
accepted as an effective treatment option for patients with spinal
metastases (23).
Cotten et al (24) and Cortet et al (25) reported that percutaneous
vertebroplasty plays a great role in treating patients with
vertebral metastases and multiple myeloma, and that the pain
patients experience could completely disappear. The remission rate
of the vertebral metastases was 67.5 and 68.5%, respectively, and
the partial pain relief rates were each 30%. The majority of
lesions were treated by filling the lesion with bone cement, which
stagnates disease and provides structure to the spine, preventing
additional damage and collapse. By contrast, PKP, attempts to
restore spinal alignment by the placement of bone cement at a lower
pressure into a cavity in the vertebrae, which is created using a
surgical balloon (26). Previous
studies have reported that PKP results in considerably less cement
extravasation compared with injecting bone cement into vertebral
bodies at a higher pressure or without balloon insertion (9,27–29).
In this study, the mean VAS score decreased
significantly at 6 months and the last follow-up (mean ±SD:
3.58±1.63 and 4.91±1.99, respectively). Therefore, the patients in
the study exhibited a significant improvement in pain relief
following surgery, which may be associated with the effect of the
bone cement and the stabilization of the spine (26). The dependence that the patients had on
analgesics also greatly decreased. In addition, the functional
status of the patients increased. The mean pre-operative KPS score
increased between 70.42±10.83 and 80.83±10.60 post-operatively. The
current results demonstrated that the insertion of the surgical
balloon restored the pre-operative mean height of the vertebra,
between 18.40±5.59 and 24.20±6.26 mm post-operatively. Furthermore,
the mean kyphotic angle was reduced from 15.68±1.461° pre-operation
to 7.71±1.512° post-operation. A mean correction of 7.9° was
achieved in the local spinal kyphosis, which is similar to the 8.8°
reported by a previous study (29).
The most common complication of PKP is extravasation
of the bone cement (30,31). A previous meta-analysis demonstrated
cement extravasation in 7% of patients following PKP and 20%
following vertebroplasty (32). In
the present study, cement extravasation occurred asymptomatically
in 11.5% of the vertebrae treated. The cavity formation in PKP
significantly decreases the rate of vascular and transcortical
extravasation of the cement (29).
Compared with previous studies, this finding indicated that an
injection of high-viscosity cement at a low pressure into a
previously formed cavity (PKP) is more effective than an injection
of low-viscosity cement at high pressure into an unreduced
vertebral body (vertebroplasty) (33–35).
Therefore, PKP is considered to be a safer and more effective
treatment option.
There were a few limitations to the present study.
Firstly, there were a small number of patients, which possibly
affected the statistical power. Secondly, the study had a short
follow-up period (mean, 401 days), which is considered to be too
short a time period. Thirdly, the present study was retrospective,
although comprehensive data analysis was performed. Therefore,
additional prospective studies may aid in gathering more definitive
evidence.
In conclusion, the present study indicates that PKP
is an effective and minimally invasive procedure for the treatment
of patients with spinal metastases, and that the technique leads to
a significant improvement in the pain and functional status of
patients. In addition, PKP is more manageable and carries less risk
compared with vertebroplasty.
References
|
1
|
Berrettoni BA and Carter JR: Mechanisms of
cancer metastasis to bone. J Bone Joint Surg Am. 68:308–312.
1986.PubMed/NCBI
|
|
2
|
Tatsui H, Onomura T, Morishita S, Oketa M
and Inoue T: Survival rates of patients with metastatic spinal
cancer after scintigraphic detection of abnormal radioactive
accumulation. Spine. 21:2143–2148. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Chi JH and Gokaslan ZL: Vertebroplasty and
kyphoplasty for spinal metastases. Curr Opin Support Palliat Care.
2:9–13. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Georgy BA: Metastatic spinal lesions:
State-of-the-art treatment options and future trends. AJNR Am J
Neuroradiol. 29:1605–1611. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yang ZZ, Xu JB, Yuan T, Qian BS, Zhang JY,
Li WZ, Li JL, Xiao YB, Peng M, Li Y and Luan L: Treating metastatic
vertebral tumor with percutaneous vertebroplasty: A report of 28
cases. Ai Zheng. 24:194–198. 2005.(In Chinese). PubMed/NCBI
|
|
6
|
Zhang HT, Chen GD, Yang HL and Luo ZP:
Percutaneous kyphoplasty in the treatment of osteoblastic-related
spinal metastases. J Spinal Disord Tech: Jul. 26:2013.(Epub ahead
of print).
|
|
7
|
Qian Z, Sun Z, Yang H, Gu Y, Chen K and Wu
G: Kyphoplasty for the treatment of malignant vertebral compression
fractures caused by metastases. J Clin Neurosci. 18:763–767. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Dudeney S, Lieberman IH, Reinhardt MK and
Hussein M: Kyphoplasty in the treatment of osteolytic vertebral
compression fractures as a result of multiple myeloma. J Clin
Oncol. 20:2382–2387. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Lieberman IH, Dudeney S, Reinhardt MK and
Bell G: Initial outcome and efficacy of ‘kyphoplasty’ in the
treatment of painful osteoporotic vertebral compression fractures.
Spine. 26:1631–1638. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Bouza C, López T, Magro A, Navalpotro L
and Amate JM: Efficacy and safety of balloon kyphoplasty in the
treatment of vertebral compression fractures: A systematic review.
Eur Spine J. 15:1050–1067. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Frankel HL, Hancock DO, Hyslop G, Melzak
J, Michaelis LS, Ungar GH, Vernon JD and Walsh JJ: The value of
postural reduction in the initial management of closed injuries of
the spine with paraplegia and tetraplegia. I. Paraplegia.
7:179–192. 1969. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Ware JE, Snow KK, Kosinski M and Gandek B:
SF-36 Health Survey: Manual and Interpretation Guide. The Health
Institute (Boston, MA). New England Medical Center. 1993.
|
|
13
|
Newnham EA, Harwood KE and Page AC:
Evaluating the clinical significance of responses by psychiatric
inpatients to the mental health subscales of the SF-36. J Affective
Disord. 98:91–97. 2007. View Article : Google Scholar
|
|
14
|
Bai GT, Ma YW and Jiang L: Application
progress of SF-36 at home and abroad. J Clin Res. 12:2367–2368.
2009.(In Chinese).
|
|
15
|
Cobb J: Outline for the study of
scoliosis. AAOS Instr Course Lect. 5:261–275. 1948.
|
|
16
|
Bienz M and Saad F: Management of bone
metastases in prostate cancer: A review. Curr Opin Support Palliat
Care. 9:261–267. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Silverman SL: The clinical consequences of
vertebral compression fracture. Bone. 13(Suppl 2): S27–S31. 1992.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
McDonald R, Chow E, Rowbottom L, Bedard G,
Lam H, Wong E, Popovic M, Pulenzas N and Tsao M: Quality of life
after palliative radiotherapy in bone metastases: A literature
review. J Bone Oncol. 4:24–31. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Yang Z, Yang D, Xie L, Sun Y, Huang Y, Sun
H, Liu P and Wu Z: Treatment of metastatic spinal tumors by
percutaneous vertebroplasty versus percutaneous vertebroplasty
combined with interstitial implantation of 125I seeds. Acta Radiol.
50:1142–1148. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Li Y, Gu YF, Sun ZK, Wu CG, Li YD, Wang W,
Chen YC and Lu J: Comparison of percutaneous vertebroplasty with
and without interventional tumour removal for malignant vertebral
compression fractures with symptoms of neurological compression.
Eur Radiol. 23:2754–2763. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Taylor JW and Schiff D: Metastatic
epidural spinal cord compression. Semin Neurol. 30:245–253. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shimony JS, Gilula LA, Zeller AJ and Brown
DB: Percutaneous vertebroplasty for malignant compression fractures
with epidural involvement. Radiology. 232:846–853. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Sun G, Jin P, Li M, et al: Percutaneous
vertebroplasty for pain management in spinal metastasis with
epidural involvement. Technol Cancer Res Treat. 10:267–274.
2011.PubMed/NCBI
|
|
24
|
Cotten A, Dewatre F, Cortet B, Assaker R,
Leblond D, Duquesnoy B, Chastanet P and Clarisse J: Percutaneous
vertebroplasty for osteolytic metastases and myeloma: Effects of
the percentage of lesion filling and the leakage of methyl
methacrylate at clinical follow-up. Radiology. 200:525–530. 1996.
View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Cortet B, Cotton A, Boutry N, Dewatre F,
Flipo RM, Duquesnoy B, Chastanet P and Delcambre B: Percutaneous
vertebroplasty in patients with osteolytic metastases or multiple
myeloma. Rev Rev Rhum Engl Ed. 64:177–183. 1997.PubMed/NCBI
|
|
26
|
Yu C-W, Hsieh M-K, Chen LH, et al:
Percutaneous balloon kyphoplasty for the treatment of vertebral
compression fractures. BMC Surg. 14:32014. View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Voggenreiter G: Balloon kyphoplasty is
effective in deformity correction of osteoporotic vertebral
compression fractures. Spine. 30:2806–2812. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Ledlie JT and Renfro MB: Kyphoplasty
treatment of vertebral fractures: 2-year outcomes show sustained
benefits. Spine. 31:57–64. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Phillips FM, Ho E, Campbell-Hupp M,
McNally T, Wetzel Todd F and Gupta P: Early radiographic and
clinical results of balloon kyphoplasty for the treatment of
osteoporotic vertebral compression fractures. Spine. 28:2260–2267.
2003. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Fourney DR, Schomer DF, Nader R,
Chlan-Fourney J, Suki D, Ahrar K, Rhines LD and Gokaslan ZL:
Percutaneous vertebroplasty and kyphoplasty for painful vertebral
body fractures in cancer patients. J Neurosurg. 98(Suppl): 21–30.
2003.PubMed/NCBI
|
|
31
|
Pflugmacher R, Schleicher P, Schröder RJ,
Melcher I and Klostermann CK: Maintained pain reduction in five
patients with multiple myeloma 12 months after treatment of the
involved cervical vertebrae with vertebroplasty. Acta Radiol.
47:823–829. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Eck JC, Nachtigall D, Humphreys SC and
Hodges SD: Comparison of vertebroplasty and balloon kyphoplasty for
treatment of vertebral compression fractures: A meta-analysis of
the literature. Spine J. 8:488–497. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Cotten A, Boutry N, Cortet B, Assaker R,
Demondion X, Leblond D, Chastanet P, Duquesnoy B and Deramond H:
Percutaneous vertebroplasty: State of the art. Radiographics.
18:311–323. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Deramond H, Depriester C, Galibert P and
Le Gars D: Percutaneous vertebroplasty with polymethylmethacrylate.
Technique, indications, and results. Radiol Clin North Am.
36:533–546. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
35
|
Garfin SR, Yuan HA and Reiley MA: New
technologies in spine: Kyphoplasty and vertebroplasty for the
treatment of painful osteoporotic compression fractures. Spine.
26:1511–1515. 2001. View Article : Google Scholar : PubMed/NCBI
|