Introduction
Abdominal drainage is widely used in abdominal
surgery for the rapid evacuation of post-operative fluid
collections. Gastric fistula, a common complication in
gastrointestinal surgery, usually occurs due to the failure of
anastomotic healing in gastrointestinal anastomosis and
reconstruction, or in the greater curvature of the stomach with a
direct injury to the gastric wall followed by splenectomy. The
incidence of gastric fistula and patient outcome are dependent on
surgery type (1) and
clinicopathological factors (2).
According to a recent meta-analysis, the incidence and mortality
rates following laparoscopic sleeve gastrectomy are ~2.2 and 0.11%,
respectively (3), whereas the
incidence is ~9.5% following gastrojejunostomy for the treatment of
gastric carcinoma (4). There are
various complications of gastric fistula, including abdominal pain,
painful bowel obstruction and fever. In clinical practice, the
diagnosis of gastric fistula is largely dependent on
gastroenterography. The majority of gastric fistula cases may be
treated by conservative therapy, including the administration of
drugs such as somatostatin, antibiotics and supportive care
(5). Certain cases may be treated
using the injection of fibrin sealant (6), however, surgery should be performed in
cases that have persisted for 120 days following diagnosis
(7). Generally, patient outcome is
good in patients with gastric fistula due to the administration of
timely therapy (8). Gastric fistula
secondary to the perforation by a drainage tube has rarely been
reported (9,10). In the present study, a case of gastric
fistula caused by misplacement of a drainage tube following a
splenectomy for abdominal trauma is reported.
Case report
A 54-year-old man was admitted to Shaoxing People's
Hospital (Shaoxing Hospital of Zhejiang University, Shaoxing,
Zhejiang, China) in April 2011 as an emergency due to injuries
sustained in an automobile accident. A physical examination
revealed tenderness over the left upper quadrant of the abdomen,
with a blood pressure of 80/50 mmHg (normal range, 90–140/60–90
mmHg). Abdominal ultrasonography indicated splenic rupture and
effusion in the peritoneal cavity. In the abdominocentesis, ~4 ml
bloody liquid was extracted. Thus, a closed abdominal injury and
abdominal hemorrhage was diagnosed. A laparotomy was performed in
the Department of Hepatobiliary Surgery, which revealed a
hemoperitoneum (2,000 ml) and splenic rupture. A splenectomy was
accomplished with no unexpected events and a rubber drainage tube
was placed in the splenic recess in proximity to the gastric
greater curvature.
The patient was placed on a semi-liquid diet on
post-operative day 4. The post-operative drainage volume gradually
decreased from 85 ml on post-operative day 1 to 35 ml on
post-operative day 6. On post-operative day 7, the patient
complained of slight discomfort and tenderness in the left upper
quadrant of the abdomen. In addition, ~50 ml of purulent fluid was
induced from the drainage tube. On post-operative day 9, 500 ml of
bile-colored fluid with small food particles was noted in the
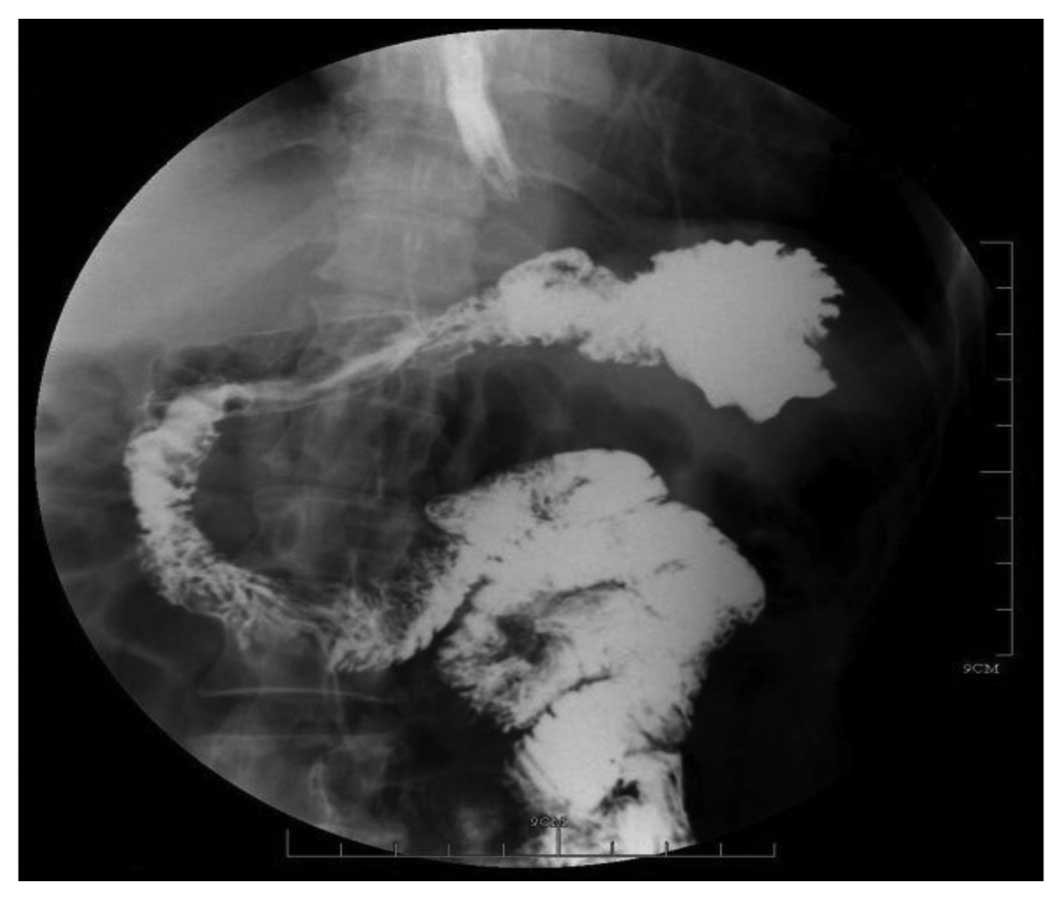
drainage tube. Barium X-ray (BLF-15B X-ray Beam Limiting Device;
Toshiba, Tokyo, Japan) revealed a gastric fistula in the upper
gastrointestinal tract (Fig. 1).
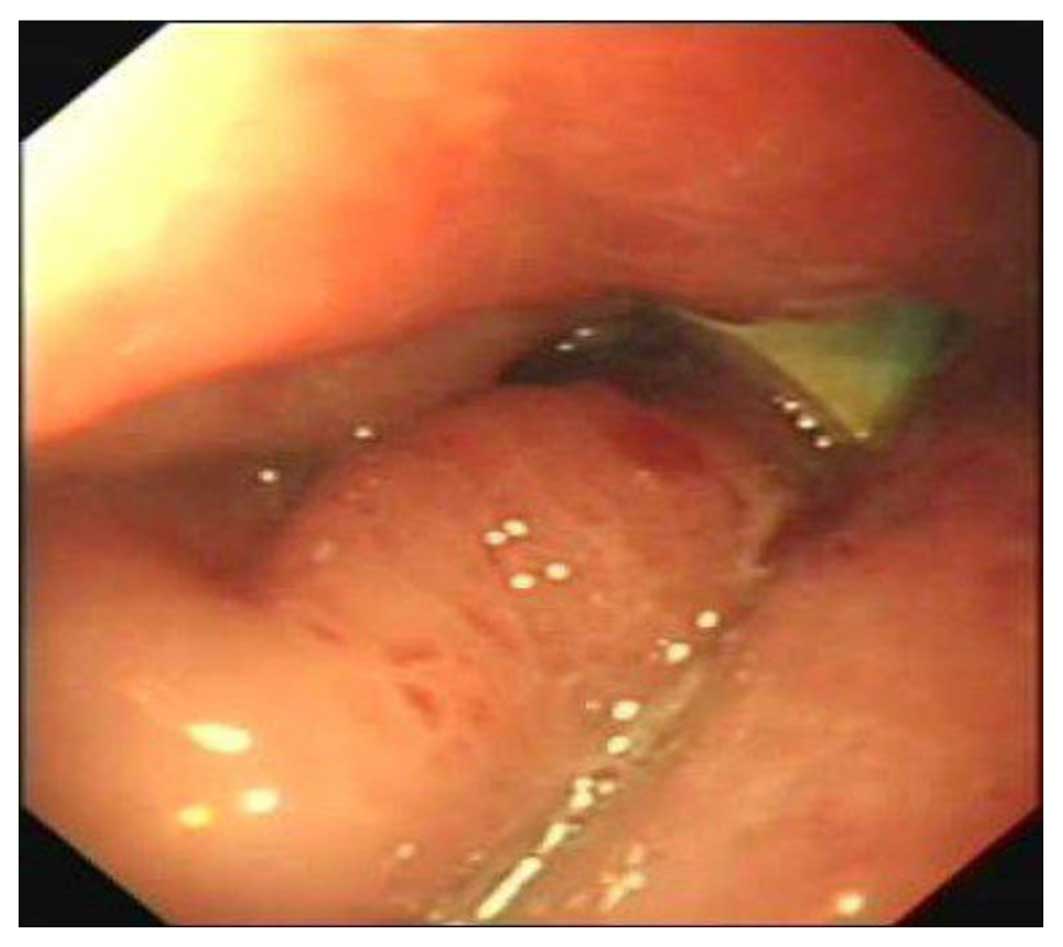
Gastroscopy (Evis Lucera CV-260SL; Olympus Corporation, Tokyo,
Japan) indicated infiltration of the drainage tube into the gastric
cavity (Fig. 2). No significant
peritoneal effusion was observed, as revealed by abdominal
ultrasound examination. The patient was consequently diagnosed with
a gastric fistula secondary to perforation by the drainage tube. As
a result, the drainage tube was withdrawn by 1 cm.
The patient was treated with somatostatin (6 mg/day
intravenously for a total of 21 days), total parenteral nutrition
and broad-spectrum antibiotics according to the general principles
of gastrointestinal fistula management (5). On post-operative day 36, the drainage
volume was decreased to 25 ml. Thus, the drainage tube was
subsequently withdrawn by 2 cm. No fluid was observed from the
drainage tube on post-operative day 39. Upper gastroenterography
(BLF-15B X-ray Beam Limiting Device) showed that the gastric
perforation was closed and the drainage tube was removed on
post-operative day 44 (Fig. 3). The
patient was discharged, and no complications were noted during the
2 years of follow-up. Written informed consent was obtained from
the patient for the publication of the present study.
Discussion
Drains are widely used in abdominal surgery in order
to remove any collections or secretions and to act as a warning of
hemorrhage or anastomotic leakage. The clinical complications of
drainage tubes are infrequent, but may include abdominal infection,
incisional herniation and prolapse of the abdominal contents
(11). Among these complications,
abdominal infection is most commonly noted. In addition, the threat
of erosion into certain adjacent tissues is the rarest complication
that may occur, with a risk of fistula development, particularly
when drains are placed near upper digestive anastomoses and sutures
(12). There have been a few reports
of visceral injury with intestinal perforation or peritonitis due
to suction drains that drew the bowel wall into the peripheral
holes, or due to pressure necrosis by the tip of the drain
(13,14).
Several studies on gastric fistulae following
splenectomy have been presented in the literature (15,16). The
condition was classically believed to be secondary to direct trauma
to the gastric wall from surgical instrumentation. In addition,
other induced factors, acting solely or in combination, may also
predispose patients to the development of post-splenectomy gastric
fistulae, including hematoma with an inflammatory reaction in the
gastrosplenic omentum, generalized arteriosclerotic disease and the
interruption of reflection of gastric muscle fibers into the
gastrosplenic ligament (17).
Notably, gastric penetration by drainage tube is extremely rare. In
2000, only one case presented with a gastrocutaneous fistula
following splenectomy, as a result of migration of the tube
subsequent to placement (9). To the
best of our knowledge, this is the second case of a patient who
sustained drainage tube penetration of the stomach subsequent to a
splenectomy.
The complication of a gastric fistula occurring due
to penetration by a drainage system is associated with a number of
factors, including the non-flexibility and stiffness of the drain
devices, edema at the site of surgical manipulation and pressure
necrosis of the stomach wall (18).
In the present case, the drainage tube showed good
biocompatibility, with a soft texture and superior elasticity. In
addition, the surgery was performed by experienced staff. The onset
of a gastric fistula caused by the erosion of the indwelling tube
suggested that the misplacement and/or long-term placement of
drains positioned close to the greater curvature of the stomach may
be the main causative factor. Ischemic necrosis of the stomach wall
occurred as a result of devascularization of the proximal stomach
artery due to the long period of in situ compression by the
tip of the drain. The gastric fistula was therefore induced with
further infiltration of the tube into the gastric cavity.
Although it is always necessary to monitor the
application of the drainage system, this precaution is of paramount
importance in certain situations. In colonic anastomosis, only a 5%
sensitivity for the detection of anastomotic leaks has been
recorded. On this basis, peritoneal drainage is not usually adopted
by surgeons (19). When drainage is
employed, it should be efficiently used and removed at the earliest
safe time following the surgery. Durai et al suggested that
it was relatively safe to remove a drainage tube if the drainage
flow was <25 ml within 24 h (20).
In addition, drains should be placed carefully to avoid direct
contact with the major blood vessels, organs and anastomoses, and
should be withdrawn and turned appropriately for a period of time
(20).
Usually, the complication of drainage penetration
with a fistula is treated using similar strategies to those for a
gastric fistula with absent peritonitis. In the few available
previous studies, patients have generally been treated
conservatively by withdrawing the drains from the perforation site
and permitting spontaneous healing of the fistula (9,18). In the
present case, the patient received somatostatin, total parenteral
nutrition and broad-spectrum antibiotics, and recovered
uneventfully. On the evidence currently available, conservative
management may be feasible for patients without any signs of
peritonitis, and the appropriate withdrawal of the drain from the
perforation site is a prerequisite to ensure the success of this
treatment strategy.
In conclusion, few cases of a gastric fistula
secondary to perforation by a drainage tube have been reported. The
present study describes one case of a gastric fistula that was
caused by improper use of a drainage tube following a splenectomy
for abdominal trauma. Following conservative treatment, the patient
was discharged with a satisfactory outcome.
References
|
1
|
Smith MD, Adeniji A, Wahed AS, Patterson
E, Chapman W, Courcoulas AP, Dakin G, Flum D, McCloskey C, Mitchell
JE, et al: Technical factors associated with anastomotic leak after
Roux-en-Y gastric bypass. Surg Obes Relat Dis. 11:313–320. 2015.
View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Kim SH, Son SY, Park YS, Ahn SH, Do Park J
and Kim HH: Risk factors for anastomotic leakage: A retrospective
cohort study in a single gastric surgical unit. J Gastric Cancer.
15:167–175. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Parikh M, Issa R, McCrillis A, Saunders
JK, Ude-Welcome A and Gagner M: Surgical strategies that may
decrease leak after laparoscopic sleeve gastrectomy: A systematic
review and meta-analysis of 9991 cases. Ann Surg. 257:231–237.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Liu BW, Liu Y, Liu JR and Feng ZX:
Comparison of hand-sewn and stapled anastomoses in surgeries of
gastrointestinal tumors based on clinical practice of China. World
J Surg Oncol. 12:2922014. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Foster CE III and Lefor AT: General
management of gastrointestinal fistulas. Recognition, stabilization
and correction of fluid and electrolyte imbalances. Surg Clin North
Am. 76:1019–1033. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Kowalski C, Kastuar S, Mehta V and Brolin
RE: Endoscopic injection of fibrin sealant in repair of
gastrojejunostomy leak after laparoscopic Roux-en-Y gastric bypass.
Surg Obes Relat Dis. 3:438–442. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Rebibo L, Bartoli E, Dhahri A, Cosse C,
Robert B, Brazier F, Pequignot A, Hakim S, Yzet T, Delcenserie R,
et al: Persistent gastric fistula after sleeve gastrectomy: An
analysis of the time between discovery and reoperation. Surg Obes
Relat Dis. 12:84–93. 2016. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jacobsen HJ, Nergard BJ, Leifsson BG,
Frederiksen SG, Agajahni E, Ekelund M, Hedenbro J and Gislason H:
Management of suspected anastomotic leak after bariatric
laparoscopic Roux-en-y gastric bypass. Br J Surg. 101:417–423.
2014. View
Article : Google Scholar : PubMed/NCBI
|
|
9
|
Paraskevopoulos JA, Samoilis S, Papadakis
G, Kostopoulos O and Kalimeris S: Drainage tube perforation of the
stomach: An exceptionally rare complication. J Trauma. 48:330–331.
2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Rege S, Narlawar R, Deshpande A and Dalvi
A: Iatrogenic gastric fistula due to inappropriate placement of
intercostal drainage tube in a case of traumatic diaphragmatic
hernia. J Postgrad Med. 47:108–110. 2001.PubMed/NCBI
|
|
11
|
Kjossev KT and Losanoff JE: Complication
of prophylactic intraperitoneal drainage. Dig Dis Sci. 46:24562001.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
González-Pinto I and González EM:
Optimising the treatment of upper gastrointestinal fistulae. Gut.
49(Suppl 4): iv22–iv31. 2001.PubMed/NCBI
|
|
13
|
Nomura T, Shirai Y, Okamoto H and
Hatakeyama K: Bowel perforation caused by silicone drains: A report
of two cases. Surg Today. 28:940–942. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nikolić M, Karthikesalingam A, Nachimuthu
S, Tang TY and Harris AM: Biliary peritonitis caused by a leaking
T-tube fistula disconnected at the point of contact with the
anterior abdominal wall: A case report. J Med Case Rep. 2:3022008.
View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Zheng X, Yao Y and Liu Q: Gastric
perforation after laparoscopic splenectomy and esophagogastric
devascularization for portal hypertension: Report of a case. Surg
Laparosc Endosc Percutan Tech. 21:e209–e212. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Martinez CA, Waisberg J, Palma RT,
Bromberg SH, Castro MA and Santos PA: Gastric necrosis and
perforation as a complication of splenectomy. Case report and
related references. Arq Gastroenterol. 37:227–230. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Harrison B, Glanges E and Sparkman RS:
Gastric fistula following splenectomy: Its cause and prevention.
Ann Surg. 185:210–213. 1977. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Eleftheriadis E: Drainage-tube penetration
into the gastric lumen, mimicking a high-volume enterocutaneous
fistula. The significance of postoperative endoscopy. Surg Endosc.
4:184–185. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Puleo FJ, Mishra N and Hall JF: Use of
intra-abdominal drains. Clin Colon Rectal Surg. 26:174–177. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Durai R, Mownah A and Ng P: Use of drains
in surgery: A review. J Perioper Pract. 19:180–186. 2009.PubMed/NCBI
|