|
1
|
Jemal A, Siegel R, Ward E, Murray T, Xu J
and Thun MJ: Cancer statistics, 2007. CA Cancer J Clin. 57:43–66.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Parkin DM, Bray F, Ferlay J and Pisani P:
Global cancer statistics, 2002. CA Cancer J Clin. 55:74–108. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Partridge EE and Barnes MN: Epithelial
ovarian cancer: Prevention, diagnosis, and treatment. CA Cancer J
Clin. 49:297–320. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Harries M and Gore M: Part. I Chemotherapy
for epithelial ovarian cancer-treatment at first diagnosis. Lancet
Oncol. 3:529–536. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Petrelli F, Zaniboni A, Coinu A, Cabiddu
M, Ghilardi M, Sgroi G and Barni S: Cisplatin or not in advanced
gastric cancer: A systematic review and meta-analysis. PLoS One.
8:e830222013. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Tan S, Peng X, Peng W, Zhao Y and Wei Y:
Enhancement of oxaliplatin-induced cell apoptosis and tumor
suppression by 3-methyladenine in colon cancer. Oncol Lett.
9:2056–2062. 2015.PubMed/NCBI
|
|
7
|
Kweekel DM, Gelderblom H and Guchelaar HJ:
Pharmacology of oxaliplatin and the use of pharmacogenomics to
individualize therapy. Cancer Treat Rev. 31:90–105. 2005.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Jun L, Haiping Z and Beibei Y: Genetic
polymorphisms of GSTP1 related to response to
5-FU-oxaliplatin-based chemotherapy and clinical outcome in
advanced colorectal cancer patients. Swiss Med Wkly. 139:724–728.
2009.PubMed/NCBI
|
|
9
|
Shim HJ, Yun JY, Hwang JE, Bae WK, Cho SH,
Lee JH, Kim HN, Shin MH, Kweon SS, Lee JH, et al: BRCA1 and XRCC1
polymorphisms associated with survival in advanced gastric cancer
treated with taxane and cisplatin. Cancer Sci. 101:1247–1254. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Yan H, Jia H, Gao H, Guo X and Xu B:
Identification, genomic organization, and oxidative stress response
of a sigma class glutathione S-transferase gene (AccGSTS1) in the
honey bee, Apis cerana cerana. Cell Stress Chaperones.
18:415–426. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Vontas JG, Small GJ and Hemingway J:
Glutathione S-transferases as antioxidant defence agents confer
pyrethroid resistance in Nilaparvata lugens. Biochem J.
357:65–72. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Hayes JD and Pulford DJ: The glutathione
S-transferase supergene family: Regulation of GST and the
contribution of the isoenzymes to cancer chemoprotection and drug
resistance. Crit Rev Biochem Mol Biol. 30:445–600. 1995. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Chan EC, Lam SY, Fu KH and Kwong YL:
Polymorphisms of the GSTM1, GSTP1, MPO, XRCC1 and NQO1 genes in
Chinese patients with non-small cell lung cancers: Relationship
with aberrant promoter methylation of the CDKN2A and RARB genes.
Cancer Genet Cytogenet. 162:10–20. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Ye F, Liu Z, Tan A, Liao M, Mo Z and Yang
X: XRCC1 and GSTP1 polymorphisms and prognosis of oxaliplatin-based
chemotherapy in colorectal cancer: A meta-analysis. Cancer
Chemother Pharmacol. 71:733–740. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Economopoulos KP and Sergentanis TN:
GSTM1, GSTT1, GSTP1, GSTA1 and colorectal cancer risk: A
comprehensive meta-analysis. Eur J Cancer. 46:1617–1631. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Funke S, Timofeeva M, Risch A, Hoffmeister
M, Stegmaier C, Seiler CM, Brenner H and Chang-Claude J: Genetic
polymorphisms in GST genes and survival of colorectal cancer
patients treated with chemotherapy. Pharmacogenomics. 11:33–41.
2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zaanan A, Dalban C, Emile JF, Blons H,
Fléjou JF, Goumard C, Istanbullu M, Calmel C, Alhazmi K, Validire
P, et al: ERCC1, XRCC1 and GSTP1 single nucleotide polymorphisms
and survival of patients with colon cancer receiving
oxaliplatin-based adjuvant chemotherapy. J Cancer. 5:425–432. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
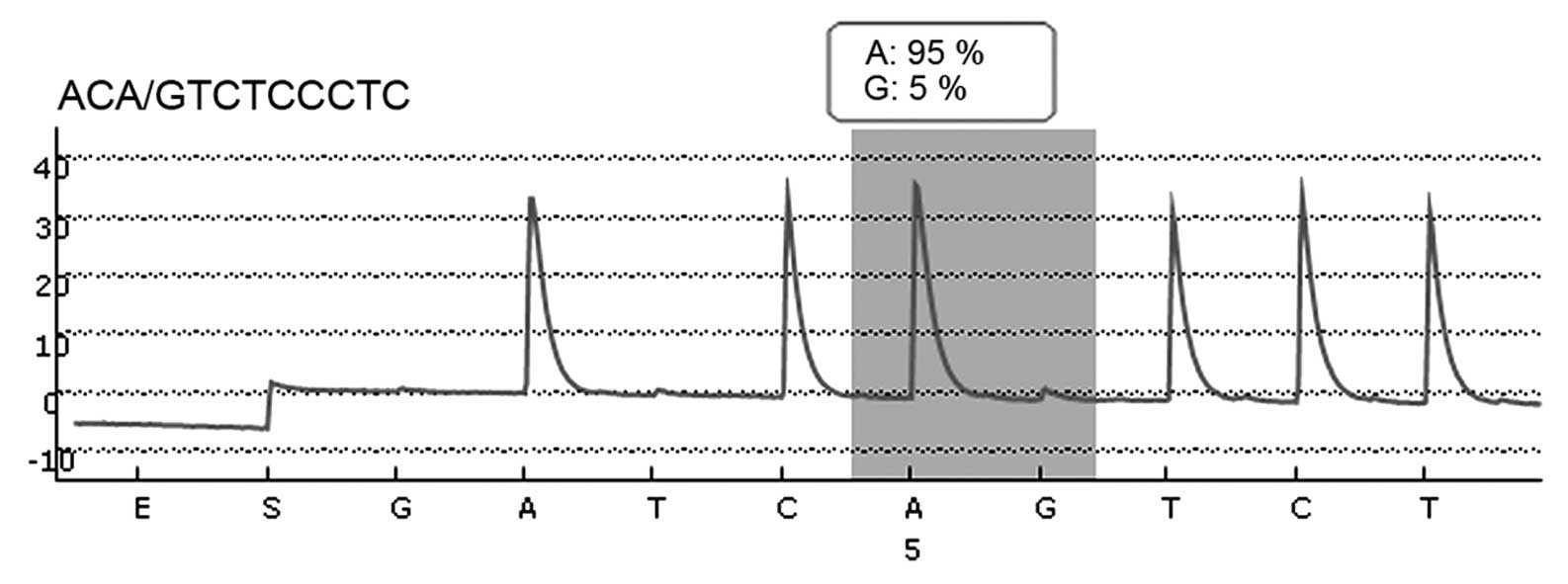
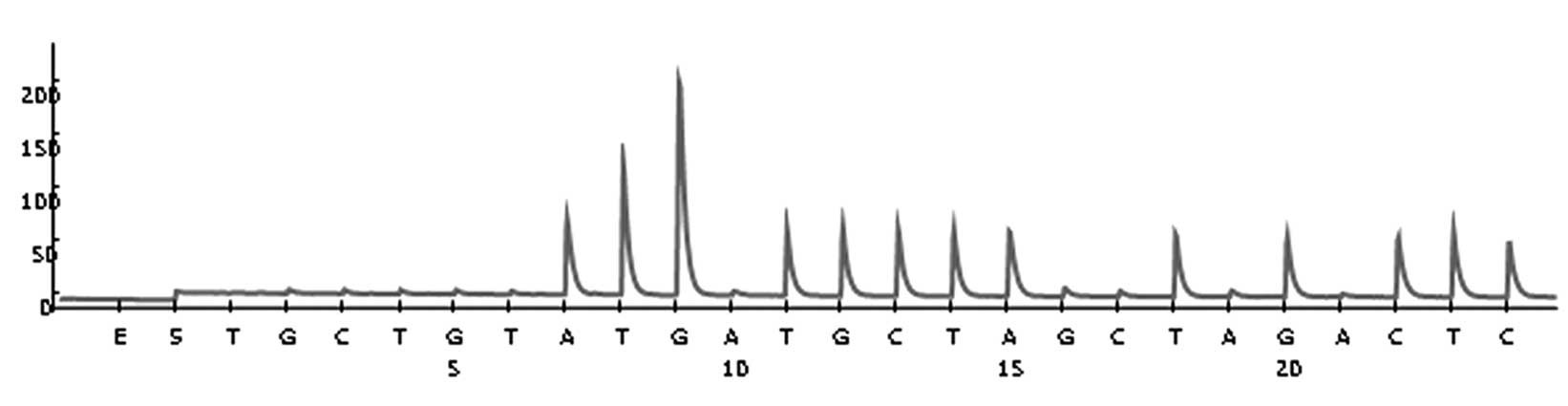
Marsh S, King CR, Garsa AA and McLeod HL:
Pyrosequencing of clinically relevant polymorphisms. Methods Mol
Biol. 311:97–114. 2005.PubMed/NCBI
|
|
19
|
Butkiewicz D, Rusin M, Sikora B, Lach A
and Chorąży M: An association between DNA repair gene polymorphisms
and survival in patients with resected non-small cell lung cancer.
Mol Biol Rep. 38:5231–5241. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Kizys MM, Cardoso MG, Lindsey SC, Harada
MY, Soares FA, Melo MC, Montoya MZ, Kasamatsu TS, Kunii IS,
Giannocco G, et al: Optimizing nucleic acid extraction from thyroid
fine-needle aspiration cells in stained slides,
formalin-fixed/paraffin-embedded tissues, and long-term stored
blood samples. Arq Bras Endocrinol Metabol. 56:618–626. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Chai H, Pan J, Zhang X, Zhang X, Shen X,
Li H, Zhang K, Yang C, Sheng H and Gao H: ERCC1 C118T associates
with response to FOLFOX4 chemotherapy in colorectal cancer patients
in Han Chinese. Int J Clin Exp Med. 5:186–194. 2012.PubMed/NCBI
|
|
22
|
Chen YC, Tzeng CH, Chen PM, Lin JK, Lin
TC, Chen WS, Jiang JK, Wang HS and Wang WS: Influence of GSTP1
I105V polymorphism on cumulative neuropathy and outcome of FOLFOX-4
treatment in Asian patients with colorectal carcinoma. Cancer Sci.
101:530–535. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Lv H, Li Q, Qiu W, Xiang J, Wei H, Liang
H, Sui A and Liang J: Genetic polymorphism of XRCC1 correlated with
response to oxaliplatin-based chemotherapy in advanced colorectal
cancer. Pathol Oncol Res. 18:1009–1014. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Ali-Osman F, Akande O, Antoun G, Mao JX
and Buolamwini J: Molecular cloning, characterization and
expression in Escherichia coli of full-length cDNAs of three
human glutathione S-transferase Pi gene variants. Evidence for
differential catalytic activity of the encoded proteins. J Biol
Chem. 272:10004–10012. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Godschalk RW, Dallinga JW, Wikman H, Risch
A, Kleinjans JC, Bartsch H and Van Schooten FJ: Modulation of DNA
and protein adducts in smokers by genetic polymorphisms in GSTM1,
GSTT1, NAT1 and NAT2. Pharmacogenetics. 11:389–398. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Gertig DM, Stampfer M, Haiman C, Hennekens
CH, Kelsey K and Hunter DJ: Glutathione S-transferase GSTM1 and
GSTT1 polymorphisms and colorectal cancer risk: A prospective
study. Cancer Epidemiol Biomarkers Prev. 7:1001–1005.
1998.PubMed/NCBI
|
|
27
|
Slattery ML, Potter JD, Samowitz W, Bigler
J, Caan B and Leppert M: NAT2, GSTM-1, cigarette smoking, and risk
of colon cancer. Cancer Epidemiol Biomarkers Prev. 7:1079–1084.
1998.PubMed/NCBI
|
|
28
|
Li QF, Yao RY, Liu KW, Lv HY, Jiang T and
Liang J: Genetic polymorphism of GSTP1: Prediction of clinical
outcome to oxaliplatin/5-FU-based chemotherapy in advanced gastric
cancer. J Korean Med Sci. 25:846–852. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Hong J, Han SW, Ham HS and Kim TY, Choi
IS, Kim BS, Oh DY, Im SA, Kang GH, Bang YJ and Kim TY: Phase II
study of biweekly S-1 and oxaliplatin combination chemotherapy in
metastatic colorectal cancer and pharmacogenetic analysis. Cancer
Chemother Pharmacol. 67:1323–1331. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Watson MA, Stewart RK, Smith GB, Massey TE
and Bell DA: Human glutathione S-transferase P1 polymorphisms:
Relationship to lung tissue enzyme activity and population
frequency distribution. Carcinogenesis. 19:275–280. 1998.
View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Stoehlmacher J, Park DJ, Zhang W, Groshen
S, Tsao-Wei DD, Yu MC and Lenz HJ: Association between glutathione
S-transferase P1, T1, and M1 genetic polymorphism and survival of
patients with metastatic colorectal cancer. J Natl Cancer Inst.
94:936–942. 2002. View Article : Google Scholar : PubMed/NCBI
|
|
32
|
Townsend DM and Tew KD: The role of
glutathione-S-transferase in anti-cancer drug resistance. Oncogene.
22:7369–7375. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
33
|
Huang MY, Huang ML, Chen MJ, Lu CY, Chen
CF, Tsai PC, Chuang SC, Hou MF, Lin SR and Wang JY: Multiple
genetic polymorphisms in the prediction of clinical outcome of
metastatic colorectal cancer patients treated with first-line
FOLFOX-4 chemotherapy. Pharmacogenet Genomics. 21:18–25. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
34
|
Suh KW, Kim JH, Kim DY, Kim YB, Lee C and
Choi S: Which gene is a dominant predictor of response during
FOLFOX chemotherapy for the treatment of metastatic colorectal
cancer, the MTHFR or XRCC1 gene? Ann Surg Oncol. 13:1379–1385.
2006. View Article : Google Scholar : PubMed/NCBI
|