Introduction
Fluorouracil (FU)-based adjuvant chemotherapy was
the standard treatment in patients with stage III colon cancer
until ~25 years ago (1). Oxaliplatin
has since emerged as an important drug for adjuvant treatment based
on clinical data, as it demonstrates significant activity in
metastatic colon cancer. The Multicenter International Study of
Oxaliplatin/5-FU/Leucovorin in the Adjuvant Treatment of Colon
Cancer trial indicated that adding oxaliplatin to infusional FU
plus leucovorin significantly increased disease-free survival and
overall survival rates (2). A
combination of oxaliplatin and capecitabine is another adjuvant
treatment option; therefore, oxaliplatin-based chemotherapy has
become popular for the adjuvant treatment of colon cancer (3). Unfortunately, oxaliplatin may cause
liver injury, including sinusoidal obstruction syndrome (SOS). SOS
may present as reticular hypointensity on hepatobiliary phase
images of gadoxetic acid-enhanced magnetic resonance images
(EOB-MRI), but does not usually present with focal lesions
(4). The present study describes a
case of oxaliplatin-induced SOS mimicking metastatic colon cancer
in the liver. The lesions were not differentiated from metastasis
via imaging and surgery was performed. Written informed consent was
obtained from the patient.
Case report
A 22-year-old woman, who had undergone a
laparoscopic right hemicolectomy for ascending colon cancer 4
months prior, presented to Hanyang University Guri Hospital (Guri,
South Korea) for the 5th cycle of adjuvant chemotherapy in November
2014. The pathological diagnosis of the ascending colon cancer was
stage pT4aN1aM0 moderately-differentiated tubular adenocarcinoma.
The patient was treated with oxaliplatin-based adjuvant
chemotherapy, consisting of 130 mg/m2 oxaliplatin on day
1 and 1,000 mg/m2 capecitabine twice daily on days 1–14
every 3 weeks (XELOX).
Prior to the fifth cycle of XELOX, the patient
exhibited no abnormal signs or symptoms. Laboratory tests revealed
a hemoglobin level of 11.8 g/dl (normal range, 12.0–16.0 g/dl), a
white blood cell count of 3,800 cells/µl (normal range,
4,000–10,000 cells/µl), a platelet count of 112,000 platelets/µl
(normal range, 150,000-400,000 platelets/µl), total bilirubin level
of 0.6 g/dl (normal range, 0.4–1.5 g/dl), alkaline phosphatase
level of 105 IU/l (normal range, 35–95 IU/l), alanine
aminotransferase concentration of 51 IU/l (normal range, 10–45
IU/l), aspartate aminotransferase concentration of 47 IU/l (normal
range, 15–45 IU/l), and normal results for kidney function tests.
The carcinoembryonic antigen was within the normal range (3.94
ng/ml; normal range, 0.1–5.0 ng/ml), and the results of the
serological tests revealed that the patient was not infected with
hepatitis B or C virus.
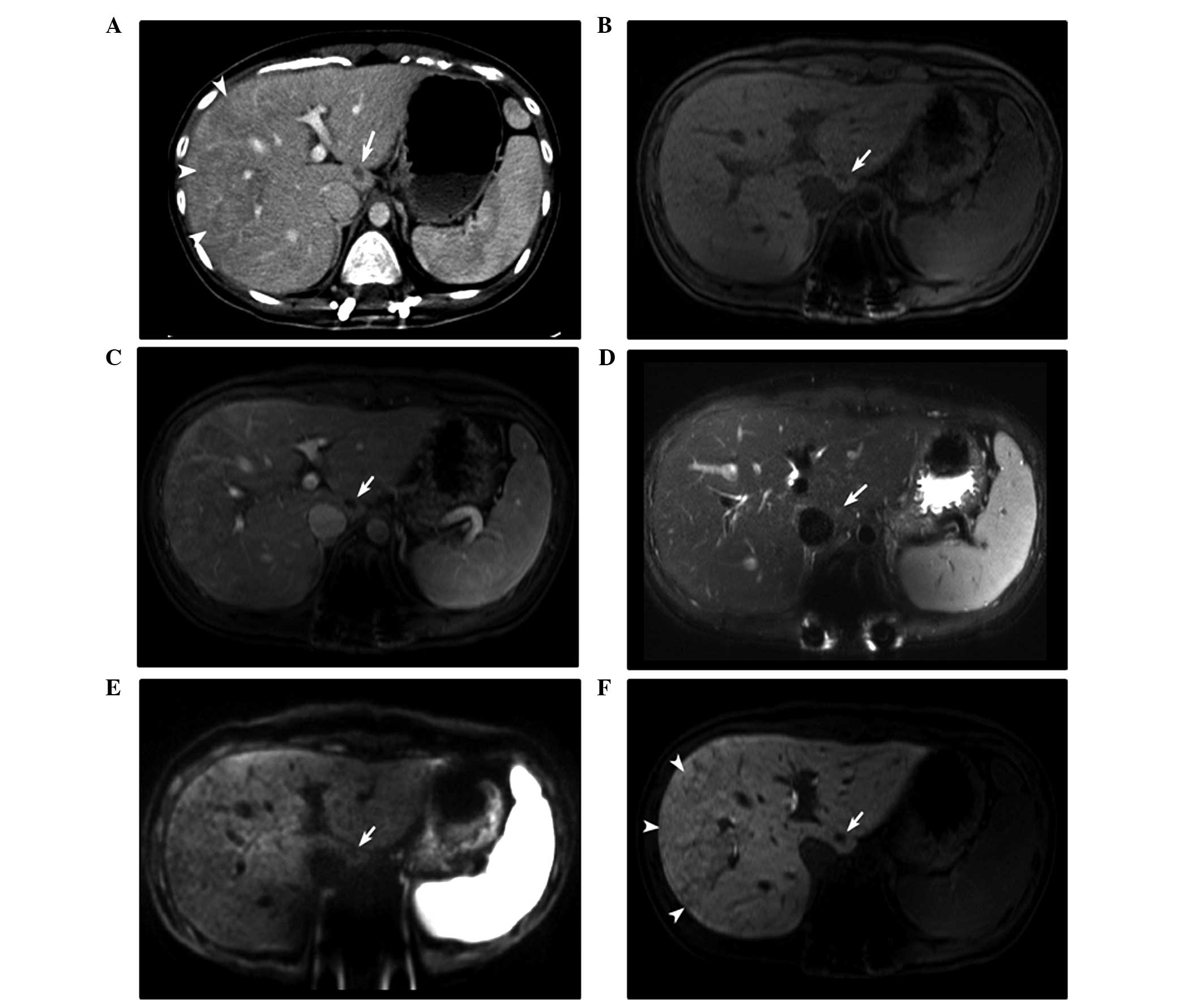
The contrast-enhanced abdominal computed tomography
(CT) scan revealed a novel tiny, nodular, low-density lesion in
segment 1 of the liver. EOB-MRI identified that the lesion was 1 cm
in size at the widest point, ovoid and hypointense on the
pre-contrast and portal-phase T1-weighted imaging, without
enhancement. EOB-MRI revealed partial hyperintensity on the
T2-weighted imaging and a hypointense nodule on diffusion-weighted
imaging (Fig. 1). Positron emission
tomography (PET)-CT identified no clear abnormal fluorodeoxyglucose
(FDG) uptake suggestive of malignancy. Although the findings did
not exclude a metastatic lesion, adjuvant chemotherapy [oxaliplatin
(190 mg, day 1) and capecitabine (1,500 mg, twice daily, days 1–14)
every 3 weeks] was administered, with a follow-up abdominal CT
performed one month later.
Abdominal CT following the fifth round of
chemotherapy revealed that the lesion was more discrete and
slightly enlarged. Hepatobiliary ultrasonography revealed a 1.4–cm
mixed echoic lesion in segment 1 and mild splenomegaly (12.3 cm;
prior to chemotherapy, 11 cm). Due to the changes observed in the
lesion, a surgical resection was planned.
The patient underwent isolated caudate lobectomy of
the liver. The liver was exposed through an inverted T incision.
Following the cholecystectomy, the falciform ligament was divided
and a liver mobilization was performed. A tumor was not visible or
palpable upon gross observation of the caudate lobe. Intraoperative
ultrasonography revealed a 1.5–cm lesion in the caudate lobe. The
adjacent liver parenchyma was normal. For the isolated caudate
lobectomy, the hanging maneuver was applied (5).
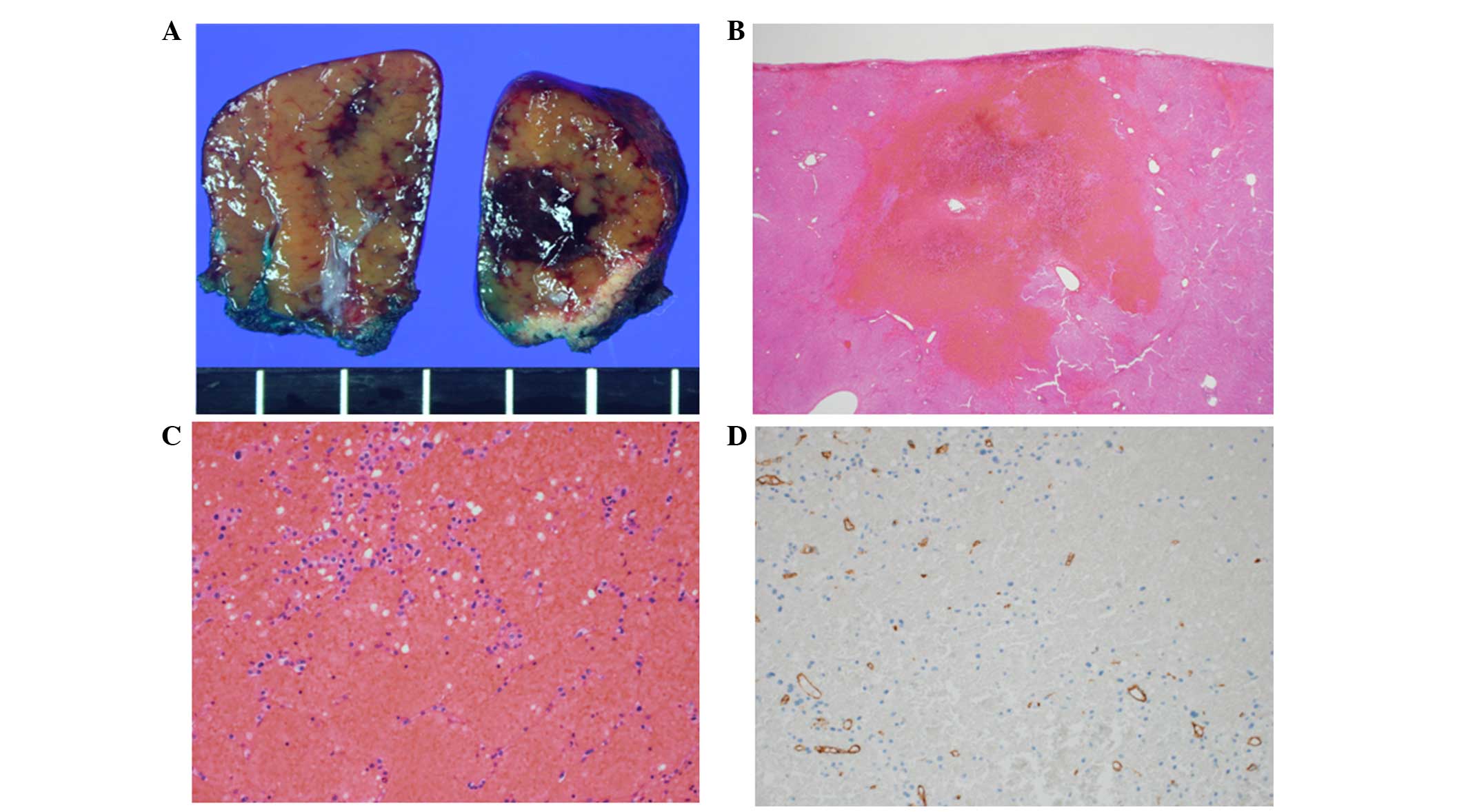
Macroscopically, an ill-defined, dark, red,
congested lesion with a soft consistency measuring 1.4×1.0 cm on
the cross-section was identified in the resected caudate lobe of
the liver. The lesion identified was considered to be the same
lesion that had indicated malignancy on the radiological studies.
The adjacent parenchyma also demonstrated diffuse sinusoidal
congestion and had a nutmeg-like appearance (Fig. 2A). Microscopically, the lesion
exhibited severe sinusoidal dilation with congestion. The widened
sinusoidal space was outlined by markedly attenuated hepatic cords
and filled with erythrocytes. An immunohistochemical study of
cluster of differentiation 34 revealed a decrease in sinusoidal
endothelial cells in this lesion (Fig.
2B–2D). The final diagnosis was oxaliplatin-induced SOS.
The patient had an uneventful post-operative course
and recovered completely. Since the SOS was revealed histologically
in the lesion and the surrounding liver tissue, administration of
XELOX was discontinued. The patient remained relapse-free for three
months following the lobectomy.
Discussion
Oxaliplatin, a third-generation platinum analog, is
an effective chemotherapeutic agent for numerous solid tumors when
combined with other drugs, including colorectal and stomach cancer.
Since the first clinical study that demonstrated severe hepatic
sinusoidal obstruction induced by oxaliplatin in 2004 (6), oxaliplatin-induced hepatic injury has
become a major concern in patients that receive hepatic resection
for metastatic colorectal cancer. Oxaliplatin-induced hepatic
injury often manifests as SOS. SOS, previously termed
veno-occlusive disease or blue liver syndrome, is characterized by
the discontinuity of the sinusoidal membrane, collagenization of
the perisinusoidal space and sinusoidal dilatations with
erythrocyte congestion in centrilobular zones due to damage to the
sinusoidal endothelial cells (6–8).
The majority of oxaliplatin-induced SOS data are
obtained by reviewing post-chemotherapy liver resection specimens
obtained from patients with colorectal liver metastases that
received preoperative chemotherapy (6,8,9). The patient in the present study
developed a hepatic lesion during adjuvant chemotherapy. The lesion
was not differentiated from metastasis despite the use of several
imaging tools. Although the hepatic lesion demonstrated no abnormal
FDG uptake on the PET-CT and no abnormalities on the
diffusion-restriction MRI, the lesion had increased in size one
month later. Due to this finding, the possibility of metastasis was
considered first. A biopsy of the lesion was initially planned;
however, due to the risk of complications from the biopsy and, if
the lesion was metastatic, a lobectomy was performed without a
biopsy.
To the best of our knowledge, there have previously
only been two reported cases of SOS mimicking a metastatic tumor on
imaging that are similar to the present study (10,11). The
two previous studies described patients that had developed several
novel hepatic lesions during adjuvant oxaliplatin-based
chemotherapy, including FOLFOX6, which consists of oxaliplatin with
FU and folinic acid, and XELOX (10,11). These
previous studies did not consider the possibility of non-malignant
lesions prior to performing the lobectomy.
Although oxaliplatin-induced SOS is usually
asymptomatic, it may be associated with an increased perioperative
morbidity and bleeding risk (9).
Therefore, there have been several studies that investigated the
predictive parameters for oxaliplatin-induced SOS, such as EOB-MRI
findings, the volume of the spleen, the levels of hyaluronic acid,
the indocyanine green retention rate at 15 min (ICG-R15), and
aspartate aminotransferase (AST) level (8,9,12). Shin et al (4) reported that reticular hypointensity on
hepatobiliary phase images of EOB-MRI was highly specific for SOS.
Shin et al divided the presence of reticular hypointensity
into 5 levels, and levels 4 and 5 were considered to indicate SOS
(4). In the present study, transverse
contrast-enhanced CT imaging revealed diffuse, poorly enhanced
regions on the right lobe of the liver, and EOB-MRI revealed
confidence level 4 reticular hypointensity on the hepatobiliary
phase images in the same region (Fig.
1F). In addition, the AST levels (54 IU/l) and ICG-R15 (12.25%)
were increased prior to surgery. The findings suggested a diagnosis
of oxaliplatin-induced SOS in the background liver. However, during
the initial evaluation, only the focal lesion in segment 1 was
focused on, making the diagnosis of SOS prior to surgery extremely
challenging.
In summary, the present study reports the case of a
patient with oxaliplatin-induced SOS that mimicked metastatic colon
cancer in the liver on imaging studies. Therefore, SOS may be
considered one of the causes of newly developed hepatic lesions in
patients with colon cancer that receive oxaliplatin-based
chemotherapy, particularly if the patients possess predictive
findings for oxaliplatin-induced SOS and the lesions do not
demonstrate the uptake of FDG on the PET-CT.
References
|
1
|
Moertel CG, Fleming TR, Macdonald JS,
Haller DG, Laurie JA, Goodman PJ, Ungerleider JS, Emerson WA,
Tormey DC, Glick JH, et al: Levamisole and fluorouracil for
adjuvant therapy of resected colon carcinoma. N Engl J Med.
322:352–358. 1990. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
André T, Boni C, Navarro M, Tabernero J,
Hickish T, Topham C, Bonetti A, Clingan P, Bridgewater J, Rivera F
and de Gramont A: Improved overall survival with oxaliplatin,
fluorouracil, and leucovorin as adjuvant treatment in stage II or
III colon cancer in the MOSAIC trial. J Clin Oncol. 27:3109–3116.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Haller DG, Tabernero J, Maroun J, de Braud
F, Price T, Van Cutsem E, Hill M, Gilberg F, Rittweger K and
Schmoll HJ: Capecitabine plus oxaliplatin compared with
fluorouracil and folinic acid as adjuvant therapy for stage III
colon cancer. J Clin Oncol. 29:1465–1471. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Shin NY, Kim MJ, Lim JS, Park MS, Chung
YE, Choi JY, Kim KW and Park YN: Accuracy of gadoxetic
acid-enhanced magnetic resonance imaging for the diagnosis of
sinusoidal obstruction syndrome in patients with
chemotherapy-treated colorectal liver metastases. Eur Radiol.
22:864–871. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Kim SH, Park SJ, Lee SA, Lee WJ, Park JW
and Kim CM: Isolated caudate lobectomy using the hanging maneuver.
Surgery. 139:847–850. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Rubbia-Brandt L, Audard V, Sartoretti P,
Roth AD, Brezault C, Le Charpentier M, Dousset B, Morel P, Soubrane
O, Chaussade S, et al: Severe hepatic sinusoidal obstruction
associated with oxaliplatin-based chemotherapy in patients with
metastatic colorectal cancer. Ann Oncol. 15:460–466. 2004.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
DeLeve LD, Shulman HM and McDonald GB:
Toxic injury to hepatic sinusoids: Sinusoidal obstruction syndrome
(veno-occlusive disease). Semin Liver Dis. 22:27–42. 2002.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Morine Y, Shimada M and Utsunomiya T:
Evaluation and management of hepatic injury induced by
oxaliplatin-based chemotherapy in patients with hepatic resection
for colorectal liver metastasis. Hepatol Res. 44:59–69. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Aloia T, Sebagh M, Plasse M, Karam V, Lévi
F, Giacchetti S, Azoulay D, Bismuth H, Castaing D and Adam R: Liver
histology and surgical outcomes after preoperative chemotherapy
with fluorouracil plus oxaliplatin in colorectal cancer liver
metastases. J Clin Oncol. 24:4983–4990. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Arakawa Y, Shimada M, Utsunomya T, Imura
S, Morine Y, Ikemoto T, Hanaoka J, Sugimoto K and Bando Y:
Oxaliplatin-related sinusoidal obstruction syndrome mimicking
metastatic liver tumors. Hepatol Res. 43:685–689. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Uchino K, Fujisawa M, Watanabe T, Endo Y,
Nobuhisa T, Matsumoto Y, Kai K, Sato S, Notohara K and Matsukawa A:
Oxaliplatin-induced liver injury mimicking metastatic tumor on
images: A case report. Jpn J Clin Oncol. 43:1034–1038. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
12
|
van den Broek MA, Vreuls CP, Winstanley A,
Jansen RL, van Bijnen AA, Dello SA, Bemelmans MH, Dejong CH,
Driessen A and Olde Damink SW: Hyaluronic acid as a marker of
hepatic sinusoidal obstruction syndrome secondary to
oxaliplatin-based chemotherapy in patients with colorectal liver
metastases. Ann Surg Oncol. 20:1462–1469. 2013. View Article : Google Scholar : PubMed/NCBI
|