Introduction
Gastric cancer is one of the most widespread
malignant tumors in the world. According to the latest world cancer
statistics, 700,000 patients succumbed due to gastric cancer in
2012, making it the third most common cause of cancer mortality
(1). In 2005, 300,000 mortalities and
400,000 new cases of gastric cancer were reported in China
(2). Metastasis from gastric cancer
typically occurs in the abdominal cavity, peritoneum, lymph nodes
and liver (3). Metastasis limited to
the brain is rare and prognosis in such cases is poor (4,5). It has
been reported in <1% of clinical cases, the majority of which
are included in 2 large, single-institution retrospective studies.
Between 1957 and 1997, a total of 3320 patients were diagnosed with
gastric cancer at M.D. Anderson Cancer Center (Houston, TX, USA),
and only 24 of these patients (0.7%) were observed to have brain
metastases following imaging studies or autopsy. The median
survival time was ~9 weeks, and in certain patients surgical
resection followed by whole-brain radiation therapy was associated
with relatively long survival times of 54 weeks (5). Another study identified brain metastasis
in only 11 out of 2322 patients (0.47%) treated between 1980 and
1998 (6). York et al (5) noted neurological improvement in only 4
out of 24 patients (16.7%) treated with either surgical resection
with whole brain radiation therapy (WBRT) (n=3) or WBRT alone
(n=1). The median survival time among the WBRT group did not differ
from patients that had received steroid monotherapy. Kaskura et
al (4) reported a median survival
time of 24.0 weeks in patients that had undergone surgery or
surgery with WBRT compared with 10.8 weeks in patients that
received WBRT alone. To the best of our knowledge, there have been
no prior reports of solitary brain metastasis from gastric cancer
with peripheral nervous system symptoms (7–10). The
current study presents a rare case of gastric cancer with brain
metastasis and nervous system symptoms treated with stereotactic
radiotherapy.
Case report
A 60-year old male patient presenting with nausea,
vomiting and epigastric pain for 10 days and was admitted to
Shanghai Changhai Hospital affiliated to the Second Military
Medical University (Shanghai, China) on November 8, 2012. The
patient ate a balanced diet without previous history of peptic
ulcer or other gastrointestinal disorders and no family medical
history of gastric cancer. Physical examination revealed no
abnormalities. Laboratory examinations identified positive
carcinoembryonic antigen (CEA) at 310.23 ng/ml (normal range,
<0.5 ng/ml); all other laboratory examinations were negative.
Gastric endoscopy revealed a protruding tumor measuring 3.0×2.5 cm
on the anterior wall of the fundus of the stomach. An enhanced
computed tomography (CT; Brilliance 16; Philips Medical Systems,
Inc., Bothell, WA, USA) scan confirmed a gastric antrum tumor. A
distal gastrectomy was performed on the patient on November 13,
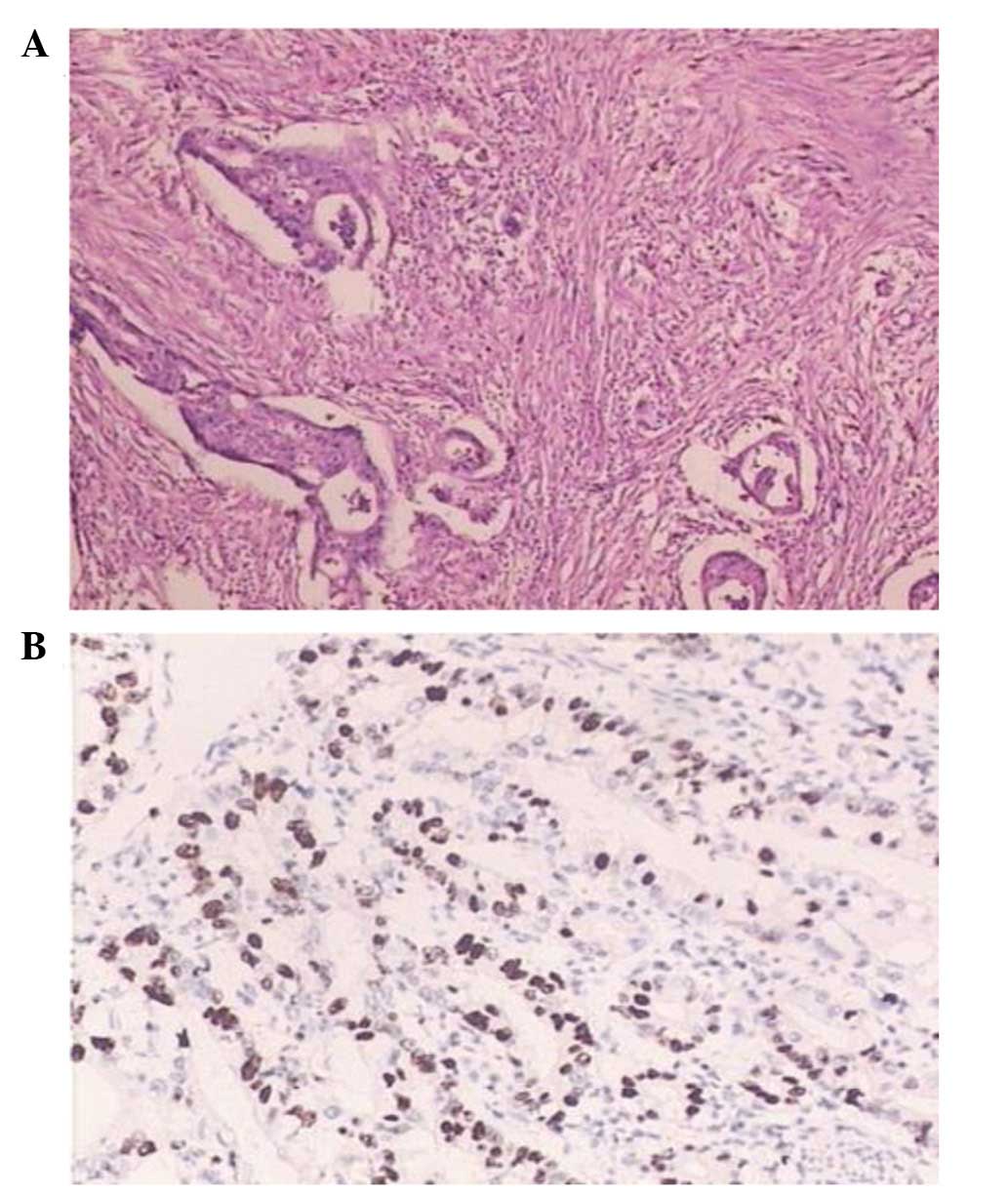
2012. Postoperative pathological analysis indicated moderately
differentiated adenocarcinoma of the stomach antrum, tumor invasion
into the serosa and evidence of metastasis into only one of the
dissected lymph nodes at the greater curvature. Pathological and
immunohistochemical analyses were conducted using the
hematoxylin-eosin staining (HE Stain kit; Beyotime Institute of
Biotechnology, Haimen, China) and avidin-biotin-peroxidase
(Vectastain ABC IHC kit; Vector Laboratories, Inc., Burlingame, CA,
USA) methods, respectively. All paraffin sections were 4 µm in
thickness (RM2125 RTS The Essential Microtome; Leica Microsystems,
Inc., Buffalo Grove, IL, USA). The antibodies used were as follows:
Rabbit polyclonal anti-human c-ErbB-2 (dilution, 1:200; catalog
no., ab2428); Abcam, Cambridge, MA, USA), mouse monoclonal
anti-human p53 (dilution, 1:1,000; catalog no., ab26; Abcam),
rabbit polyclonal anti-human epidermal growth factor receptor
(EGFR; dilution, 1:2,500; catalog no., ab2430; Abcam), rabbit
monoclonal anti-human p16 (dilution, 1:2,000; catalog no., ab51243;
Abcam), rabbit polyclonal anti-human type IIα topoisomerase
(dilution, 1:1,000; catalog no., #4733; Cell Signaling Technology,
Inc., Danvers, MA, USA) and rabbit polyclonal anti-human Ki-67
(dilution, 1:1,000; catalog no., ab15580; Abcam).
Immunohistochemical results were as follows: c-erbB-2 (+), p53 (−),
EGFR (−), p16 (−), type II topoisomerase (++), Ki-67 (60%)
(Fig. 1).
The postoperative course was uneventful. The patient
was discharged in good general condition 1 week after the
operation. Between 3 weeks and 5 months after the surgery, the
patient received 6 courses of adjuvant chemotherapy according to
the SOX scheme (60 mg oral S-1 twice a day on days 1–14 and 200 mg
intravenous infusion oxaliplatin on day 1 every 3 weeks). The
patient's CEA levels gradually declined to within normal limits 7
months after the surgery. The patient was systemically followed
once every 3 months following the completion of chemotherapy and no
abnormalities were noted.
However, 8 months after the surgery, the patient
suddenly developed paroxysmal finger numbness of the left hand with
hypopselaphesia, and these symptoms did not improve even following
nerve nutrition therapy (0.5 mg oral mecobalamin 3 times a day, for
2 months). Symptoms of numbness were still present 1 year after
surgery, with thigmesthesia and loss of precision grip function,
accompanied by paroxysmal tinnitus of the left ear. Physical
examination revealed attenuated proximal muscle strength (grade IV)
(11), decreased deep sensation of
the left upper limb and positive Hoffmann sign of the left hand.
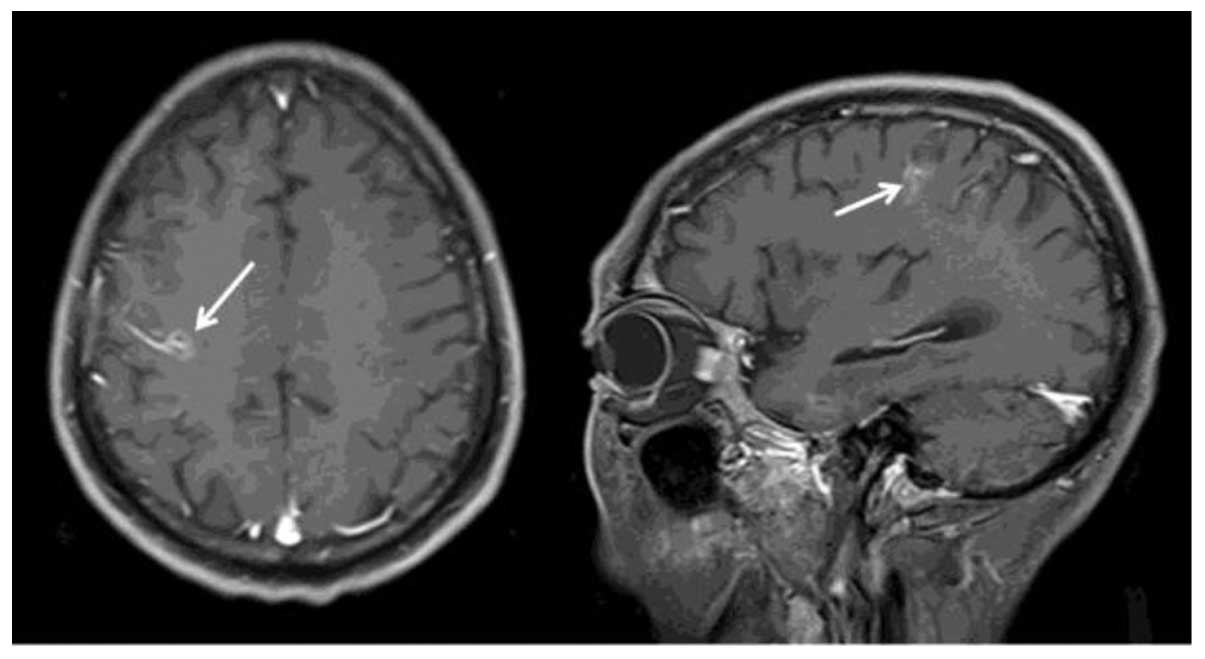
Cranial enhanced magnetic resonance imaging (MRI; MAGNETOM Avanto
1.5T; Siemens Heathcare, Erlangen, Germany) identified a tumor
(22×15 mm) in the junctional zone of the right frontal lobe and the
parietal lobe, accompanied by mild hemorrhage and peritumoral edema
(Fig. 2). A lumbar puncture biopsy
was performed, however, no malignant cells were found in the
cerebrospinal fluid. An enhanced CT scan of the chest and an
enhanced MRI scan of the liver demonstrated no abnormalities.
Laboratory data were within normal limits, with the exception of
signs of anemia, with a red blood cell count of
3.37×1012/l (normal range, 4.0–5.5×1012/l)
and a hemoglobin level of 6.7 g/dl (normal range, 12–16 g/dl). The
patient was followed up monthly for anemia; however, for ~3 months
there were no changes from the original values.
The patient declined brain metastasectomy or
palliative chemotherapy, but received 30 Gy of stereotactic
radiotherapy delivered in 5 fractions over 1 week. A follow-up
brain CT performed 2 months after radiotherapy revealed a reduced
tumor in the brain (16×12 mm). The patient was alive with good
health condition 8 months after radiotherapy. At this point, the
patient's nervous system symptoms were not markedly improved and
the patient continued to exhibit anemia (hemoglobin, 6–7 g/dl),
which was treated with Yang Xue Yin (10 ml orally administered 3
times/day). However, the patient refused to undergo any further
imaging examinations due to the high cost.
Discussion
The incidence of brain metastasis with gastric
cancer is rare and has been reported to be <1% of gastric cancer
cases (4,5). Furthermore, the majority of the reported
cases of brain metastasis were accompanied by lymph node, liver,
lung or bone metastasis (4,5,12); there
have been extremely few reports of brain metastasis as a solitary
lesion from gastric cancer. An early follow-up study reported that
the most frequent initial symptoms of brain metastasis are
headache, mental status changes, migraine, vision disorder and
Jacksonian epilepsy (13). In the
present study, these peripheral nervous system symptoms were
initially considered to be caused by chemotherapy with oxaliplatin.
After obtaining a medical history, and performing a comprehensive
physical examination and cranial enhanced MRI, the patient was
clinically diagnosed with brain metastasis of gastric cancer.
However, malignant tumor cells were not recovered by lumbar
puncture to confirm a pathological diagnosis. CEA in cerebrospinal
fluid was positive.
A follow-up brain CT performed 2 months after
radiotherapy revealed a reduced tumor in the brain. The patient was
alive with good health condition 8 months after radiotherapy. The
median survival of patients with metastatic gastric cancer is no
more than 1 year (13). In
particular, the overall prognosis of patients with brain metastases
from gastric cancer is extremely poor, with a median survival time
of 2–4 months (4–6,14). In the
absence of clear guidelines on therapy, each case requires
individual analysis and a multidisciplinary approach. Patients with
a solitary metastasis are predominantly treated by resection,
radiotherapy and chemotherapy, whereas palliative care may be a
more appropriate option for the treatment of multiple metastases
(4,5,15,16). In the present case, the patient
declined brain metastasectomy or palliative chemotherapy and
received 30 Gy of stereotactic radiotherapy delivered in 5
fractions.
The present study reports a rare case of gastric
cancer with brain metastasis. The present case report highlights
several key learning points. Gastric cancer with metastasis may
appear as a single lesion in brain and without typical central
nervous system symptoms. Peripheral nervous system symptoms should
be highlighted for brain metastasis. Thus, the current case raises
awareness that gastric cancer may present as brain metastasis,
particularly in patients with peripheral nervous system
symptoms.
In conclusion, brain metastasis of gastric cancer is
difficult to treat. In the current case, the patient rejected brain
metastasectomy and chemotherapy. In such cases, stereotactic
radiotherapy may be proposed with curative intent when appropriate.
The current patient is an outstanding example of the beneficial use
of stereotactic radiotherapy for longer survival time.
References
|
1
|
World Health Organization: Latest World
Cancer Statistics. Global cancer burden rises to 14.1 million new
cases in 2012: Marked increase in breast cancers must be addressed.
Press release no. 223. IARC. (Lyon/Geneva). Dec 12–2013.
|
|
2
|
Yang L: Incidence and mortality of gastric
cancer in China. World J Gastroenterol. 12:17–20. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Deng J, Liang H, Wang D, Sun D, Pan Y and
Liu Y: Investigation of the recurrence patterns of gastric cancer
following a curative resection. Surg Today. 41:210–215. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kasakura Y, Fujii M, Mochizuki F, Suzuki T
and Takahashi T: Clinicopathological study of brain metastasis in
gastric cancer patients. Surg Today. 30:485–490. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
York JE, Stringer J, Ajani JA, Wildrick DM
and Gokaslan ZL: Gastric cancer and metastasis to the brain. Ann
Surg Oncol. 6:771–776. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Go PH, Klaassen Z, Meadows MC and
Chamberlain RS: Gastrointestinal cancer and brain metastasis: A
rare and ominous sign. Cancer. 117:3630–3640. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Kitayama Y, Yoden Y and Okamoto N: A case
of effective paclitaxel therapy for gastric cancer with brain
metastasis. Gan To Kagaku Ryoho. 33:981–984. 2006.(In Japanese).
PubMed/NCBI
|
|
8
|
Kojima Y, Watanabe T, Sanada T, Hiramatsu
Y, Nakane Y, Yamamura M, Hioki K and Yamamoto M: A case report of
brain metastasis due to an advanced gastric cancer. Gan No Rinsho.
34:1731–1734. 1988.(In Japanese). PubMed/NCBI
|
|
9
|
Mizumatsu S, Nishimura T, Sakai K, Goto M,
Sugatani H and Higashi T: A case of brain metastasis from gastric
cancer involving bilateral middle cerebellar peduncles. No Shinkei
Geka. 34:955–960. 2006.(In Japanese). PubMed/NCBI
|
|
10
|
Perri F, Bisceglia M, Giannatempo GM and
Andriulli A: Cerebellar metastasis as a unique presenting feature
of gastric cancer. J Clin Gastroenterol. 33:80–81. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
James MA: Use of the Medical Research
Council muscle strength grading system in the upper extremity. J
Hand Surg Am. 32:154–156. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Chang YR, Han DS, Kong SH, Lee HJ, Kim SH,
Kim WH and Yang HK: The value of palliative gastrectomy in gastric
cancer with distant metastasis. Ann Surg Oncol. 19:1231–1239. 2012.
View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Stortebecker TP: Metastatic tumors of the
brain from a neurosurgical point of view; a follow-up study of 158
cases. J Neurosurg. 11:84–111. 1954. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Nomura T, Yoshikawa T, Kato H, Nikkuni K,
Sasaki K, Shirai Y and Hatakeyama K: Early gastric cancer
manifested as brain metastasis: Report of a case. Surg Today.
27:334–336. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Murawa D, Nowaczyk P, Szymkowiak M and
Karaszewska B: Brain metastasis as the first symptom of gastric
cancer-case report and literature review. Pol Przegl Chir.
85:401–406. 2013.PubMed/NCBI
|
|
16
|
Bussing A, Zhai XF, Peng WB and Ling CQ:
Psychosocial and spiritual needs of patients with chronic diseases:
Validation of the Chinese version of the spiritual needs
questionnaire. J Integr Med. 11:106–115. 2013. View Article : Google Scholar : PubMed/NCBI
|