Introduction
Myoepithelial carcinomas (MECs), also termed
malignant myoepitheliomas (1), are
composed almost exclusively of tumor cells with morphological and
immunohistochemical myoepithelial differentiation and clear-cut
tumor infiltration into adjacent tissue. MECs account for 1–4% of
all salivary gland tumors and arise predominantly from the major
glands (1). Occasionally, MECs occur
in the intraoral minor salivary glands and most frequently involve
the palate (2). In the 2005 edition
of the World Health Organization (WHO) histological classification
of salivary gland tumors, MECs were considered to be low-grade
tumors with a low tendency for local recurrence and metastasis
(3). MECs most commonly affect
patients in their third to fifth decades of life, with a slight
female predilection (2). The clinical
prognosis of MECs is not well characterized, however, certain
studies have suggested that MECs should be recognized as high-grade
malignancies with a poor prognosis (4). Extensive resection with free margins is
the recommended treatment for MEC lesions (5). To the best of our knowledge, there is no
published literature illustrating MECs of the vallecula, which
makes the vallecula a rare location for MECs and region that is
challenging to access for surgeons (6). The present study reports the case of a
patient with MEC of the vallecula, which was successfully managed
using a lateral pharyngotomy approach and the construction of a
sternohyoid myofascial flap.
Case report
A 48-year-old female patient was referred to the
Department of Oncology, West China Hospital of Stomatology (Sichuan
University, Chengdu, China) from the Sichuan Provincial People's
Hospita (Chengdu, China) in April 2014, due to an 8-month history
of a foreign body sensation in the pharynx and a 1-month history of
intermittent hemoptysis. Upon physical examination, a firm mass was
palpable near the tongue base, while the posterior margin of the
mass was too deep to reach. No other significant manifestations in
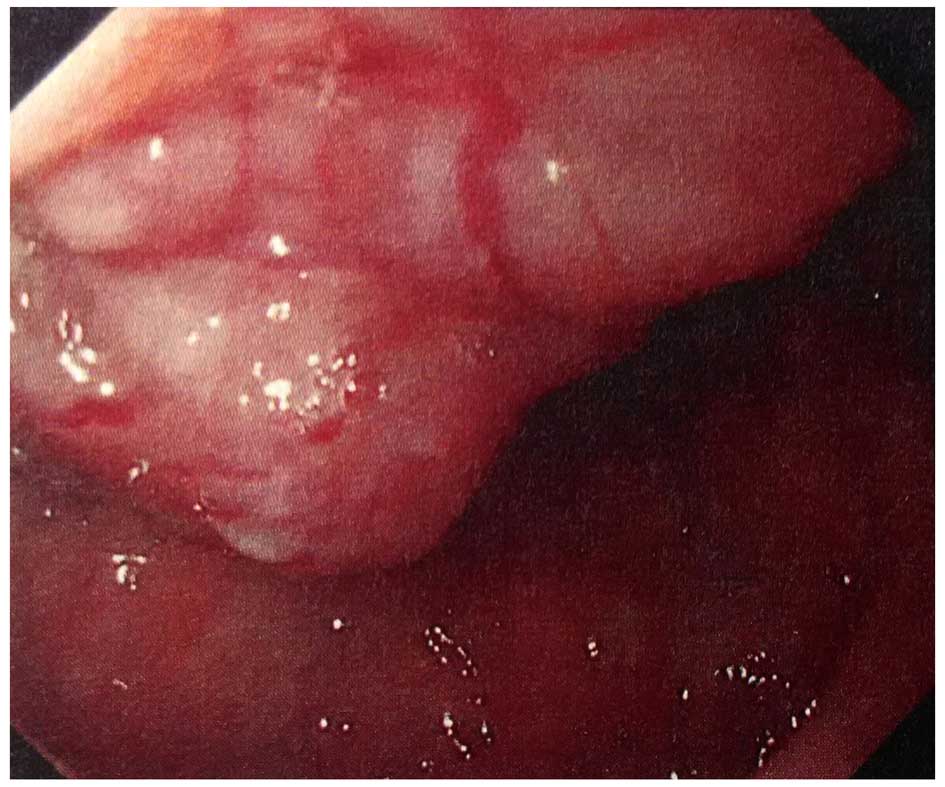
the oral cavity and neck region were observed. The endoscopic
examination revealed an exophytic tumorous lesion with tortuous
vessels on the surface. The majority of the mass was located in the
vallecula and involved the base of the tongue and the epiglottis
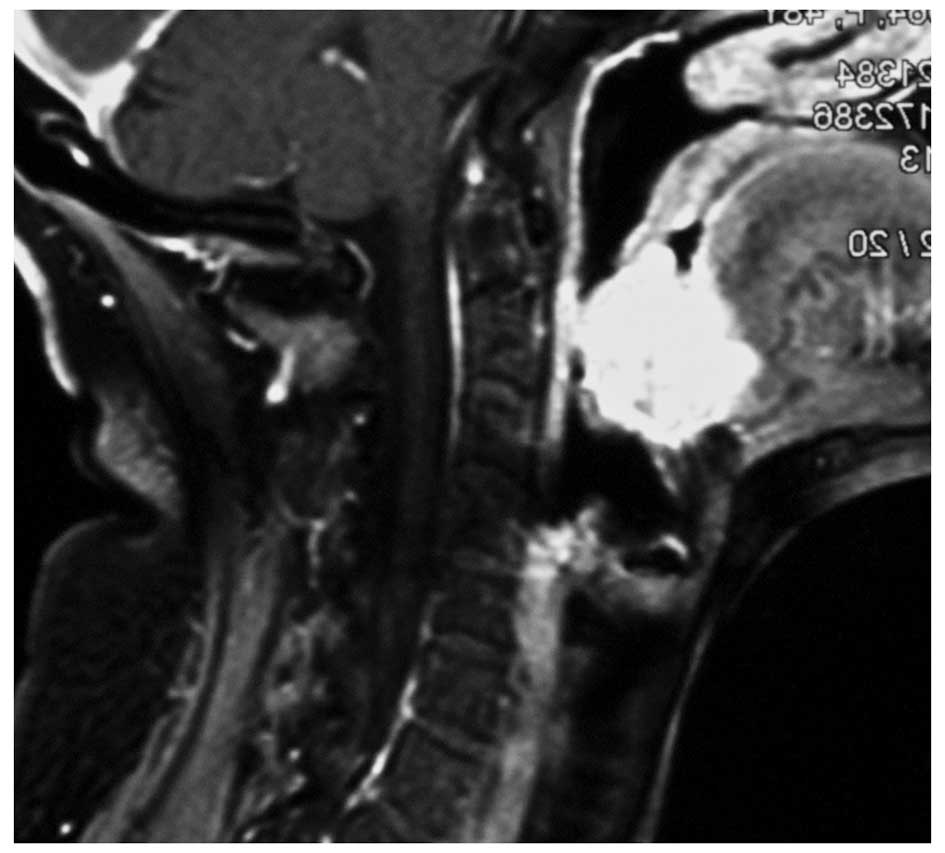
(Fig. 1). Magnetic resonance imaging
(MRI) demonstrated a soft tissue mass measuring 41×35×31 mm in
size, which extended from the anterior wall of the epiglottis to
the base of the tongue, but did not affect the parapharyngeal space
(Fig. 2). The mass was well enhanced
by gadolinium administration. The pertechnetate thyroid scan
single-photon emission computed tomography imaging differentiated
the mass from the ectopic thyroid gland of the tongue base. Chest
radiographs and ultrasounds of the abdomen showed no sign of
distant metastasis.
Since the patient had a history of intermittent
hemoptysis, the surgical excision was performed without a
preoperative biopsy. Intraoperative frozen sections were used to
diagnose the lesion. Under general anesthetic, the mass was removed
using the lateral pharyngotomy approach (7). A sternohyoid myofascial flap was used to
reconstruct the defect at the base of the tongue. A tracheostomy
and primary suture were also performed. The trunks of the
ipsilateral hypoglossal nerve and lingual artery were identified
and protected prior to surgery in the pharynx at the safe mucosal
margins. The mass, which involved the epiglottis, tongue base and
vallecula, was fully excised. The intraoperative frozen sections
indicated a preliminary diagnosis of MEC, and the surgical margins
were free of disease. The sternohyoid muscle on the right side was
elevated up towards the superior margin of the thyroid cartilage,
and the superficial fascia was fixed to the underlying muscle. The
external surface of the flap and fascia was remodeled into the
pharynx for the reconstruction of the tongue base, prior to the
fixation of the residual larynx to the newly formed tongue base.
The patient was discharged 10 days subsequent to the surgery,
without postsurgical chemotherapy or radiotherapy. The patient
received regular follow-ups, and exhibited no signs of local
recurrence or lymph node or distant metastasis in the 18 months
following surgery.
Macroscopically, the excised mass was 4×3 cm in size
and the cut surface was pale white in color. The surrounding muscle
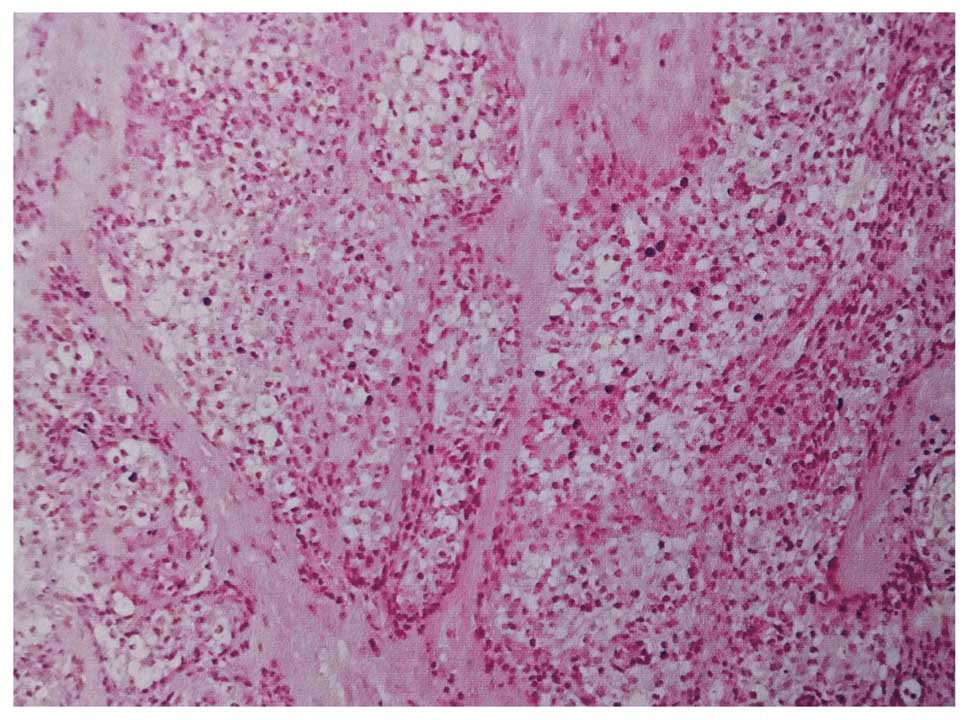
was infiltrated by the mass. Additional microscopic examination
identified the infiltrative growth pattern and necrotic foci in the
tumor. The microscopic examination also revealed that the majority
of the tumor was composed of clear cells that were characterized by
abundant vacuolated clear cytoplasm and displaced nuclei. Scattered
spindle cells and epithelioid cells were also identified in the
tumor (Fig. 3). Only a few cells were
recognized with cellular atypia, and the number of mitoses was low.
A hyalinized matrix was also identified, which divided the tumor
cells into small nests or thin cords. There was no clinical or
pathological evidence of a pre-existing pleomorphic adenoma.
Cytokeratin-5, −6 and −7 (CK-5, −6 and −7) and tumor protein p63
(p63) were expressed in the tumor cells when assessed using
immunohistochemical staining; however, the S-100 protein (S-100)
and carcinoembryonic antigen (CEA) were not expressed. As a result
of the histological examination and immunohistochemical staining, a
diagnosis of MEC was made.
The present study was in compliance with the
Declaration of Helsinki (8) and was
approved by the Ethics Committee of the West China College of
Stomatology, Sichuan University. Written informed consent was
obtained from the patient for the publication of the case report
and accompanying images.
Discussion
MECs are a rare group of tumors that account for
1–4% of salivary gland tumors and 0.2–0.32% of minor salivary gland
tumors (2). MECs are diagnosed
following the criteria of lesions that are composed almost
exclusively of tumor cells, with myoepithelial differentiation and
clear-cut tumor infiltration into adjacent tissue (6). The majority of studies demonstrate that
MECs are more prevalent in the major salivary glands (5,6); however,
the findings of a study by Kane et al indicated that minor
salivary glands have a greater involvement (71%) with MEC (1). MECs involving intraoral minor salivary
glands tended to occur in middle to older age groups (range, 14–77
years; mean, 56.9 years), with a slight male predilection
(male-to-female ratio, 0.87:1) and a predominance of palate
involvement (60.7%) (2). These
results were generally in agreement with the clinical findings of
MECs that involved the major salivary glands.
Considering the rarity and variety of MECs, the
clinical prognosis and biological behavior of the disease were not
previously well-characterized. In the 1991 and 2005 editions of the
WHO Histological Classification of Salivary Gland Tumors, MECs were
considered to be low-grade tumors with a low tendency for local
recurrence and metastasis (3,9). However, according to a study by Yu et
al (5), MECs may be recognized as
high-grade malignancies with poor prognoses. Yang et al
(2) analyzed MECs of the intraoral
minor salivary glands and indicated that those particular MECs were
likely to be low-grade malignancies. Di Palma and Guzzo (10) indicated an association between the
biological behavior and the origin of the tumor, finding that de
novo MECs tended to be a high-grade malignancies. An
association between the biological behavior and the origin of the
tumor was not identified in the studies by Savera et al
(6) and Kane et al (1), and in the latter study, several other
valuable histological features that correlated strongly with the
clinical behavior of MECs were identified.
Histologically, the tumor cells of MECs are
categorized according to cytological features as epithelioid,
clear, plasmacytoid and spindle cells (6). The majority of the neoplasms exhibit one
prevalent cell type, which blends imperceptibly with the
surrounding cell types (6). Two
tumor-associated matrices, consisting of myxoid and hyalinized
matrices, are acknowledged, and the hyaline stroma is the most
commonly observed (1). In the present
study, the MEC lesion was mainly composed of clear cells with
scattered spindle cells and epithelioid cells, which was divided
into small nests or thin cords by a hyalinized matrix.
Immunohistochemistry is essential in order to identify MECs. The
diagnosis of MECs requires reactivity with the CKs and at least one
of the other myoepithelial markers, including S100, vimentin,
calponin, p63 or CD10 (3). In the
present study, the MEC sample expressed CK-5, −6 and −7 and p63,
but did not express S-100 and CEA. The majority of previous studies
indicated that the MECs expressed S-100, and only 16% of MEC
lesions did not express S-100, which made the diagnosis of MEC even
more challenging (1,3,6). In the
absence of S-100 expression, the expression of calponin, common
acute lymphocytic leukemia antigen, p63 and vimentin aided the
diagnosis of MECs (1). p63 is a
useful marker of myoepithelial cells in salivary gland neoplasms,
but is also expressed in squamous cell carcinoma and mucoepidermoid
carcinoma (6). The differentiation of
cells is aided by the expression of CEA at the cell luminal
surface; therefore, CEA is used to exclude neoplasms with clear
cells or epitheloid cells, including adenoid cystic carcinoma,
adenocarcinoma and epithelial-myoepithelial carcinoma (6). In the present study, exclusive
myoepithelial differentiation was confirmed using morphological and
immunohistochemical examinations, while the malignancy diagnosis
was supported by an infiltrative growth pattern and the presence of
necrotic foci.
Due to the high recurrence rate, radical surgery
with free margins is recommended for the successful management of
MEC lesions (5,6), and the efficacy of radiotherapy and
chemotherapy to treat MEC remains controversial. Metastasis of MEC
to the lymph nodes is infrequent, and since the present patient
showed no evidence of lymph node metastasis, a neck dissection was
not recommended. Several surgical approaches have been proposed for
resecting tumors in the neck region, depending on the size and site
of the tumor (7,11). Kermani et al presented the case
of a benign myoepithelioma of the vallecula, and removed the mass
using the suprahyoid approach (12).
In the present study, the suprahyoid approach was not recommended
due to the infiltrative growth pattern of the MEC and the
involvement of the vallecula, tongue base and epiglottis, which was
identified by MRI scans. Since the lateral pharynx was not affected
by MEC, a lateral pharyngotomy was performed for radical resection
of the mass with free margins. The wide local resection in this
area is likely to induce a swallowing impairment and velopharyngeal
incompetence. In order to prevent such complications, a sternohyoid
myofascial flap was used to reconstruct the tongue base. No evident
complications were noted following surgery, and the patient was
free of recurrence for 18 months following surgery.
In conclusion, the present study presents the
successful surgical treatment of a rare MEC in the vallecula. The
present case requires consideration due to: i) The unusual location
of the mass, as no previous case of MEC was indicated to arise from
the vallecula; ii) the unusual immunohistochemical appearance, as
rare MECs do not express S-100, as presented here; and iii) the
unusual technique used to treat the MEC, as there are no specific
surgical guidelines for resecting MECs in the vallecula. The
present study demonstrates that the lateral pharyngotomy and
sternohyoid myofascial flap are viable options for the successfully
management of MECs of the vallecula.
Acknowledgments
The authors thank Miss. Yaneng Ge from the
Department of Trauma, West China College Of Stomatology, Sichuan
University (Chengdu, China), for providing images of the patient
and for certain important suggestions for the present
manuscript.
References
|
1
|
Kane SV and Bagwan IN: Myoepithelial
carcinoma of the salivary glands: A clinicopathologic study of 51
cases in a tertiary cancer center. Arch Otolaryngol Head Neck Surg.
136:702–712. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Yang S, Li L, Zeng M, Zhu X, Zhang J and
Chen X: Myoepithelial carcinoma of intraoral minor salivary glands:
A clinicopathological study of 7 cases and review of the
literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.
110:85–93. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Thompson L: World Health Organization
classification of tumours: Pathology and genetics of head and neck
tumours. Ear Nose Throat J. 85:742006.PubMed/NCBI
|
|
4
|
Wang C, Zhang Z, Ge Y, Liu Z, Sun J, Gao Z
and Li L: Myoepithelial carcinoma of the salivary glands: A
clinicopathologic study of 29 patients. J Oral Maxillofac Surg.
73:1938–1945. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Yu G, Ma D, Sun K, Li T and Zhang Y:
Myoepithelial carcinoma of the salivary glands: Behavior and
management. Chin Med J (Engl). 116:163–165. 2003.PubMed/NCBI
|
|
6
|
Savera AT, Sloman A, Huvos AG and Klimstra
DS: Myoepithelial carcinoma of the salivary glands: A
clinicopathologic study of 25 patients. Am J Surg Pathol.
24:761–774. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Laccourreye O, Benito J, Menard M, Garcia
D, Malinvaud D and Holsinger C: Lateral pharyngotomy for selected
invasive squamous cell carcinoma of the lateral oropharynx - part
I: How. Laryngoscope. 123:2712–2717. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
World Medical Association: World Medical
Association Declaration of Helsinki: Ethical principles for medical
research involving human subjects. JAMA. 310:2191–2194. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Seifert G, Sobin LH and Thackray AC:
Histological Typing of Salivary Gland Tumours (2nd). 9–10.
Springer-Verlag. Berlin: 1991. View Article : Google Scholar
|
|
10
|
Di Palma S and Guzzo M: Malignant
myoepithelioma of salivary glands: Clinicopathological features of
ten cases. Virchows Arch A Pathol Anat Histopathol. 423:389–396.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Mulwafu W, Fagan JJ and Lentin R:
Suprahyoid approach to base-of-tongue squamous cell carcinoma. S
Afr J Surg. 44(120): 122–124. 2006.
|
|
12
|
Kermani W, Belcadhi M, Ben Ali M, Sriha B
and Bouzouita K: Myoepithelioma of the vallecula: A case report.
Ear Nose Throat J. 90:E9–E11. 2011.PubMed/NCBI
|