Introduction
Nitroxoline (5-nitro-8-hydroxy-quinoline) is an
established antibiotic that has been widely used in European, Asian
and African countries for >50 years (1). It is particularly effective for the
treatment of urinary tract infections (UTI) due to its unique
pharmacokinetic properties (1). When
administered orally, nitroxoline is rapidly absorbed into the
plasma and then excreted into urine (2). It also has a long retention time in
urine (2), thus, making it ideal for
UTI treatment. Recently, nitroxoline has gained considerable
attention due to its potent anticancer properties. It was first
identified as an effective inhibitor of angiogenesis by two
parallel screens: A target-based screen for methionine
aminopeptidase-2 (MetAP-2) inhibitors from a library of 175,000
chemical compounds and a cell-based screen using the Johns Hopkins
Drug Library to identify currently used clinical drugs that can
also inhibit human umbilical vein endothelial cell (HUVEC)
proliferation (3). Thereafter, more
studies confirmed the anticancer activity of nitroxoline and
further demonstrated its anticancer mechanism (3–5). In
particular, nitroxoline demonstrated potent anticancer activity
against various types of cancer cell, including lymphoma, leukemia,
glioma, bladder cancer, breast cancer, pancreatic cancer and
ovarian cancer cells (3–5). As well as inhibiting angiogenesis,
nitroxoline was also able to induce cancer cell apoptosis (4), and suppress cancer cell migration and
invasion (6). Taken together, as an
established drug for UTI treatment, nitroxoline has exhibited great
promise as a novel candidate for anticancer treatment.
Drug repurposing, the process of identifying novel
uses for existing drugs, has been gaining popularity in recent
years. The major advantage of this approach is that the
pharmacokinetic, pharmacodynamic and toxicity profiles of known
drugs are generally well known due to of years of clinical history
(1,7).
Thus, exploring established non-cancer drugs for anticancer
activity provides an opportunity to rapidly advance therapeutic
strategies into clinical trials. To rapidly advance nitroxoline
repurposing for anticancer treatment into clinical trials, the
present study performed systemic preclinical pharmacodynamic
evaluation of nitroxoline, with specific aims to confirm the
anticancer activity of nitroxoline, select cancer types suitable
for nitroxoline treatment and provide a reference dosage regimen
for future clinical application.
Materials and methods
Drugs and materials
Nitroxoline (Lot: KLL-20110601 J) and its metabolite
nitroxoline sulfate (Lot: 5209-005A1), which was isolated and
purified from the urine of nitroxoline-treated mice, were provided
by Jiangsu Asieris Pharmaceuticals Co., Ltd. (Taizhou, China).
Cisplatin (Lot: F20100420) was purchased from Qilu Pharmaceutical
Co., Ltd. (Jinan, China).
Cell lines and cell culture
The human cell lines used for the in vitro
and in vivo anticancer activity assays are listed in
Table I. Among them, HUVEC, HepG2,
A549, LoVo, MCF7, T24, 5637 and J82 cell lines were obtained from
American Type Tissue Culture Collection (ATCC; Manassas, VA, USA),
and cultured in their respective ATCC-specified medium. KCC853,
SGC-7901 and human embryonic lung fibroblast (HELF) cell lines were
purchased from China Infrastructure of Cell Line Resources
(Beijing, China), and cultured in RPMI-1640 medium (Invitrogen;
Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with
10% FBS (Gibco; Thermo Fisher Scientific, Inc.), 100 U/ml
penicillin and 100 µg/ml streptomycin (Invitrogen; Thermo Fisher
Scientific, Inc.). All cells were maintained in a humidified
incubator with 5% CO2 at 37°C.
 | Table I.Anti-cancer activity of nitroxoline
in vitro. |
Table I.
Anti-cancer activity of nitroxoline
in vitro.
| Cell line | Origin of cell
line | Inhibition rate at 80
µM, % | IC50,
µM | Inhibition rate at 10
µM, % |
|---|
| HUVEC | Human umbilical vein
endothelial cells |
97.1±1.2 |
7.06±1.64 |
66.1±7.5 |
| T24 | Bladder transitional
cell carcinoma |
99.4±0.5 |
1.68±0.09c |
94.0±2.4b |
| 5637 | Bladder grade II
carcinoma |
98.0±1.9 |
2.45±0.23b |
87.9±1.9b |
| KCC853 | Clear cell renal cell
carcinoma |
96.1±2.3 |
2.96±0.89a |
86.0±7.8a |
| HepG2 | Hepatocellular
carcinoma |
95.3±2.2 |
5.75±1.04 |
57.4±0.6 |
| SGC-7901 | Gastric
carcinoma |
96.1±2.9 |
7.18±0.19 |
43.6±2.5b |
| A549 | Lung
adenocarcinoma |
75.1±1.6c |
11.43±2.07 |
53.6±6.7 |
| MCF7 | Breast
adenocarcinoma |
74.1±0.9c |
20.58±4.83c |
51.1±
2.1a |
| J82 | Bladder
transitional cell carcinoma |
57.8±1.2c |
20.83±5.47b |
46.8±7.4a |
| LoVo | Colorectal
carcinoma |
45.0±1.1c |
5.99±0.56 |
33.6±1.4c |
| HELF | Human embryonic
lung fibroblasts |
39.8±1.2c |
13.26±2.61 |
2.9±0.8c |
Cytotoxicity assay
Cells were seeded in 96-well plates at a density of
3,000 cells per well. After 24 h culture in normal growth medium,
the cells were exposed to graded concentrations (84, 42, 21, 10.5,
5.25, 2.63, 1.32 and 0.66 µM) of nitroxoline or nitroxoline sulfate
for 96 h. Following treatment, the viability of the cells was
determined by performing a methyl thiazolyl tetrazolium (MTT)
assay. Briefly, MTT (0.5 mg/ml; Sigma-Aldrich, St. Louis, MO, USA)
was added and cells were incubated for 4 h at 37°C. After removing
the supernatant, the formazan crystals produced were dissolved in
200 µl dimethyl sulfoxide (Sigma-Aldrich) and the absorbance at 570
nm was determined using a microplate reader (Multiskan Ascent;
Thermo Labsystems; Thermo Fisher Scientific, Inc.). Data are
presented as the mean ± standard deviation (SD) derived from
quadruplicate samples of at least two independent experiments. The
half maximal inhibitory concentration (IC50) was
determined by logistic non-linear regression analysis of the
dose-response curves (Origin software, version 7.0; OriginLab
Corporation, Northampton, MA, USA).
In vivo anti-cancer effect assay
All animal care and experimental procedures
conformed to the Guide for the Care and Use of Laboratory Animals
(8) as adopted and promulgated by
Beijing Medical Experimental Animal Care Commission. The present
study was approved by The Laboratory Animal Ethics Committee of
Beijing Institute of Radiation Medicine (Beijing, China;
certificate no., BIRMSPF-120125A). A total of 220 male athymic nude
mice (Balb/c nu/nu; 8 weeks old) were obtained from Beijing Vital
River Laboratory Animal Technology Co., Ltd. (Beijing, China),
housed in controlled specific pathogen-free conditions (25±1°C
constant temperature, 40–60% relative humidity, 12-h light/dark
cycle) and allowed free access to food and water during the study
period.
A total of 140 nude mice were used to generate mouse
models of orthotopic bladder cancer, as previously described
(3,9,10).
Briefly, mice were anesthetized by intraperitoneal injection of 100
mg/kg ketamine/10 mg/kg xylazine (Sigma-Aldrich). A superficial 6–0
polypropylene purse-string suture [Medico (Huaian) Co., Ltd.,
Huaian, China] was placed around the urethral meatus prior to
passing a lubricated 24-gauge intravenous catheter [Medico (Huaian)
Co., Ltd.] through the urethra into the bladder. Subsequent to
aspirating urine and irrigating the bladder with phosphate-buffered
saline (PBS; Invitrogen; Thermo Fisher Scientific, Inc.), a stylet
needle was used to slightly impair the bladder urothelium by gently
scraping; this action also facilitated tumor cell seeding.
Thereafter, T24 or 5637 bladder carcinoma cells (2×106)
were instilled into the bladders of nude mice (70 mice per tumor
model) as single-cell suspensions in 200 µl PBS and the
purse-string suture was tied down for a 2.5-h period, during which
the mice were kept anesthetized.
A total of 80 nude mice were used to establish a
mouse model of orthotopic renal cancer by subrenal capsule
implantation. First, 5×106 KCC853 clear cell renal
carcinoma cells in 200 µl PBS were subcutaneously injected into the
back of nude mice. When the subcutaneous tumor volume reached
400–600 mm3, tumor tissues were removed from the hosts
and cut into small sections measuring ~2×2×2 mm3 in size
under sterile conditions. The tumor sections were then implanted
into the subcapsular area of the right kidney of the nude mice, as
previously described (11,12).
Each of the three mouse model groups were sorted
into 5 or 6 groups (n=7–14 per group) with almost equal mean body
weight 2 weeks after establishment of the orthotopic tumor models.
The groups included the control group, the cisplatin group and the
nitroxoline groups. Cisplatin was used as the positive control drug
by intravenous injection at a dose of 5 mg/kg once a week. Mice
were orally administered with nitroxoline as the treatment group,
according to the dosage regimens described in Tables II–IV.
The control group was orally administered with normal saline (10
ml/kg) twice a day. Animals were sacrificed by CO2
asphyxiation 3–4 weeks after treatment to allow necropsy, and the
whole bladders or kidneys were harvested and assessed for tumor
weight. The whole weight of the bladder and orthotopic tumor was
calculated as bladder tumor weight, as the majority of the
orthotopic tumors infiltrated into the muscles of the bladders and
separate of the two tissues was difficult. Renal tumor weight was
calculated by subtracting the weight of the left normal kidney from
that of the right tumor-bearing kidney. The tumor growth inhibitory
rate was calculated as follows: Inhibitory rate (%) = [1 - (mean
tumor weight of treated group / mean tumor weight of control
group)] × 100.
 | Table II.Effects of nitroxoline on 5637 cell
bladder cancer orthotopic xenografts in nude mice. |
Table II.
Effects of nitroxoline on 5637 cell
bladder cancer orthotopic xenografts in nude mice.
|
| Drug
administration | Anti-cancer
activity | Toxicity |
|---|
|
|
|
|
|
|---|
| Drug | Dose, mg/kg | Schedule | Route | Tumor weight,
mga | Inhibition rate,
% | Body weight loss,
%a | Mortalities/total
mice, n |
|---|
| Control | Vehicle | BID for 21
days | p.o. |
164±61 |
|
14.8±4.9 |
4/14 |
| Cisplatin | 5 | QW for 3 weeks | i.v. |
79±41c | 52.0 |
19.8±9.1 |
2/14 |
| Nitroxoline | 30 | BID for 21
days | p.o. |
88±32b | 46.4 |
14.9±3.7 | 1/7 |
| Nitroxoline | 60 | BID for 21
days | p.o. |
63±24c | 61.4 |
12.0±3.8 |
2/14 |
| Nitroxoline | 120 | BID for 21
days | p.o. |
50±21c | 69.6 |
7.4±3.2 |
5/14 |
| Nitroxoline | 240 | BID for 21
days | p.o. |
43±19c | 73.6 |
12.2±4.7 | 2/7 |
 | Table IV.Effects of nitroxoline on KCC853 cell
renal tumor orthotopic xenografts in nude mice. |
Table IV.
Effects of nitroxoline on KCC853 cell
renal tumor orthotopic xenografts in nude mice.
|
| Drug
administration | Anti-cancer
activity | Toxicity |
|---|
|
|
|
|
|
|---|
| Drug | Dose, mg/kg | Schedule | Route | Tumor weight,
mga | Inhibition rate,
% | Body weight loss,
%a | Mortalities/total
mice, n |
|---|
| Control | Vehicle | BID for 21
days | p.o. |
183±73 |
|
11.8±4.3 | 2/16 |
| Cisplatin | 5 | QW for 3 weeks | i.v. |
99±35b | 46.0 |
15.0±3.3 | 1/16 |
| Nitroxoline | 60 | BID for 21
days | p.o. |
96±41b | 47.5 |
13.2±5.7 | 2/16 |
| Nitroxoline | 120 | BID for 21
days | p.o. |
89±23b | 51.4 |
9.2±3.7 | 4/16 |
| Nitroxoline | 240 | BID for 21
days | p.o. |
67±28b | 63.7 |
7.7±5.4 | 2/16 |
Immunohistochemical staining
The tumor tissues were fixed in formalin (Wuhan
Boster Biological Technology, Ltd., Wuhan, China), embedded in
paraffin (Wuhan Boster Biological Technology, Ltd.) and sectioned
into 4-mm sections. The tissue sections were deparaffinized and
rehydrated as follows: Sections were incubated in three washes of
xylene (Sigma-Aldrich) for 5 min each; sections were sequentially
incubated in 100, 95, 90, 80 and 70% ethanol (Sinopharm Chemical
Reagent Co., Ltd., Beijing, China) for 10 min each; and sections
were washed twice in distilled water for 5 min each. The tissues
were then blocked with 3% H2O2 to quench the
endogenous peroxidase activity. Antigen retrieval was performed by
boiling the slides in sodium citrate buffer (10 mM, pH 6.0; Wuhan
Boster Biological Technology, Ltd.) for 20 min. Slides were then
incubated with non-specific binding blocking buffer (PBS + 5%
bovine serum albumin + 0.1% Tween-20; Sigma-Aldrich) at room
temperature for 1 h, followed by rabbit anti-human polyclonal Ki67
(1:50 dilution; cat. no. BA2888; Wuhan Boster Biological
Technology, Ltd.), rabbit anti-human polyclonal survivin (1:50
dilution; cat. no. BA14055; Wuhan Boster Biological Technology,
Ltd.) and rabbit anti-human polyclonal cluster of differentiation
(CD)31 (1:50 dilution; cat. no. BA1346; Wuhan Boster Biological
Technology, Ltd.) antibodies overnight at 4°C. After washing with
PBS, slides were then incubated with goat anti-rabbit polyclonal
horseradish peroxidase-conjugated secondary antibody (1:200
dilution; cat. no. SV0002; Wuhan Boster Biological Technology,
Ltd.) at room temperature for 1 h. The immunohistochemistry
reaction was developed with a DAB substrate kit (Wuhan Boster
Biological Technology, Ltd.) prior to counterstaining the slides
with hematoxylin. Hematoxylin and eosin (H&E) staining was
performed using a H&E staining kit in accordance with the
manufacturer's protocol (Wuhan Boster Biological Technology, Ltd.).
Briefly, deparaffinized and rehydrated tissue slides were incubated
in hematoxylin solution for 2 min. Subsequent to washing twice with
distilled water for 5 min each, the slides were sequentially
immersed in acid alcohol, distilled water and ammonia solution for
10 sec each. Slides were then washed twice with distilled water for
5 min each, immersed in 80% ethanol for 10 min, incubated in eosin
solution for 15 sec, and then sequentially immersed in 90, 95 and
100% ethanol for 10 min each. Finally, the slides were incubated
twice in xylene for 5 min each and mounted with DPX Mountant for
histology (Sigma-Aldrich). Negative controls were treated the same
way except the primary antibody was replaced by the isotype-matched
anti-human IgG. The immunohistochemical staining was examined using
an EVOS X1 microscope (Advanced Microscopy Group; Thermo Fisher
Scientific, Inc.).
Statistical analysis
Data are presented as the mean ± SD. Equal variance
was assessed by Bartlett's test, and the statistical significance
of differences between groups was compared by one-way analysis of
variance test followed by Tukey's post-hoc test (GraphPad Prism
5.0; GraphPad Software Inc., La Jolla, CA, USA). P<0.05 was
considered to indicate a statistically significant difference.
Results
In vitro sensitivities of various
cancer cell lines to the anticancer activity of nitroxoline
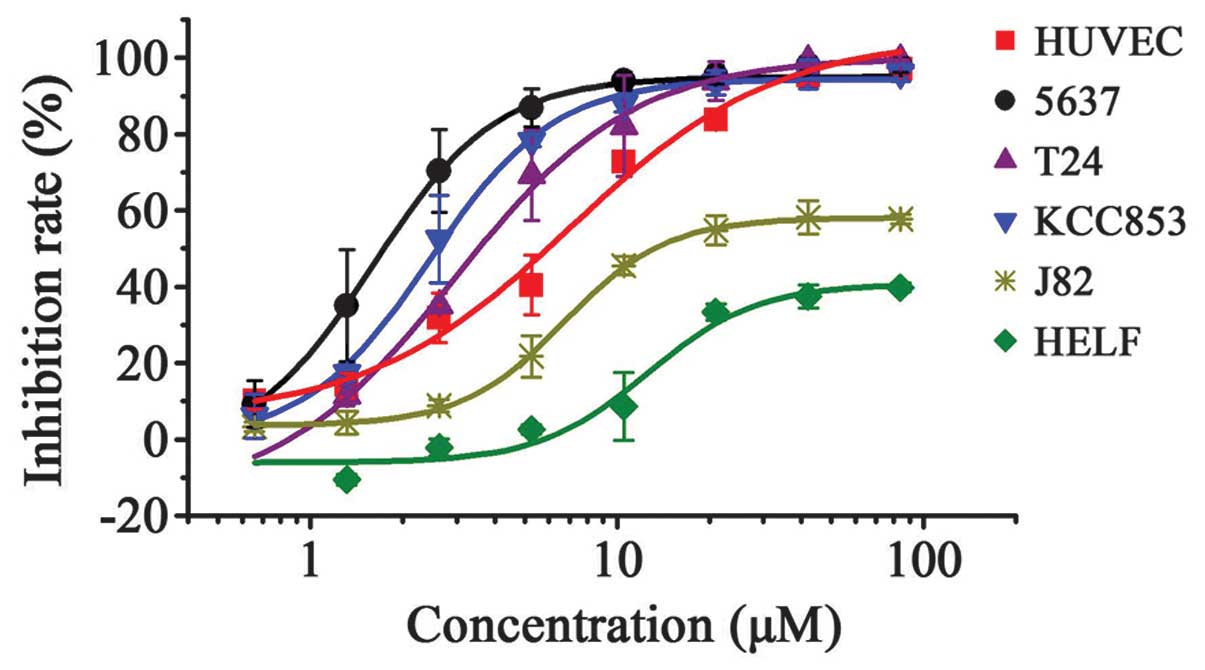
Nitroxoline inhibited the growth of all cell lines
in a dose-dependent manner (Table I).
However, there were marked differences among its effects on
individual cell lines. At the maximum concentration (80 µM),
nitroxoline caused complete (>95%) growth inhibition of the
HUVEC, T24, 5637, KCC853, HepG2 and SGC7901 cell lines (Table I). Among them, the T24, 5637 and
KCC853 urological cancer cell lines demonstrated an obvious left
shift in their dose-response curves (Fig.
1) and significant 2–4-fold decreases in IC50 values
compared with the well-known target cell line HUVEC (Table I) (3).
These results indicate nitroxoline is more effective at directly
inhibiting the proliferation of certain urological cancer cells
than others. Considering that the antimicrobial activity of
nitroxoline has been demonstrated at concentration of >10 µM
(13), and that daily nitroxoline
dosage of 400–750 mg (for adults) resulted in ≤10 µM nitroxoline
retention in human plasma and urine after 24 h (2), the present study next analyzed
nitroxoline from a translational perspective by comparing the
anticancer effects of 10 µM nitroxoline on the aforementioned cell
lines. T24, 5637 and KCC853 exhibited 86–94% growth inhibition upon
10 µM nitroxoline treatment. Nitroxoline was significantly more
effective and sensitive than in HUVEC cells, which exhibited only
~66% growth inhibition. However, not all bladder cancer cell lines
were equally sensitive to nitroxoline. J82 cells exhibited ~47%
growth inhibition following 10 µM nitroxoline treatment, and its
IC50 value was 7–10-fold higher than those of T24, 5637
and KCC853 (Table I and Fig. 1). In addition, HELF, a non-cancerous
cell line, was insensitive to the cytotoxic effect of nitroxoline,
exhibiting just ~2.9% growth inhibition at 10 µM nitroxoline; this
result confirmed the excellent safety profile of nitroxoline, as
established by its 50-year clinical history. Taken together, the
results indicate that certain urological cancer cell lines, such as
T24, 5637 and KCC853, are sensitive to nitroxoline treatment and
are suitable for establishing urological tumor orthotopic mouse
models that use the unique pharmacokinetic property of nitroxoline
(high accumulation in urinary tract) to their advantage. Therefore,
T24, 5637 and KCC853 urological cancer cell lines were selected for
further in vivo pharmacodynamic analysis.
Effects of nitroxoline on the growth
of urological tumor orthotopic xenografts
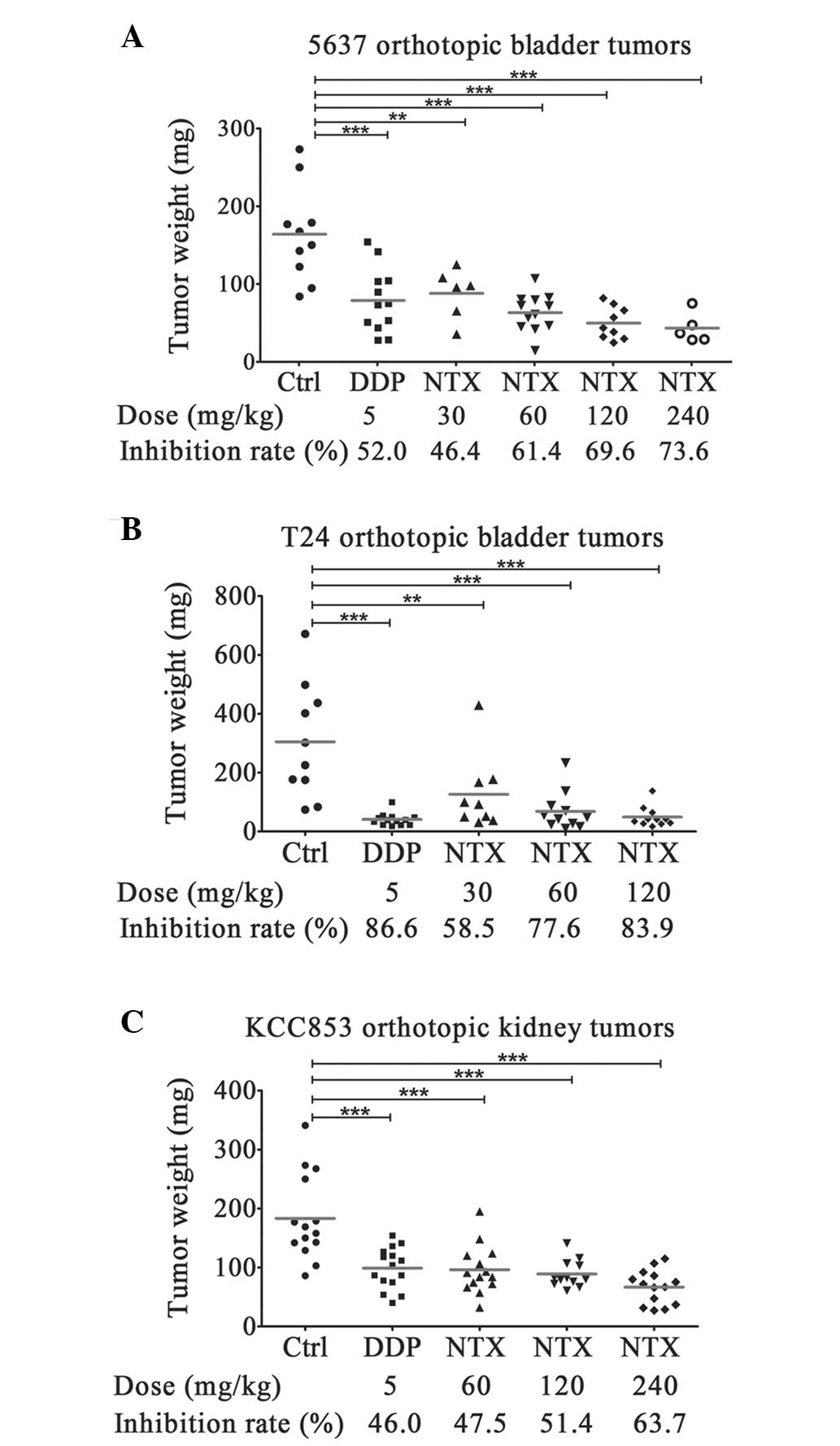
Nitroxoline dose-dependently inhibited the growth of
5637 cell bladder tumor orthotopic xenografts (Fig. 2A; Table
II). The lowest dose (30 mg/kg, twice a day) of nitroxoline
used for cancer treatment in nude mice was equivalent to the common
dose (750 mg/day) used for human UTI treatment, according to
equivalent dose calculation based on the body surface area of
different species (14). This low
dose of nitroxoline (30 mg/kg) resulted in ~46% tumor growth
inhibition compared with the vehicle control. As the dose of
nitroxoline increased, tumor growth inhibition rates demonstrated
corresponding increases and amounted to ~74% at the highest dose of
240 mg/kg. The T24 cell bladder tumor orthotopic xenograft it
exhibited a more sensitive response to nitroxoline treatment
(Fig. 2B; Table III), with as high as 83.9% of growth
inhibition at the dose of 120 mg/kg. Even at the lowest dose (30
mg/kg), nitroxoline significantly inhibited the growth of T24
bladder tumors by 58.5%. The effect on tumor growth was not
specific to bladder tumors; nitroxoline was also effective at
inhibiting the growth of KCC853 cell renal tumor orthotopic
xenografts, resulting in 47.5, 51.4 and 63.7% of growth inhibition
at doses of 60, 120 and 240 mg/kg, respectively (Fig. 2C; Table
IV). Cisplatin, the positive control drug, inhibited the growth
of 5637, T24 and KCC853 orthotopic tumors by 46.4, 86.6 and 46.0%,
respectively, suggesting that the anticancer effects of 5 mg/kg
cisplatin in nude mice were equivalent to that of 60–120 mg/kg
nitroxoline. Taken together, nitroxoline appears to effectively
inhibit the growth of orthotopic urological tumors in a
dose-dependent manner.
 | Table III.Effects of nitroxoline on T24 cell
bladder cancer orthotopic xenografts in nude mice. |
Table III.
Effects of nitroxoline on T24 cell
bladder cancer orthotopic xenografts in nude mice.
|
| Drug
administration | Anti-cancer
activity | Toxicity |
|---|
|
|
|
|
|
|---|
| Drug | Dose, mg/kg | Schedule | Route | Tumor weight,
mga | Inhibition rate,
% | Body weight loss,
%a | Mortalities/total
mice, n |
|---|
| Control | Vehicle | BID for 28
days | p.o. |
304±195 |
|
18.0±2.6 | 4/14 |
| Cisplatin | 5 | QW for 4 weeks | i.v. |
41±21 | 86.6 |
23.1±7.3 | 1/14 |
| Nitroxoline | 30 | BID for 28
days | p.o. |
126±125b | 58.5 |
22.1±5.4 | 5/14 |
| Nitroxoline | 60 | BID for 28
days | p.o. |
69±65c | 77.6 |
16.7±2.6 | 3/14 |
| Nitroxoline | 120 | BID for 28
days | p.o. |
49±35c | 83.9 |
14.3±2.3 | 3/14 |
Toxic effects were concurrently evaluated by mouse
mortality and body weight loss rates. These factors were not
exhibited in a corresponding dose-dependent manner (Tables II–IV). In fact, no significant differences in
mouse mortality and body weight loss rates were observed between
each group, suggesting that these outcomes may not occur as
side-effects of nitroxoline but due to unavoidable factors, such as
postoperative complications or exacerbation of the orthotopic
tumors.
Overall, low doses of nitroxoline (30 mg/kg, twice a
day) were sufficient to significantly inhibit urological tumor
growth in orthotopic mouse models. Higher doses of nitroxoline
(60–240 mg/kg, twice a day) demonstrated obviously enhanced
anticancer efficacy without corresponding increases in
toxicity.
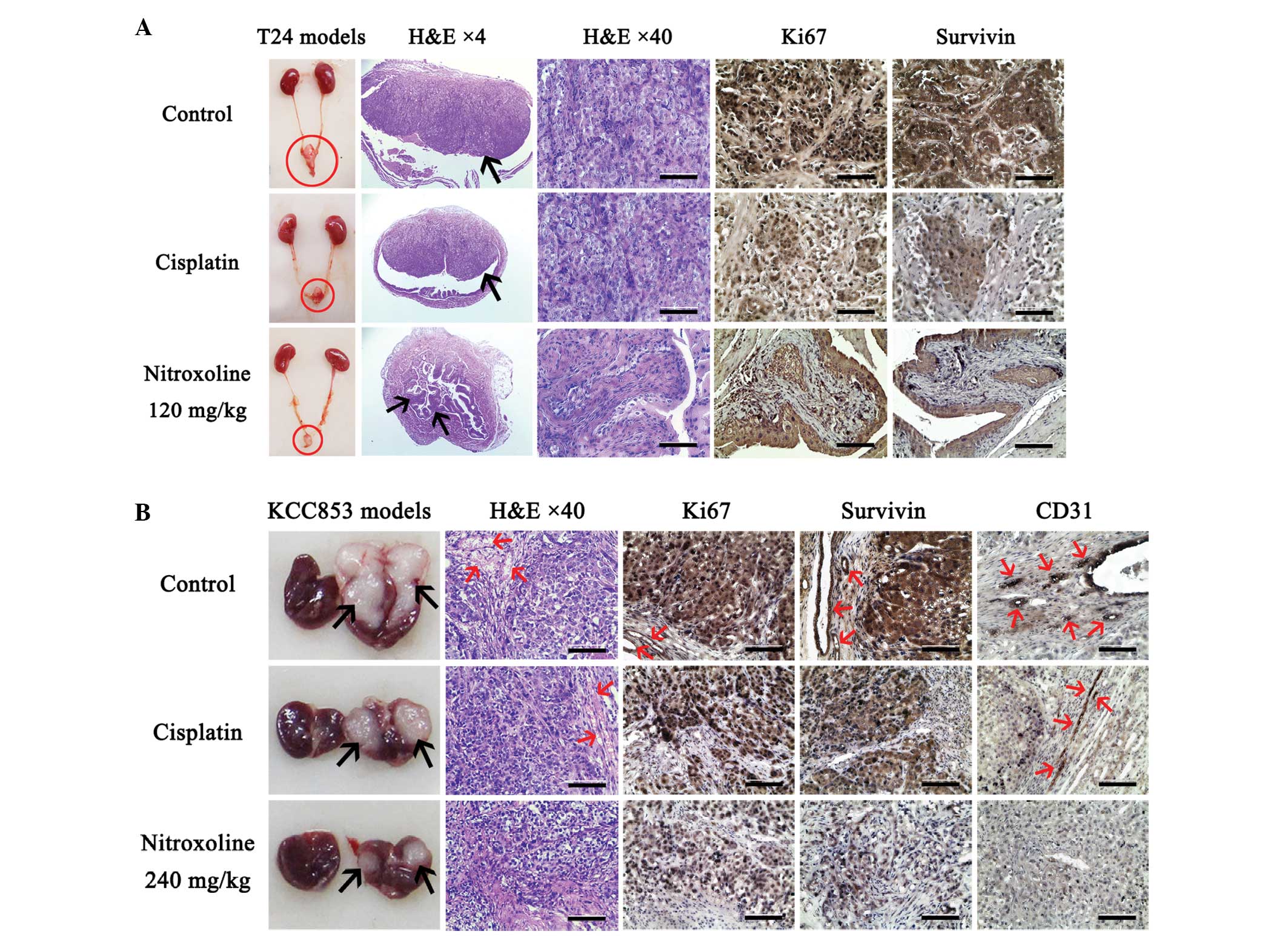
Nitroxoline-treated orthotopic
urological tumors exhibit low proliferative characteristics
Due to the high sensitivity of T24 cells to
nitroxoline treatment in vitro and in vivo (Table I; Fig.
3), further histological analysis and cytotoxic assays were
performed using T24 cells or T24 xenograft tumors. Histological
examination by H&E staining revealed that T24 orthotopic
bladder tumors from the vehicle control and cisplatin groups had
features common in non-papillary urothelial carcinoma (15), characterized by the presence of
neoplastic urothelial nests (Fig.
3A). However, the majority of bladder tumors removed from
nitroxoline-treated mice had features of papillary urothelial
carcinoma (15), showing fused
papillae and disordered architecture (Fig. 3A). Therefore, nitroxoline appears to
significantly delay malignant progression of T24 tumors.
Immunohistochemistry further demonstrated that the nested tumor
cells in control T24 tumors had strong Ki67 (16) and survivin (17) staining, while markedly weaker staining
of both proliferative markers were observed in tumors treated with
cisplatin or nitroxoline (Fig. 3A).
Taken together, the results indicate that nitroxoline may delay the
malignant progression of T24 orthotopic bladder tumors by
inhibiting their proliferative activity.
All the H&E-stained KCC853 orthotopic renal
tumors showed features of clear cell renal cell carcinoma (Fig. 3B) (18).
The difference between each group was the density of microvessels
in the tumors. KCC853 orthotopic tumors of the vehicle control and
cisplatin groups had numerous erythrocyte-filled blood vessels,
while microvessels were rarely observed in the nitroxoline-treated
tumors, particularly tumors in the highest dose (240 mg/kg) group
(Fig. 3B). Immunohistochemistry
further confirmed the inhibitory effect of nitroxoline on
angiogenesis. Ki67 and survivin exhibit strong staining in
proliferative tumor and proliferative endothelial cells; this
strong staining was obviously observed in both cells types of
control KCC853 tumor samples (Fig.
3B). By contrast, cisplatin- and nitroxoline-treated tumors
only demonstrated weak Ki67 and survivin staining in tumor cells,
and no visible staining in endothelial cells (Fig. 3B). Furthermore, immunohistochemical
staining of CD31, a direct marker of blood vessels (19), confirmed that the density of
microvessels was very low in nitroxoline-treated tumors compared
with that in the vehicle control tumors (Fig. 3B). Taken together, the results
indicate that nitroxoline may effectively inhibit angiogenesis and
proliferation of KCC853 orthotopic renal tumors.
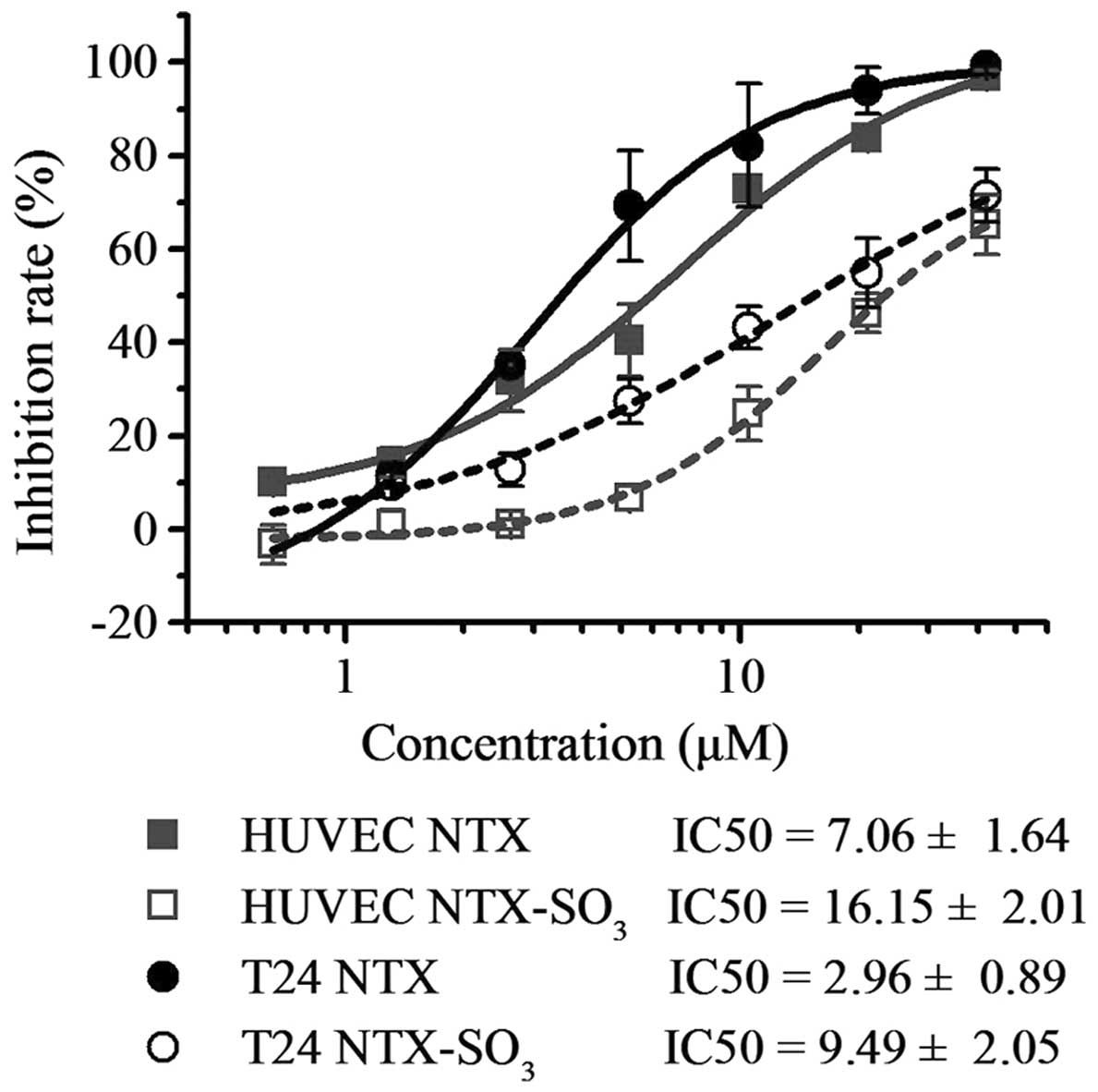
Nitroxoline sulfate, a metabolite of
nitroxoline, also exhibits anticancer activity
Following oral administration, ~99% of the excreted
nitroxoline is eliminated as metabolites in the urine and only 1.0%
is eliminated as the parent component (2,20). Thus,
the present study aimed to determine whether the metabolites of
nitroxoline also exhibit anticancer activity. According to the
relative peak area signals, the two major metabolites of
nitroxoline, nitroxoline sulfate and glucuronide, contribute most
to the urinary excretion of nitroxoline (20). Due to the poor stability of
nitroxoline glucuronide in vitro, it is rarely used the
in vitro evaluation of anticancer activity. However,
nitroxoline sulfate can be successfully collected from the urine of
nitroxoline-treated nude mice with high purity (99%) and good
stability (stable at 37°C for at least 96 h). Thus, the present
study performed an MTT assay using nitroxoline and nitroxoline
sulfate, and demonstrated that nitroxoline sulfate is able to
inhibit the growth of HUVEC and T24 cells, but with ~30% decreases
in the maximum inhibition rates and 2–3-fold increases in
IC50 values compared with its parent drug, nitroxoline.
However, due to the high concentration and excretion levels of
nitroxoline sulfate in the urine (30–60-fold higher than that of
nitroxoline) (20), urinary
nitroxoline sulfate level may be sufficient to inhibit tumor growth
(Fig 4).
Discussion
Drug repurposing, alternatively termed ‘new uses for
old drugs’ or ‘drug repositioning’, has gained considerable
attention over the past decade, and become a powerful alternative
strategy for identifying and developing novel anticancer drugs
(1,7,21). The
majority of non-cancer drugs approved for anticancer treatment have
common features, including well-defined pharmacokinetic and
pharmacodynamics properties, and well-characterized cancer targets
(1,7,21).
Nitroxoline has an excellent safety profile and well-defined
pharmacokinetic properties that have been established through its
50-year clinical history (1,2,6).
Furthermore, its anticancer activity has been demonstrated to be
associated with angiogenesis inhibition by targeting MetAP2 and
sirtuin 1/2 (3), blocking cancer cell
migration and invasion by targeting cathepsin B (6), and directly inducing apoptosis (4). Thus, the most important and imperative
study required to advance nitroxoline repurposing into clinical
trials for anticancer treatment was systemic preclinical
pharmacodynamic evaluation of its anticancer activity. The current
in vitro study compared the sensitivities of various cell
lines to nitroxoline treatment, from which three sensitive cell
lines with urological origins (T24, 5637 and KCC853) were selected
for further in vivo analysis. As expected, nitroxoline
effectively and dose-dependently inhibited the growth of these
urological tumors in orthotopic mouse models. The low dose (30
mg/kg, twice a day) of nitroxoline used in nude mice, equivalent to
the common dose (750 mg/day) used for human UTI treatment,
inhibited the growth of urological xenografts by 40–60%. Higher
dose of nitroxoline (120–240 mg/kg, twice a day) resulted in 50–85%
growth inhibition without corresponding increase in toxicity.
Therefore, the routine nitroxoline administration regimen used for
human UTI treatment was sufficient for urological cancer treatment,
and higher dose of nitroxoline may aid cancer patients with good
general conditions.
In addition, the present study demonstrated that
nitroxoline sulfate, one of the most common metabolites of
nitroxoline in the urine, may effectively inhibit the proliferation
of T24 and HUVEC cells. Sulfate conjugation increases the aqueous
solubility of the parent drug nitroxoline to allow for renal
excretion; however, it decreases the lipid solubility of
nitroxoline, making it difficult for nitroxoline sulfate to pass
across the cell membrane and exhibit its anticancer activity.
Although nitroxoline sulfate demonstrated relatively low anticancer
activity compared with parent drug nitroxoline in the present
study, its high concentration and excretion levels in the urine
(30–60-fold higher than that of nitroxoline) (20) mean that it may be sufficient to
inhibit tumor growth. The results of the present study largely
increased the feasibility of nitroxoline repurposing for clinical
anticancer application, particularly for bladder cancer
treatment.
In summary, the current study demonstrated that
nitroxoline and its metabolite nitroxoline sulfate in the urine
exhibit powerful anti-cancer potential against urological tumors,
and the routine nitroxoline administration regimen for human UTI
treatment appeared to be effective and sufficient for urological
cancer treatment. These results, in addition to the well-known
safety profiles of nitroxoline and well-defined pharmacokinetic
properties, successfully advanced nitroxoline repurposing into a
phase II clinical trial in China for non-muscle invasive bladder
cancer treatment (registration no. CTR20131716).
Acknowledgements
The present study was partially supported by the
National Key Technologies R&D Program for New Drugs (grant no.
2012ZX09301003-001).
References
|
1
|
Shim JS and Liu JO: Recent advances in
drug repositioning for the discovery of new anticancer drugs. Int J
Biol Sci. 10:654–663. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Mrhar A, Kopitar Z, Kozjek F, Presl V and
Karba R: Clinical pharmacokinetics of nitroxoline. Int J Clin
Pharmacol Biopharm. 17:476–481. 1979.PubMed/NCBI
|
|
3
|
Shim JS, Matsui Y, Bhat S, Nacev BA, Xu J,
Bhang HE, Dhara S, Han KC, Chong CR, Pomper MG, et al: Effect of
nitroxoline on angiogenesis and growth of human bladder cancer. J
Natl Cancer Inst. 102:1855–1873. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Lazovic J, Guo L, Nakashima J, Mirsadraei
L, Yong W, Kim HJ, Ellingson B, Wu H and Pope WB: Nitroxoline
induces apoptosis and slows glioma growth in vivo. Neuro Oncol.
17:53–62. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Jiang H, Taggart JE, Zhang X, Benbrook DM,
Lind SE and Ding WQ: Nitroxoline (8-hydroxy-5-nitroquinoline) is
more a potent anti-cancer agent than clioquinol
(5-chloro-7-iodo-8-quinoline). Cancer Lett. 312:11–17. 2011.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mirković B, Renko M, Turk S, Sosič I,
Jevnikar Z, Obermajer N, Turk D, Gobec S and Kos J: Novel mechanism
of cathepsin B inhibition by antibiotic nitroxoline and related
compounds. Chem Med Chem. 6:1351–1356. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Gupta SC, Sung B, Prasad S, Webb LJ and
Aggarwal BB: Cancer drug discovery by repurposing: Teaching new
tricks to old dogs. Trends Pharmacol Sci. 34:508–517. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
8
|
National Research Council: Guide for the
Care and Use of Laboratory Animals (8th). The National Academies
Press. Washington DC: 2011.
|
|
9
|
Hadaschik BA, Black PC, Sea JC, Metwalli
AR, Fazli L, Dinney CP, Gleave ME and So AI: A validated mouse
model for orthotopic bladder cancer using transurethral tumour
inoculation and bioluminescence imaging. BJU Int. 100:1377–1384.
2007. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Kang MR, Yang G, Charisse K,
Epstein-Barash H, Manoharan M and Li LC: An orthotopic bladder
tumor model and the evaluation of intravesical saRNA treatment. J
Vis Exp pii. 4207:2012
|
|
11
|
Zhao H, Nolley R, Chen Z and Peehl DM:
Tissue slice grafts: An in vivo model of human prostate androgen
signaling. Am J Pathol. 177:229–239. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Thong AE, Zhao H, Ingels A, Valta MP,
Nolley R, Santos J, Young SR and Peehl DM: Tissue slice grafts of
human renal cell carcinoma: An authentic preclinical model with
high engraftment rate and metastatic potential. Urol Oncol.
32:43.e23–e30. 2014. View Article : Google Scholar
|
|
13
|
Murugasu-Oei B and Dick T: In vitro
activity of the chelating agents nitroxoline and oxine against
Mycobacterium bovis BCG. Int J Antimicrob Agents. 18:579–582. 2001.
View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Reagan-Shaw S, Nihal M and Ahmad N: Dose
translation from animal to human studies revisited. FASEB J.
22:659–661. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Montironi R and Lopez-Beltran A: The 2004
WHO classification of bladder tumors: A summary and commentary. Int
J Surg Pathol. 13:143–153. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Santos L, Amaro T, Costa C, Pereira S,
Bento MJ, Lopes P, Oliveira J, Criado B and Lopes C: Ki-67 index
enhances the prognostic accuracy of the urothelial superficial
bladder carcinoma risk group classification. Int J Cancer.
105:267–272. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Shariat SF, Ashfaq R, Karakiewicz PI,
Saeedi O, Sagalowsky AI and Lotan Y: Survivin expression is
associated with bladder cancer presence, stage, progression, and
mortality. Cancer. 109:1106–1113. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Lopez-Beltran A, Scarpelli M, Montironi R
and Kirkali Z: 2004 WHO classification of the renal tumors of the
adults. Eur Urol. 49:798–805. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Albelda SM, Muller WA, Buck CA and Newman
PJ: Molecular and cellular properties of PECAM-1 (endoCAM/CD31): A
novel vascular cell-cell adhesion molecule. J Cell Biol.
114:1059–1068. 1991. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Wagenlehner FM, Münch F, Pilatz A, Bärmann
B, Weidner W, Wagenlehner CM, Straubinger M, Blenk H, Pfister W,
Kresken M and Naber KG: Urinary concentrations and antibacterial
activities of nitroxoline at 250 milligrams versus trimethoprim at
200 milligrams against uropathogens in healthy volunteers.
Antimicrob Agents Chemother. 58:713–721. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Boguski MS, Mandl KD and Sukhatme VP: Drug
discovery. Repurposing with a difference. Science. 324:1394–1395.
2009. View Article : Google Scholar : PubMed/NCBI
|