Introduction
Retroperitoneal tumors are rare lesions with diverse
pathological subtypes, which originate from the retroperitoneal
space (1). In total, ~40% of
retroperitoneal tumors are benign (2). Benign retroperitoneal tumors are
slow-growing and typically lack a specific clinical manifestation.
The primary characteristic of this lesion is the compression of the
tumor surroundings, therefore, early diagnosis is often difficult
(3). Pre-operative diagnosis
predominantly relies on imaging techniques, including enhanced
computed tomography (CT) and magnetic resonance imaging (4). Retroperitoneal tumors often surround and
associate with vital abdominal organs and blood vessels, thus,
performing a complete surgical resection is challenging (5). Nevertheless, follow-up data from
previous studies have demonstrated that patients who have undergone
a complete resection have significantly higher 1-, 3- and 5-year
survival rates than those who have undergone an incomplete
resection. Therefore, the resection rate significantly impacts the
post-operative local recurrence rate and prognosis (6). Even if a retroperitoneal tumor is
diagnosed as benign, if it is not removed completely then the tumor
may result in the compression of abdominal organs, tissues, blood
vessels and nerves, followed by continual tumor growth and possible
fatality (7). Certain researchers
consider the invasion of benign retroperitoneal tumors into the
surrounding abdominal blood vessels and organs to be an independent
limiting factor for their complete surgical resection (8). Given that such lesions are more likely
to surround, rather than infiltrate, abdominal vascular walls, the
present study designed a novel surgical approach, known as the
fractionation approach. This approach resulted in the fractionation
and subsequent complete resection of a giant benign retroperitoneal
tumor that surrounded major blood vessels, including the celiac
axis and the splenic, common hepatic and superior mesenteric
arteries, and was closely associated with the abdominal aorta and
the portal, splenic, superior mesenteric and left renal veins.
During this technique, the important retroperitoneal blood vessels
were protected effectively.
Case report
A 21-year-old man was admitted to The First
Affiliated Hospital of Chongqing Medical University (Chongqing,
China) in March 2013 presenting with a mass in the pancreatic head
region that had been identified during a physical examination 9
months previously. The patient also complained of subxiphoid
discomfort for >1 month. A total of 9 months prior to admission,
the patient had undergone abdominal ultrasonography at another
hospital, which resulted in the detection of a mass measuring
~6.5×4.5 cm, located in the pancreatic head region and the first
hepatic hilum. As the mass was asymptomatic, the patient did not
undergo treatment. Furthermore, 1 month prior to admission,
paroxysmal pain and discomfort was experienced below the xiphoid,
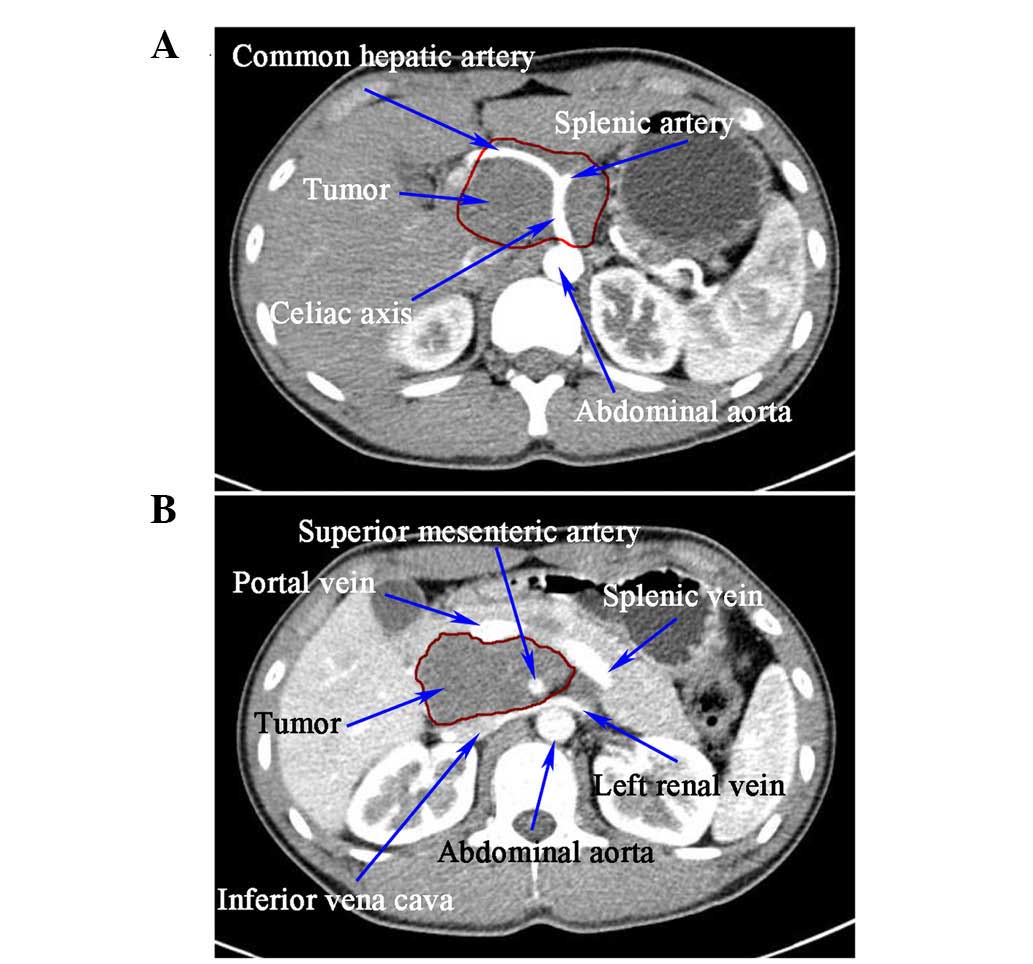
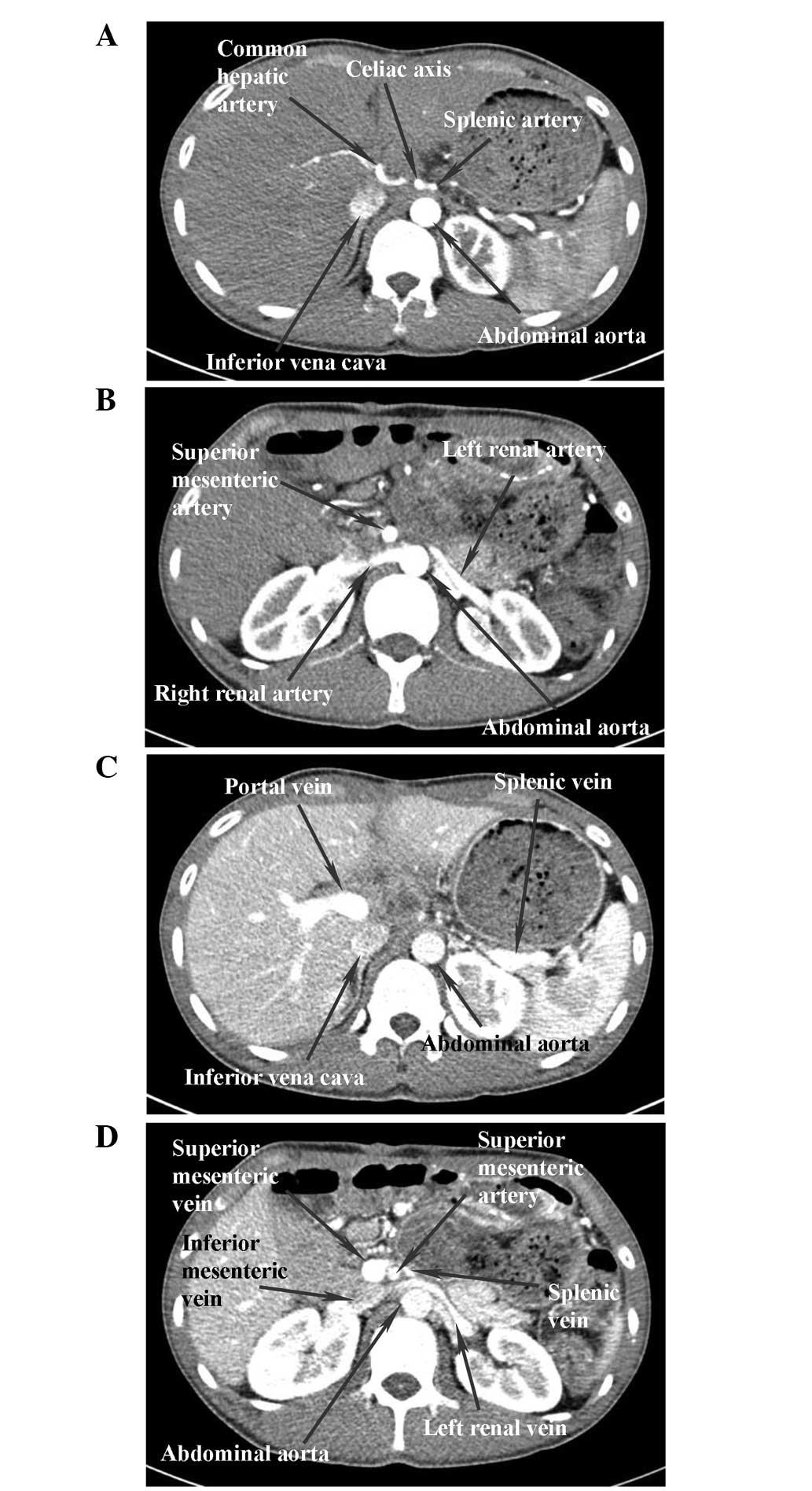
and abdominal enhanced CT (SOMATOM® Definition Flash
Dual Source CT Scanner; Siemens AG, Munich, Germany) identified a
mass ~7.2×4.3×7.5 cm in size located in the rear of the pancreatic
head and body. The tumor completely surrounded the celiac axis and
the splenic, common hepatic and superior mesenteric arteries, and
was closely associated with the abdominal aorta and the portal,
splenic, superior mesenteric and left renal veins. Additionally,
the mass invaded the pancreatic head and compressed the pancreatic
body (Fig. 1). Pre-operative CT also
indicated the presence of a benign tumor, which was diagnosed as
benign since the tumor had a clear margin, smooth surface,
symmetrical density and a blood supply, the lymph nodes surrounding
the tumor were not enlarged and the abdominal blood vessels did not
have a filling defect. An intraoperative frozen biopsy confirmed
the diagnosis of a benign tumor. Subsequently, a retroperitoneal
tumor resection and a pancreaticoduodenectomy were performed.
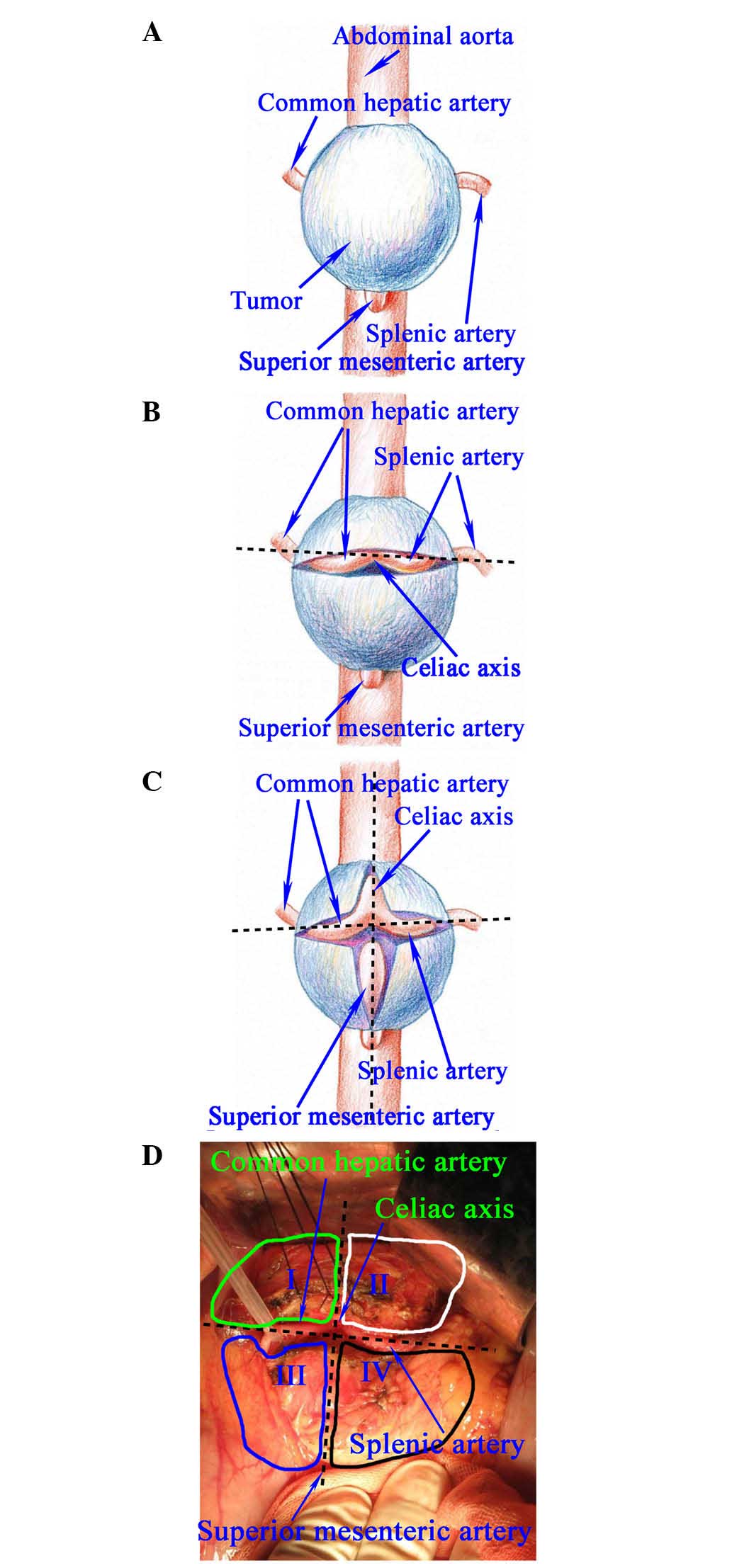
The tumor was exposed during surgery and 0.6×0.6 cm
of tissue was removed as an intraoperative frozen biopsy sample,
which was later established to be benign. The association between
the tumor and its surrounding structures was analyzed. It was
observed that the lesion completely surrounded the celiac axis and
the splenic, common hepatic and superior mesenteric arteries, and
was closely associated with the splenic, portal and left renal
veins, and the abdominal aorta (Fig.
2A). The lesion, however, could not be separated from the head
of the pancreas. Therefore, a fractionated resection of the tumor
was performed, as well as a pancreaticoduodenectomy. The gastric
antrum and the pancreatic neck were severed, and the splenic,
portal and superior and inferior mesenteric veins were isolated.
The tumor, which was located behind the pancreas and the
aforementioned veins, was now fully exposed. Bounded by the splenic
and common hepatic arteries, the tumor was divided into upper and
lower fractions (Fig. 2B). The tumor
was incised according to the courses of the common hepatic and
splenic arteries, which were then exposed to the celiac axis, and
the left gastric artery was severed. Also bounded by the celiac
axis and the superior mesenteric artery, the tumor mass was further
divided into left and right fractions (Fig. 2C). The tumor was incised according to
the courses of the celiac axis and the superior mesenteric artery.
Subsequently, the celiac axis and superior mesenteric artery were
exposed to the surface of the abdominal aorta. The tumor fractions
were resected separately in the following sequence: Upper right,
lower right, upper left and lower left (Fig. 2C and D). The important blood vessels
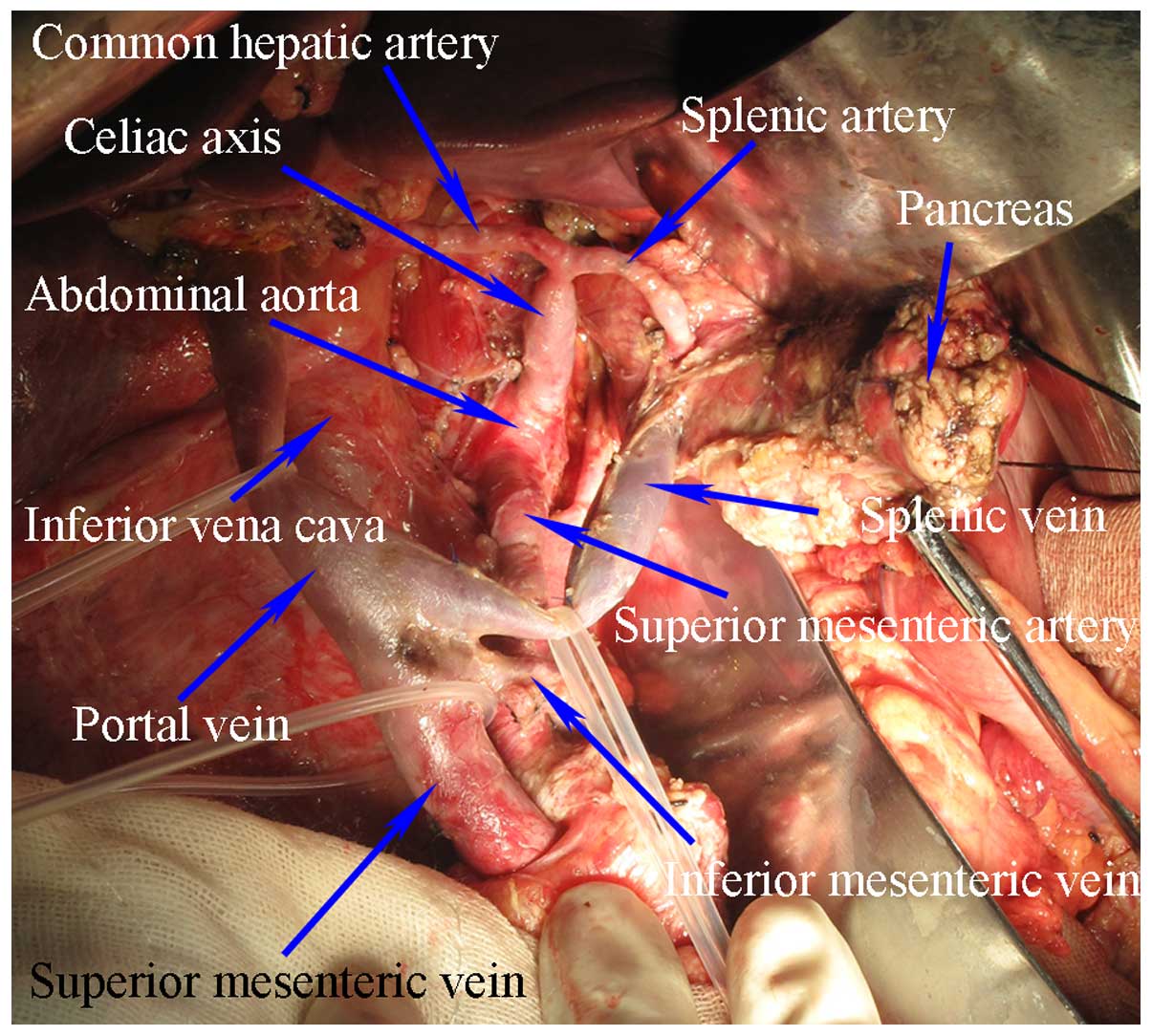
were protected sufficiently (Fig. 3).
The remaining pancreaticoduodenectomy steps were performed in a
routine manner.
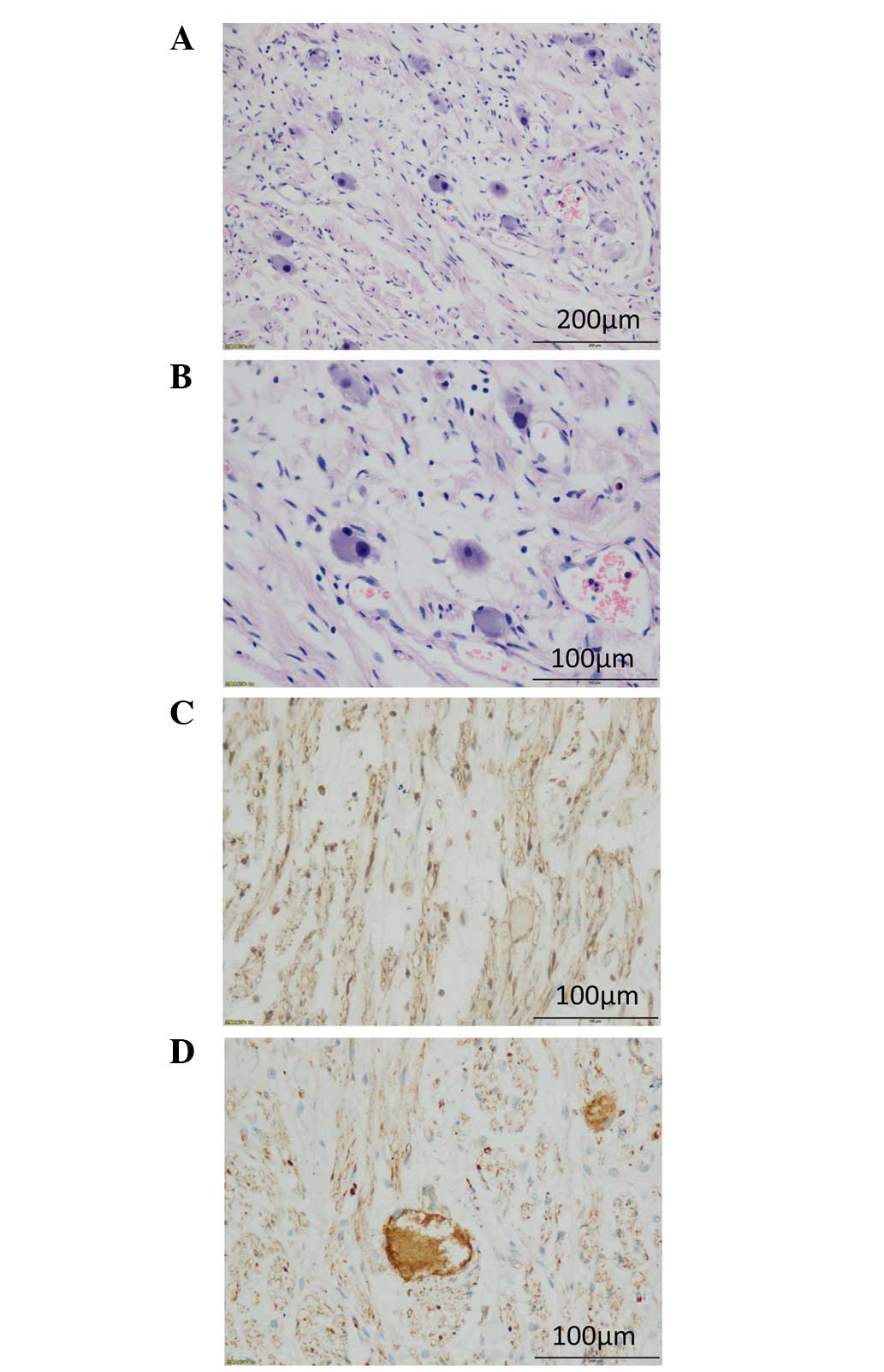
Pathological analysis identified that the neoplasm
was composed of numerous scattered, mature ganglion cells (Fig. 4A and B). No association was observed
at the junction of the pancreas and intestine, or near the resected
margin of the pancreas and intestine. Immunohistochemical staining
exhibited a positive S100 reaction in the membrane of the ganglion
cells fibers (Fig. 4C), whereas the
cytoplasm of the ganglion cells reacted strongly with synaptophysin
(Fig. 4D). Immunohistochemistry was
performed by the Clinical Pathological Diagnosis Center of
Chongqing Medical University (Chongqing, China).
The patient was followed up for a year and a half,
and appeared to be in a good condition without discomfort. An
abdominal CT scan demonstrated no tumor recurrence, whilst the
celiac axis and splenic, common hepatic and superior mesenteric
arteries, and the abdominal aorta were intact, and the superior
mesenteric and portal veins were patent (Fig. 5).
Written informed consent was obtained from the
patient prior to the publication of the present study.
Discussion
Retroperitoneal tumors are lesions that originate
from the retroperitoneal space, presenting with diverse
pathological subtypes (1,9). Of all retroperitoneal tumors, benign
tumors account for ~40% (2,10). Benign retroperitoneal tumors have a
wide range with regard to age of onset, with the lesions typically
growing slowly and exhibiting no symptoms at the early stages
(9,11–13).
Patients frequently seek treatment due to experiencing chronic
abdominal pain and bloating, resulting from compression of the
surrounding tissues by larger tumors (9,14). By the
time a diagnosis is reached, tumors may have already surrounded and
invaded important abdominal blood vessels, subsequently making a
complete surgical resection difficult (5). Furthermore, surgery may easily lead to
the injury of vital organs and blood vessels, as well as multiple
post-operative complications. Nevertheless, if benign tumors are
resected incompletely, post-operative recurrence and tumor regrowth
may lead to a similar outcome as observed with malignancies, and
may ultimately lead to fatality (7).
Therefore, the search for a surgical approach that allows complete
resection of a tumor, whilst protecting important blood vessels,
tissues and organs, appears to be necessary.
Benign retroperitoneal tumors are slow-growing and
non-invasive (12). Such lesions
typically surround and compress major blood vessels close to the
abdominal cavity, rather than directly infiltrating or damaging the
vascular walls, as observed in malignancies. Furthermore, in benign
retroperitoneal tumors, there is typically little concern regarding
tumor implantation and metastasis resulting from tumor rupture
during surgical resection. Thus, the implementation of a complete
resection of these benign tumors is made possible using the
fractionation approach, according to the orientation of the major
retroperitoneal blood vessels, which surround important abdominal
blood vessels.
The present study reviewed the literature of the
recent decades regarding the surgical treatment of retroperitoneal
tumors. Only a small number of studies reported and discussed this
method for the resection of such lesions (5,13). Certain
studies have described cases of laparoscopic resection of
retroperitoneal tumors. Ahn et al (15) described a laparoscopic approach for
the resection of retroperitoneal tumors, which had the advantages
of minimal damage to surrounding tissues, reduced bleeding and
fewer complications compared with traditional open dissection
(13,15–17).
However, in the case of larger tumors, severe intraperitoneal
adhesions or hemorrhages, laparoscopic surgery may face
limitations, particularly when treating retroperitoneal tumors that
surround and invade major blood vessels within the abdominal cavity
(3,17). Subsequently, a traditional open
dissection becomes necessary.
Kariya et al (18) described the use of radiofrequency
ablation followed by injections of carbon dioxide (CO2)
between the retroperitoneal tumor capsule and the adjacent tissues
and organs. The principle of such injections is that CO2
serves an important role in thermal isolation, which may prevent
thermal injury to the surrounding tissues during radiofrequency
ablation. However, this method does present with limitations when
the tumors are surrounding important abdominal blood vessels,
particularly multiple abdominal vessels at numerous locations.
Furthermore, a percutaneous injection of CO2 is
difficult to execute, and has the potential to cause heavy bleeding
or air embolization. CO2 embolization, caused by
laparoscopic surgery, has been previously reported (19). Therefore, the effectiveness of the
surgical procedure remains controversial.
Regarding retroperitoneal tumors that invade
important abdominal blood vessels, the literature describes a
different treatment using combined major vascular resection. For
example, Fueglistaler et al (8) noted a combined approach using a partial
vascular resection and revascularization for the treatment of
retroperitoneal tumors that had invaded the abdominal blood
vessels. However, this approach has its own limitations, including
a risk of heavy bleeding during vascular resection and prosthetic
vessel replacement. Intraoperative arterial occlusion may result in
ischemia and hypoxia in corresponding tissues and organs, whilst
venous occlusion may result in distal tissue and organ congestion.
Multiple studies have demonstrated that if hepatic vascular
occlusion is experienced for >60 min, this contributes to the
risk of post-operative liver failure (11,20). If
complete renal artery occlusion is encountered for a period of 30
min, this may affect the post-operative renal function of patients
(11,21–25).
Prolonged renal artery occlusion may cause renal failure, pale
hypertension and kidney necrosis, whilst mesenteric vessel
occlusion may cause bowel necrosis. Regarding vascular
replacement-associated complications, the incidence of early
complications following vena cava replacement is ~44%, which
includes intraoperative coagulation disorders, prosthetic clogging
and prosthetic infection, possibly leading to fatality (8). In the study by Fueglistaler et al
(8), it was reported that the early
complication rate subsequent to aorta and vena cava replacement,
performed using different vascular replacement approaches, remained
at 19%. Therefore, combined vascular resection and replacement
approaches have their drawbacks. Nevertheless, such approaches are
considered to be the only methods of treatment for advanced tumors,
particularly malignant tumors that exhibit vascular invasion
(8). The surgical approach for the
treatment of benign retroperitoneal tumors presenting with vascular
invasion should be successful in fully removing the tumors, whilst
effectively protecting blood vessels; therefore, the surgical
approach may significantly lower the incidence of post-operative
complications and reduce the cost of surgery.
The treatment of tumors associated with
retroperitoneal blood vessels, and even organs, using traditional
methods may inflict greater risks and difficulties when conducting
the surgery due to their vascular invasion. In particular,
important retroperitoneal organs (including the liver, spleen,
pancreas), and even blood vessels (such as the celiac artery and
vein), may affect the safety of surgery when it is subsequent to
injury, possibly leading to severe bleeding and decreased patient
survival (26). Similarly, injury to
specific blood vessels, including the renal artery, may cause
uncontrolled hypertension (26) and
an increasing risk of perioperative cardiocerebral events.
Furthermore, this may lead to multiple post-operative complications
and possibly affect the prognosis and quality of life of
patients.
When considering the fractionated resection approach
for tumors that surround blood vessels, identification of the
status of important abdominal blood vessels that have been invaded
by the tumor is required. Subsequently, the tumor should be divided
into different areas, according to the blood vessels that surround
the lesion and serve as guidelines. Finally, the tumor may be
resected separately and completely. This method does not only
expose and protect important abdominal blood vessels, lower the
risk of severe bleeding caused by major abdominal vascular injury
and reduce post-operative complications, but it is also conducive
to a complete resection of the tumor. In the present case, the
retroperitoneal tumor was ~7.2×4.3×7.5 cm in size, completely
surrounded the celiac axis and the common hepatic, splenic and
superior mesenteric arteries, and was also closely associated with
the abdominal aorta and portal, superior mesenteric, splenic and
left renal veins. Complete surgical resection was, however,
challenging. Pre-operative CT and the intraoperative frozen biopsy
indicated the presence of a benign tumor. Using the fractionation
approach, a straight line was made along the direction of the
common hepatic and splenic arteries, which subsequently divided the
tumor into upper and lower fractions. The tumor was then incised
between the upper and lower fractions, and the celiac axis was
gradually exposed according to the direction of the common hepatic
and splenic arteries. Following this, the tumor was divided into
left and right fractions along the direction of the celiac axis and
the superior mesenteric artery. The tumor was then incised between
the left and right fractions, and the abdominal aorta was gradually
exposed whilst attention was paid to protect the celiac axis and
superior mesenteric artery. At this point, the tumor was divided
into four fractions, namely the upper right, lower right, upper
left and lower left. The lesion was then resected separately whilst
the important abdominal blood vessels (including the celiac axis,
and the common hepatic, splenic and superior mesenteric arteries)
were preserved (Fig. 2). Benign
tumors that surround and invade blood vessels in other areas of the
abdomen should also be able to be resected in a similar manner
using the fractionation approach, whilst maximizing the protection
of important blood vessels.
The fractionation approach is specifically designed
for benign retroperitoneal tumors surrounding important abdominal
blood vessels. Regarding retroperitoneal malignancies, fractionated
resection runs the risk of tumor rupture, implantation and
metastasis. Similarly, malignancies are prone to directly
infiltrate and grow into the vascular walls, therefore limiting the
likelihood of achieving radical resection. At this time,
combination with vascular resection or replacement may be likely to
improve the patient survival rate (5).
In conclusion, fractionated resection of benign
retroperitoneal tumors may protect the invaded, surrounding blood
vessels, whilst also achieving a complete radical resection. In the
present case, no recurrence was observed during a year and a half
of follow-up, with the invaded, surrounding blood vessels being
preserved.
Acknowledgements
This study received a grant from the Chongqing
Science and Technology Commission (grant no., cstc2012jjA0313).
References
|
1
|
Strauss DC, Hayes AJ and Thomas JM:
Retroperitoneal tumours: Review of management. Ann R Coll Surg
Engl. 93:275–280. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Nakashima J, Ueno M, Nakamura K, Tachibana
M, Baba S, Deguchi N, Tazaki H and Murai M: Differential diagnosis
of primary benign and malignant retroperitoneal tumors. Int J Urol.
4:441–446. 1997. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Hanaoka M, Hashimoto M, Sasaki K, Matsuda
M, Fujii T, Ohashi K and Watanabe G: Retroperitoneal cavernous
hemangioma resected by a pylorus preserving
pancreaticoduodenectomy. World J Gastroenterol. 19:4624–4629. 2013.
View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Taskin HE and Berber E: Retroperitoneal
tumors that may be confused as adrenal pathologies. J Surg Oncol.
106:600–603. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Tseng WW, Wang SC, Eichler CM, Warren RS
and Nakakura EK: Complete and safe resection of challenging
retroperitoneal tumors: Anticipation of multi-organ and major
vascular resection and use of adjunct procedures. World J Surg
Oncol. 9:1432011. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Xu YH, Guo KJ, Guo RX, Ge CL, Tian YL and
He SG: Surgical management of 143 patients with adult primary
retroperitoneal tumor. World J Gastroenterol. 13:2619–2621. 2007.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Nogami M, Hoshi T, Toukairin Y, Arai T,
Uozaki H and Fukusato T: A case of the large retroperitoneal
solitary fibrous tumor. Leg Med (Tokyo). 15:19–22. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Fueglistaler P, Gurke L, Stierli P, Obeid
T, Koella C, Oertli D and Kettelhack C: Major vascular resection
and prosthetic replacement for retroperitoneal tumors. World J
Surg. 30:1344–1349. 2006. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Virseda Rodríguez JA, Donate Moreno MJ,
Pastor Navarro H, Carrión López P, Martínez Ruiz J, Martínez
Sanchiz C and Perán Teruel M: Primary retroperitoneal tumors:
Review of our 10-year case series. Arch Esp Urol. 63:13–22.
2010.PubMed/NCBI
|
|
10
|
Egawa S, Satoh T, Suyama K, Uchida T,
Iwabuchi K and Koshiba K: Giant retroperitoneal cyst in an adult
male. Int J Urol. 3:304–306. 1996. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Shindo S, Motohashi S, Katsu M, Kaga S,
Inoue H, Matsumoto M, Kono K, Fujii H and Takeda M: Treatment of
abdominal malignancy invading the vena cava: A report of seven
cases. Surg Today. 37:685–689. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Strauss DC, Qureshi YA, Hayes AJ and
Thomas JM: Management of benign retroperitoneal schwannomas: A
single-center experience. Am J Surg. 202:194–198. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Wei TC, Chung HJ, Lin AT and Chen KK:
Robot-assisted laparoscopic excision of a retroperitoneal paracaval
tumor. J Chin Med Assoc. 76:724–726. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Navin P, Meshkat B, McHugh S, Beegan C,
Leen E, Prins H and Aly S: Primary retroperitoneal mucinous
cystadenoma - A case study and review of the literature. Int J Surg
Case Rep. 3:486–488. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Ahn KS, Han HS, Yoon YS, Kim HH, Lee TS,
Kang SB and Cho JY: Laparoscopic resection of nonadrenal
retroperitoneal tumors. Arch Surg. 146:162–167. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Lehrfeld T, Natale R, Sharma S, Mendoza
PJ, Li Schwab CW and Lee DI: Robot-assisted excision of a
retroperitoneal mass between the left renal artery and vein. JSLS.
14:447–449. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Zhang Z and Xiu D: Laparoscopic surgery
for primary retroperitoneal tumors: A single institution experience
of 14 cases. Surg Laparosc Endosc Percutan Tech. 20:399–403. 2010.
View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Kariya S, Tanigawa N, Kojima H, Komemushi
A, Shomura Y, Ueno Y, Shiraishi T and Sawada S: Radiofrequency
ablation combined with CO2 injection for treatment of
retroperitoneal tumor: Protecting surrounding organs against
thermal injury. AJR Am J Roentgenol. 185:890–893. 2005. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Park EY, Kwon JY and Kim KJ: Carbon
dioxide embolism during laparoscopic surgery. Yonsei Med J.
53:459–466. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
20
|
Huguet C, Gavelli A, Chieco PA, Bona S,
Harb J, Joseph JM, Jobard J, Gramaglia M and Lasserre M: Liver
ischemia for hepatic resection: Where is the limit? Surgery.
111:251–259. 1992.PubMed/NCBI
|
|
21
|
Kowalczyk KJ, Alemozaffar M, Hevelone ND,
Ulmer WD, Plaster BA, Lipsitz SR, Yu HY and Hu JC: Partial clamping
of the renal artery during robot-assisted laparoscopic partial
nephrectomy: Technique and initial outcomes. J Endourol.
26:469–473. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Shao P, Qin C, Yin C, Meng X, Ju X, Li J,
Lv Q, Zhang W and Xu Z: Laparoscopic partial nephrectomy with
segmental renal artery clamping: Technique and clinical outcomes.
Eur Urol. 59:849–855. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Shao P, Tang L, Li P, Xu Y, Qin C, Cao Q,
Ju X, Meng X, Lv Q, Li J, et al: Application of a vasculature model
and standardization of the renal hilar approach in laparoscopic
partial nephrectomy for precise segmental artery clamping. Eur
Urol. 63:1072–1081. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Gill IS, Eisenberg MS, Aron M, Berger A,
Ukimura O, Patil MB, Campese V, Thangathurai D and Desai MM: ‘Zero
ischemia’ partial nephrectomy: Novel laparoscopic and robotic
technique. Eur Urol. 59:128–134. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Gong EM, Zorn KC, Orvieto MA, Lucioni A,
Msezane LP and Shalhav AL: Artery-only occlusion may provide
superior renal preservation during laparoscopic partial
nephrectomy. Urology. 72:843–846. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Jones VS and Burns CR: Operative
considerations in pediatric retroperitoneal teratomas - a review.
Eur J Pediatr Surg. 23:265–269. 2013.PubMed/NCBI
|