Introduction
Biliary tract cancers have a median survival rate of
4.8 months with a 1- and 5-year survival rate of 31 and 10%
respectively (1). A diagnosis is
often made at an advanced disease stage in patients with malignant
biliary obstruction (2). Such
malignancies are known to be unresectable and have a poor
prognosis. For patients with a life expectancy of >3 months,
self-expandable metal stents are deployed (3); however, occlusion of these stents has
been reported in 50% of patients within 6 months of deployment
(2). The relatively high failure rate
is attributed to tumor in- and overgrowth, epithelial hyperplasia,
biofilm deposition, debris formation and sludge buildup.
Furthermore, covered nitinol metal stents have shown an inability
to increase stent patency or patient survival time (4). Photodynamic therapy (PDT) is not a
common treatment option for biliary tract cancers, but it is a
novel palliative therapy that may have a direct effect on the local
tumor within the bile duct lumen with promising results for the
maintenance of biliary drainage (3).
However, the availability, photosensitivity and procedural cost of
PDT is limited, and the procedure necessitates repeated treatment
sessions (5). In addition, a recent
multicenter, randomized phase III study demonstrated that patients
that received PDT with stenting had a 61% excess mortality risk
with a poorer overall survival compared with patients that received
stenting alone (3).
Recently, intraductal radiofrequency ablation (RFA)
has become a beneficial therapeutic option against malignant
biliary obstruction. Clinical studies by Steel et al
(2) and Mizandari et al
(6) demonstrated the safety of
endobiliary RFA treatment, with asymptomatic biochemical
pancreatitis, cholangitis and pain recognized as the only common
complications; however, in the present study, RFA caused biliary
tract perforation, a previously unreported complication that can
result in serious infection, peritonitis and even mortality.
Case report
Case 1
A 67-year-old male presented with a biliary
obstruction with symptoms that consisted of icteric scelra, fever,
fatigue, chills, anorexia, nausea, vomiting and elevated blood
bilirubin at Beijing Chaoyang Hospital (Beijing, China) in May
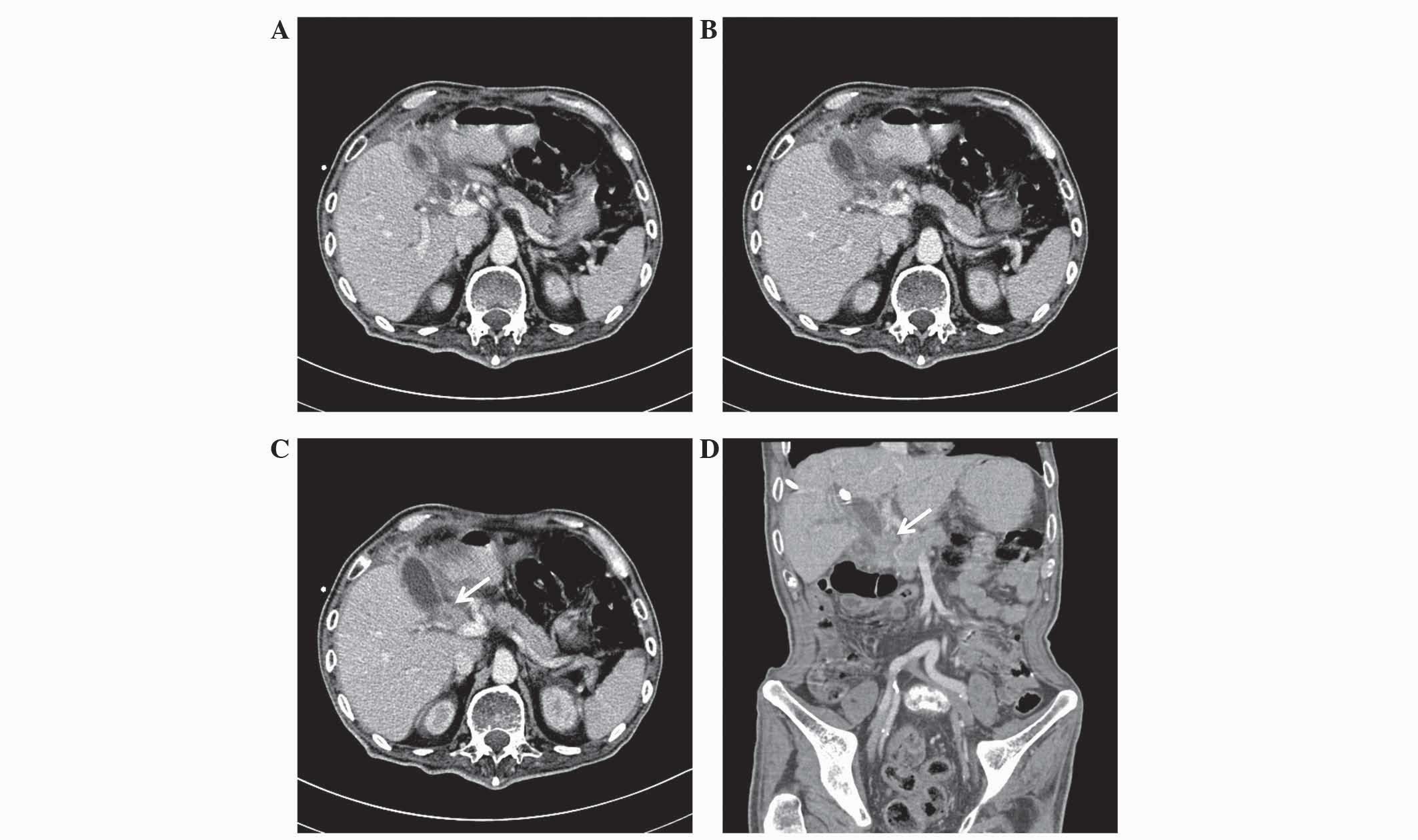
2013. Contrast-enhanced computed tomography (CT) revealed a
space-occupying lesion in the extrahepatic bile duct (Fig. 1). The patient was diagnosed with
cholangiocarcinoma based on the symtoms and imaging. An exploratory
laparotomy was performed in May 2013 at the Cancer Hospital of
Chinese Academy of Medical Sciences (Beijing, China), which
revealed that it was an unresectable malignant biliary tumor.
Therefore, percutaneous transhepatic biliary drainage was conducted
to relieve the obstructive jaundice, which decreased the total
bilirubin from 352 to 78 mmol/l (normal range, 0–20 mmol/l).
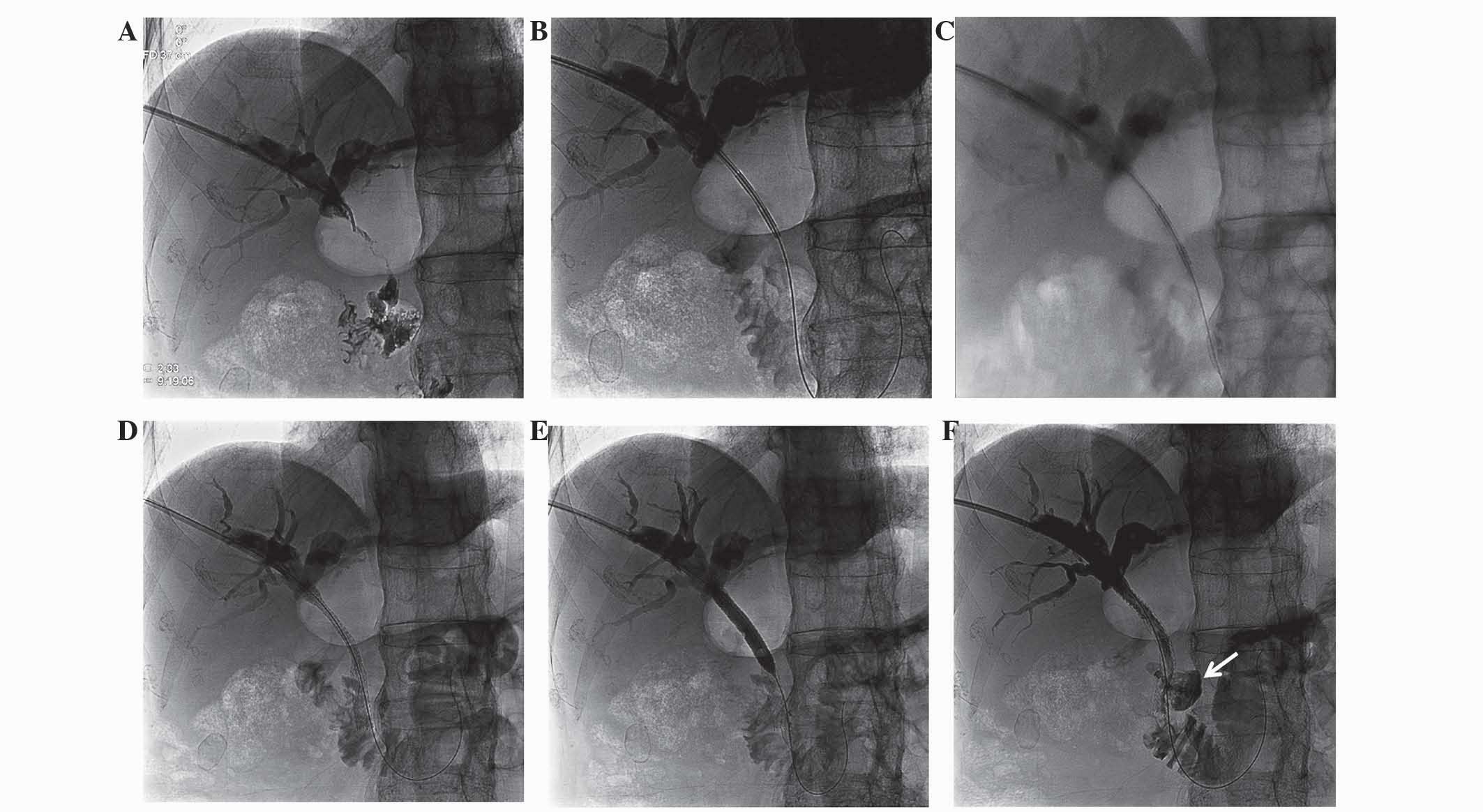
After obtaining informed consent from the patient,
percutaneous intraductal RFA was performed on December 3, 2013,
using an 8 Fr percutaneous endobiliary RFA catheter (Habib;
EMcision Ltd., London, UK) placed using a guidewire from the distal
segment of the common bile duct to the proximal segment of the
common hepatic duct (Fig. 2A–C). RFA
was applied for 2 min at 10 W to two sections of stricture within
the biliary duct sections with a 1-min rest period in-between. An
8×80-mm Zilver self-expanding metal stent (ZIV6-80-8-8.0; Cook
Inc., Bloomington, IN, USA) was then deployed in the stenosis
section of the bile duct and inflated using an 8×40-mm dilatation
balloon catheter (ATB5-35-40-8-4.0; Cook Inc.) (Fig. 2D and E). Percutaneous transhepatic
cholangiography (PTC) was performed in which the contrast agent
overflowed to the outside of the biliary duct, confirming the
diagnosis of biliary tract perforation (Fig. 2F). The patient, however, also
presented with melena the following day. Despite the application of
various treatments, such as blood transfusion (1,400 ml), fluid
infusion (1,500 ml/day; consisting of amino acids, lipid emulsion,
glucose, sodium chloride, water, vitamins and potassium chloride)
and anti-infection therapies (cefoxitin sodium injection, 2 g 3
times/day for 12 days), the patient succumbed on December 15,
2013.
Case 2
A 61-year-old male with obstructive jaundice was
diagnosed with pancreatic carcinoma at Beijing Chaoyang Hospital in
October 2013, based on the symptoms, laboratory findings and
imaging manifestations that were exhibited by the patient. Symptoms
consisted of weakness, anorexia and icteric scelra; laboratory
examination revealed elevated blood bilirubin (257 mmol/l) and
tumor marker cancer antigen 19–9 (2,687 U/ml; normal range, 0–39
U/ml); and an abdominal CT scan revealed a space-occupying lesion
in the head of pancreas with dilation of the extra- and
intrahepatic biliary duct. The patient had undergone a surgical
resection for esophagocardial cancer 3 months previously at the
Cancer Hospital of Chinese Academy of Medical Sciences. Due to the
patient's poor physical condition [Karnofsky performance status
score, 70 (7)], microinvasive
treatment with interventional radiology was considered the best
option. Percutaneous transhepatic biliary drainage was conducted to
relieve the obstructive jaundice, which decreased the total
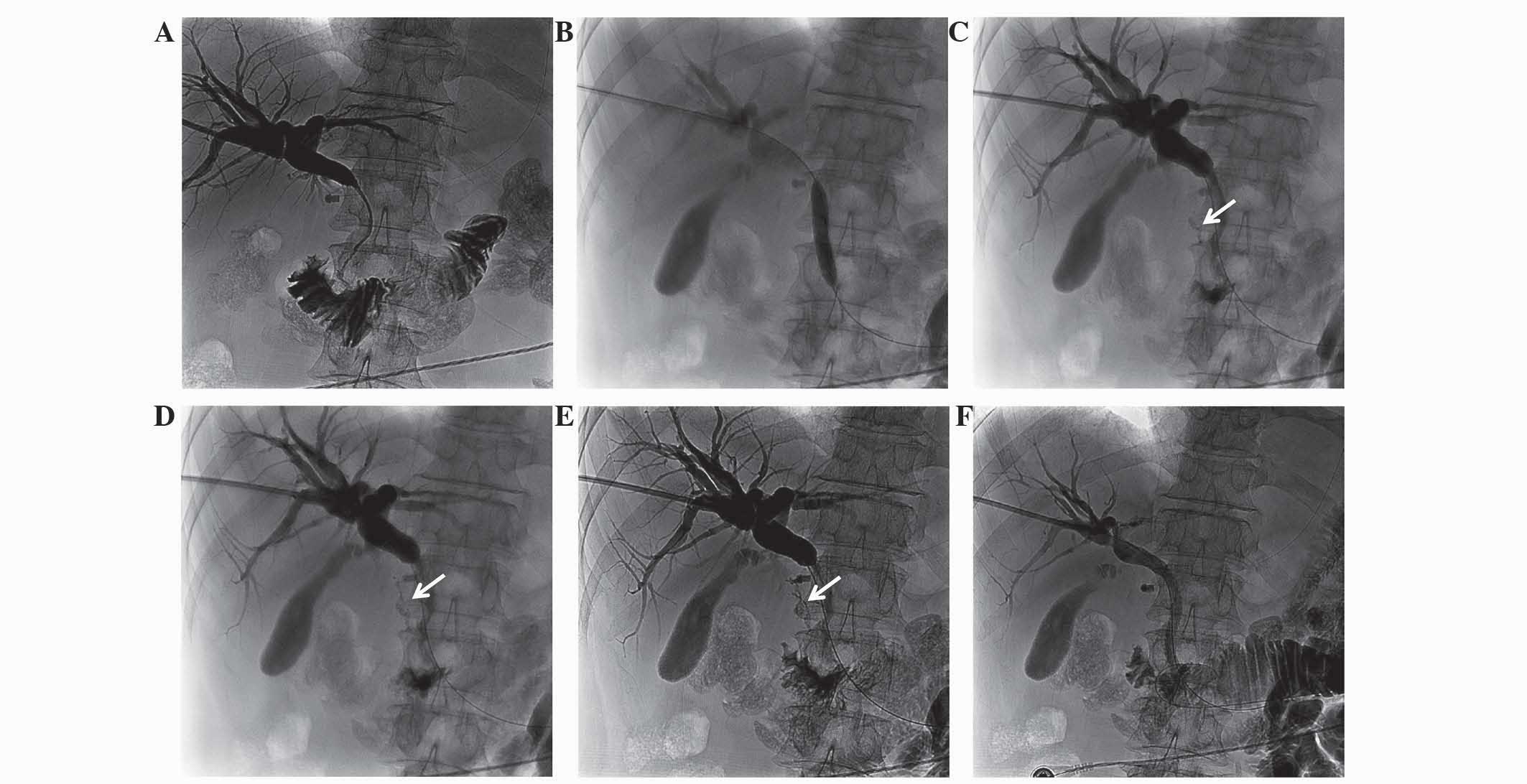
bilirubin from 257 to 65 mmol/l. PTC showed that the biliary duct
stricture section was located at the common bile duct (Fig. 3A).
After obtaining informed consent from the patient,
percutaneous intraductal RFA was combined with self-expandable
metal stent deployment on November 28, 2013. A guidewire was used
to place the 8 Fr percutaneous endobiliary RFA catheter in two
sections of the common bile duct to ablate the malignant tumor. RFA
was applied for 2 min at 10 W in each section following a 1-min
rest period. Due to the severity of the biliary duct stenosis, an
8×40-mm dilatation balloon catheter was used to pre-expand the bile
duct for stent deployment (Fig. 3B).
Following the dilation, PTC showed a considerably small-diameter
biliary tract perforation and overflow of the contrast agent
(Fig. 3C–E), although no signs of
choleperitonitis were observed. The 8×80-mm Zilver self-expanding
metal stent was then deployed to cover the perforated region. PTC
following stent deployment showed no contrast agent overflow to the
outside of the bile duct (Fig. 3F),
and the patient was discharged 7 days later. No follow-up of the
patient was performed.
Discussion
For patients with malignant biliary strictures and a
life expectancy of >3 months, self-expandable metal stent
deployment is the standard treatment option. The addition of RFA
could prove beneficial to such patients, as a recent retrospective
study comparing metal stenting with and without RFA showed
(8). The study demonstrated that RFA
was an independent predictor of survival in the treatment of
malignant biliary strictures. RFA with an image-guided minimally
invasive interventional approach has been used for several years to
treat patients with a variety of other primary and secondary
malignancies, including hepatocellular carcinoma, lung and breast
cancer, musculoskeletal system tumors, and renal and metastatic
carcinomas (9). The use of an
ablation catheter in malignant biliary obstruction was approved by
The United States Food and Drug Administration and the EU/EC
Declaration of Conformity (10);
however, intraductal RFA has not been considered, due to the
expected complication of thermal biliary damage from heating and
direct mechanical damage from the needle, such as bile leakage or
biliary stricture (11). By contrast,
biliary damage is a relatively uncommon complication following RFA
of hepatic tumors, with an incidence of 0.1–12.0% (12).
There have been reports of the use of intraductal
RFA for the treatment of unresectable malignant biliary
obstructions with percutaneous and endoscopic approaches,
demonstrating its feasibility and safety; pain, cholangitis and
asymptomatic biochemical pancreatitis have been reported as the
only common complications (2,6,13), while
hepatic coma, newly diagnosed left bundle branch block and partial
liver infarction have been reported as uncommon complications
(2,14,15).
However, a few cases of hemobilia and mortality following
intrabiliary RFA have also been reported (15). Despite the fact that, to the best of
our knowledge, there had previously been no cases of biliary tract
perforations following RFA, the said complication occurred in the
two cases mentioned in the present study, which was confirmed by
PTC. These cases involved unresectable malignant biliary
obstructions; a cholangiocarcinoma and a pancreatic carcinoma.
In the present study, the two cases received
overlapping RFA for 2 min at 10 W. Thermal injury induced deep bile
duct necrosis and possibly caused the perforations. Furthermore,
the dilatation of the bile duct with a balloon catheter (prior to
RFA in case 1, and following RFA in case 2) may have aggravated the
strong necrotic effect induced by RFA thermal injury. For the
treatment of minor biliary tract perforation, the insertion of a
self-expanding metal stent directly after the RFA procedure appears
to be an effective method (case 2); however, the management of
major biliary tract perforation is more challenging and may result
in severe complications, including mortality (case 1). Possible
preemptive strategies for the prevention of biliary tract
perforation could include pre-interventional investigation with
CT/magnetic resonance imaging, in order to identify the extent of
the tumor around the bile duct and avoid injuring the normal bile
duct. It is also important to avoid overlapping RFA. Finally, the
use of balloon angioplasty prior to or following RFA should be
carefully assessed.
The patient in case 1 also presented with melena the
day after RFA, indicating the possibility of a direct association
between the procedure and gastrointestinal bleeding. Only three
studies have reported a similar occurrence following intrabiliary
RFA, including six cases of hemobilia and one case of hepatic
artery pseudoaneurysm rupture (14,16,17). In
the present case, endoscopy was performed to identify the bleeding
site, but no injury or active bleeding was observed in the
duodenum. Thermal injury to the hepatic artery was therefore
presumed as the cause.
In conclusion, despite the therapeutic advantages of
endobiliary RFA against jaundice and the possibility of an
RFA-induced increase in the survival time of patients with
unresectable malignant biliary obstructions, biliary tract
perforation should be acknowledged as a serious potential
complication of the procedure, and the deployment of self-expanding
metal stents should be considered a preferable treatment option for
minor biliary perforation.
References
|
1
|
Pinter M, Hucke F, Zielonke N, et al:
Incidence and mortality trends for biliary tract cancers in
Austria. Liver Int. 34:1102–1108. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Steel AW, Postgate AJ, Khorsandi S, et al:
Endoscopically applied radiofrequency ablation appears to be safe
in the treatment of malignant biliary obstruction. Gastrointest
Endosc. 73:149–153. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Rustagi T and Jamidar PA: Intraductal
radiofrequency ablation for management of malignant biliary
obstruction. Dig Dis Sci. 59:2635–2641. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Kullman E, Frozanpor F, Söderlund C, et
al: Covered versus uncovered self-expandable nitinol stents in the
palliative treatment of malignant distal biliary obstruction:
Results from a randomized, multicenter study. Gastrointest Endosc.
72:915–923. 2010. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Law R, Pai M, Baron TH and Habib N: The
effects of endobiliary radiofrequency ablation in two patients with
pancreatic cancer: Gross and microscopic findings. Gastrointest
Interv. 2:124–126. 2013. View Article : Google Scholar
|
|
6
|
Mizandari M, Pai M, Xi F, et al:
Percutaneous intraductal radiofrequency ablation is a safe
treatment for malignant biliary obstruction: Feasibility and early
results. Cardiovasc Intervent Radiol. 36:814–819. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Karnofsky DA, Abelmann WH, Craver LF and
Burchenal JH: The use of nitrogen mustard in the palliative
treatment of cancer with particular reference to bronchogenic
carcinoma. Cancer. 1:634–656. 1948. View Article : Google Scholar
|
|
8
|
Sharaiha RZ, Natov N, Glockenberg KS, et
al: Comparison of metal stenting with radiofrequency ablation
versus stenting alone for treating malignant biliary strictures: Is
there an added benefit? Dig Dis Sci. 59:3099–3102. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Gazelle GS, Goldberg SN, Solbiati L and
Livraghi T: Tumor ablation with radio-frequency energy. Radiology.
217:633–646. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Lui KL and Li KK: Intraductal
radiofrequency ablation of tumour ingrowth into an uncovered metal
stent used for inoperable cholangiocarcinoma. Hong Kong Med J.
19:539–541. 2013. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Livraghi T, Solbiati L, Meloni MF, et al:
Treatment of focal liver tumors with percutaneous radio-frequency
ablation: Complications encountered in a multicenter study.
Radiology. 226:441–451. 2003. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Fonseca AZ, Santin S, Gomes LG, Waisberg J
and Ribeiro MA Jr: Complications of radiofrequency ablation of
hepatic tumors: Frequency and risk factors. World J Hepatol.
6:107–113. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Figueroa-Barojas P, Bakhru MR, Habib NA,
et al: Safety and efficacy of radiofrequency ablation in the
management of unresectable bile duct and pancreatic cancer: A novel
palliation technique. J Oncol. 2013:9108972013. View Article : Google Scholar : PubMed/NCBI
|
|
14
|
Dolak W, Schreiber F, Schwaighofer H, et
al: Endoscopic radiofrequency ablation for malignant biliary
obstruction: A nationwide retrospective study of 84 consecutive
applications. Surg Endosc. 28:854–860. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Alis H, Sengoz C, Gonenc M, Kalayci MU and
Kocatas A: Endobiliary radiofrequency ablation for malignant
biliary obstruction. Hepatobiliary Pancreat Dis Int. 12:423–427.
2013. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Tal AO, Vermehren J, Friedrich-Rust M, et
al: Intraductal endoscopic radiofrequency ablation for the
treatment of hilar non-resectable malignant bile duct obstruction.
World J Gastrointest Endosc. 6:13–19. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Topazian M, Levy MJ, Patel S, Charlton MR
and Baron TH: Hepatic artery pseudoaneursym formation following
intraductal biliary radiofrequency ablation. Endoscopy. 45(Suppl
2): S161–S162. 2013.
|