Introduction
Primary peritoneal serous carcinoma (PPSC) is an
extremely rare malignancy that was first described in 1959
(1). The estimated incidence of PPSC
in the United States is 6.78 cases per 1,000,000 individuals
(2). This type of cancer arises from
the peritoneal epithelium and is similar to serous ovarian
carcinoma. A diagnosis of PPSC is typically made based on the
Gynecology Oncology Group criteria (3). However, a correct differential diagnosis
of PPSC is difficult preoperatively. The median overall survival
time of PPSC is 11–17 months (4) and
the optimal treatments for PPSC are surgical resection and platinum
based chemotherapy (5).
The current study presents the case of a 66 year-old
female patient diagnosed with PPSC mimicking omental metastasis and
peritoneal carcinomatosis from the gastrointestinal tract or
ovarian malignancy. PPSC is extremely rare with few cases cited in
the current literature. The present study describes a rare case of
PPSC with a review of the literature. Written informed consent was
obtained from the patient.
Case report
In September 2014, a 66-year-old woman presented to
Yeungnam University College of Medicine (Daegu, Korea) with abdomen
distension for 3 weeks. Otherwise, the patient was in good health
with intermittent abdominal discomfort. Findings upon physical
examination were unremarkable. Furthermore, the initial laboratory
tests were all within normal ranges. Chest and abdominal
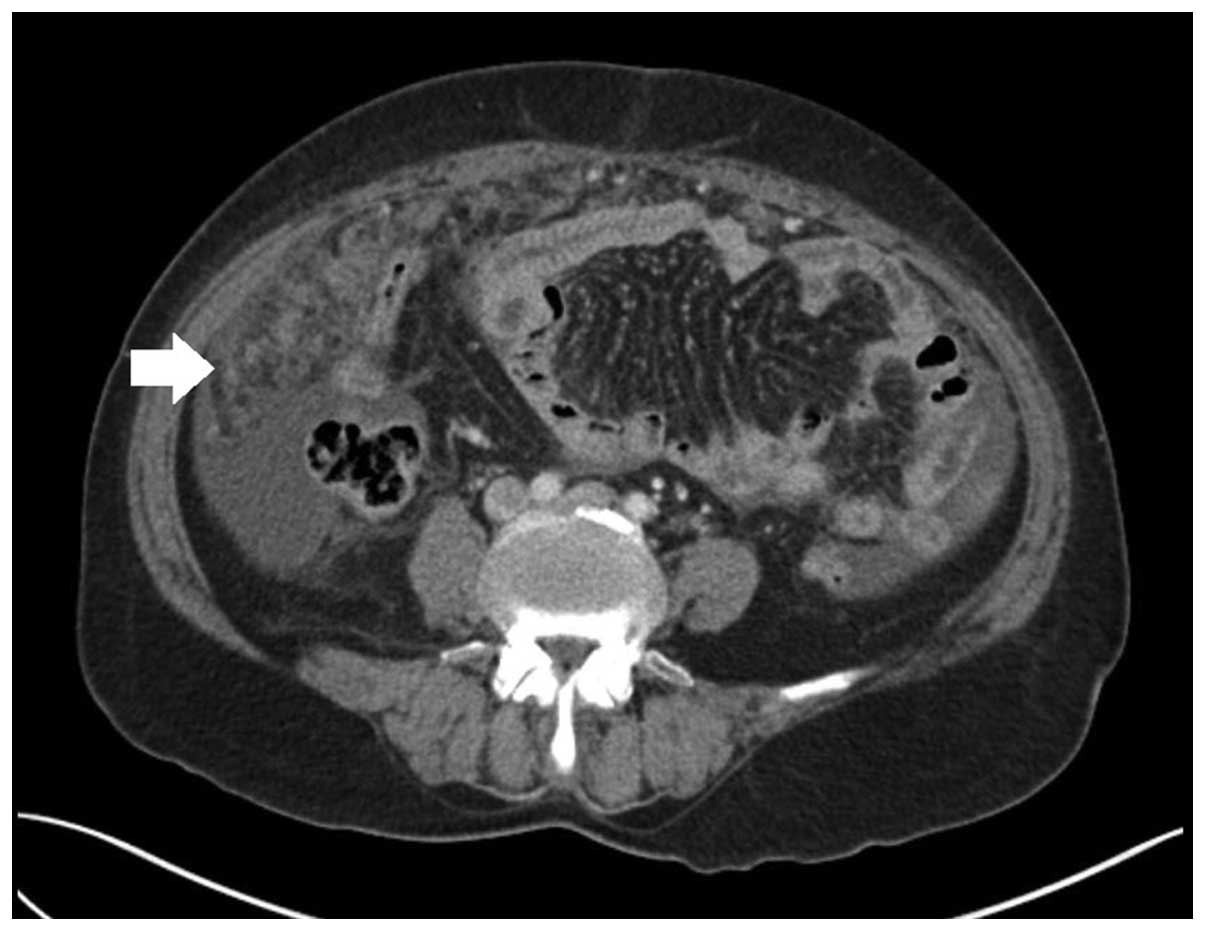
radiographs were also unremarkable. The patient underwent a
contrast-enhanced abdominal computed tomography (CT) scan (SOMATOM
Definition AS; Siemens AG, Munich, Germany) to evaluate the cause
of the abdominal distension. The CT scan revealed abundant ascites
in the abdominal cavity and omental infiltration (Fig. 1). Other abdominal organs, including
the liver, spleen, kidney and both ovaries, appeared normal upon
CT. Ascitic cytology was then performed; evaluation of the
cytological characteristics of the ascites suggested the presence
of malignant cells.
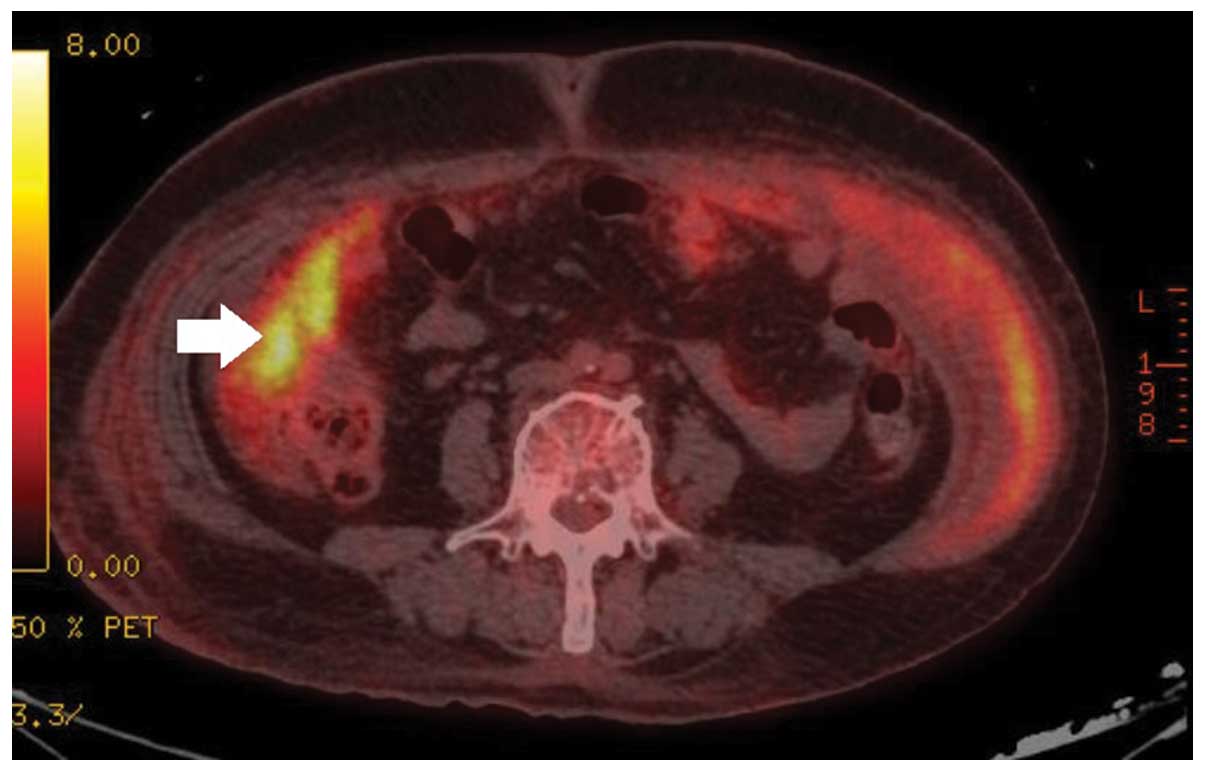
18F-fluorodeoxyglucose positron emission tomography
(PET)/CT (Discovery DVCT; GE Healthcare Bio-Sciences, Pittsburgh,
PA, USA) was then performed to evaluate the primary origin of the
malignancy. The result of PET/CT revealed hot uptake in the greater
omentum (Fig. 2). Other abdominal
organs, including the stomach, colon, pancreas, uterus and both
ovaries, were within the normal range of uptake. Furthermore, the
patient's preoperative serum cancer antigen-125 (CA-125) levels
were elevated to 1,032 U/ml (normal range, 0–35 U/ml).
Based on the aforementioned results, a diagnosis of
primary peritoneal malignancy was determined. Surgery was
identified as the most appropriate treatment strategy, therefore,
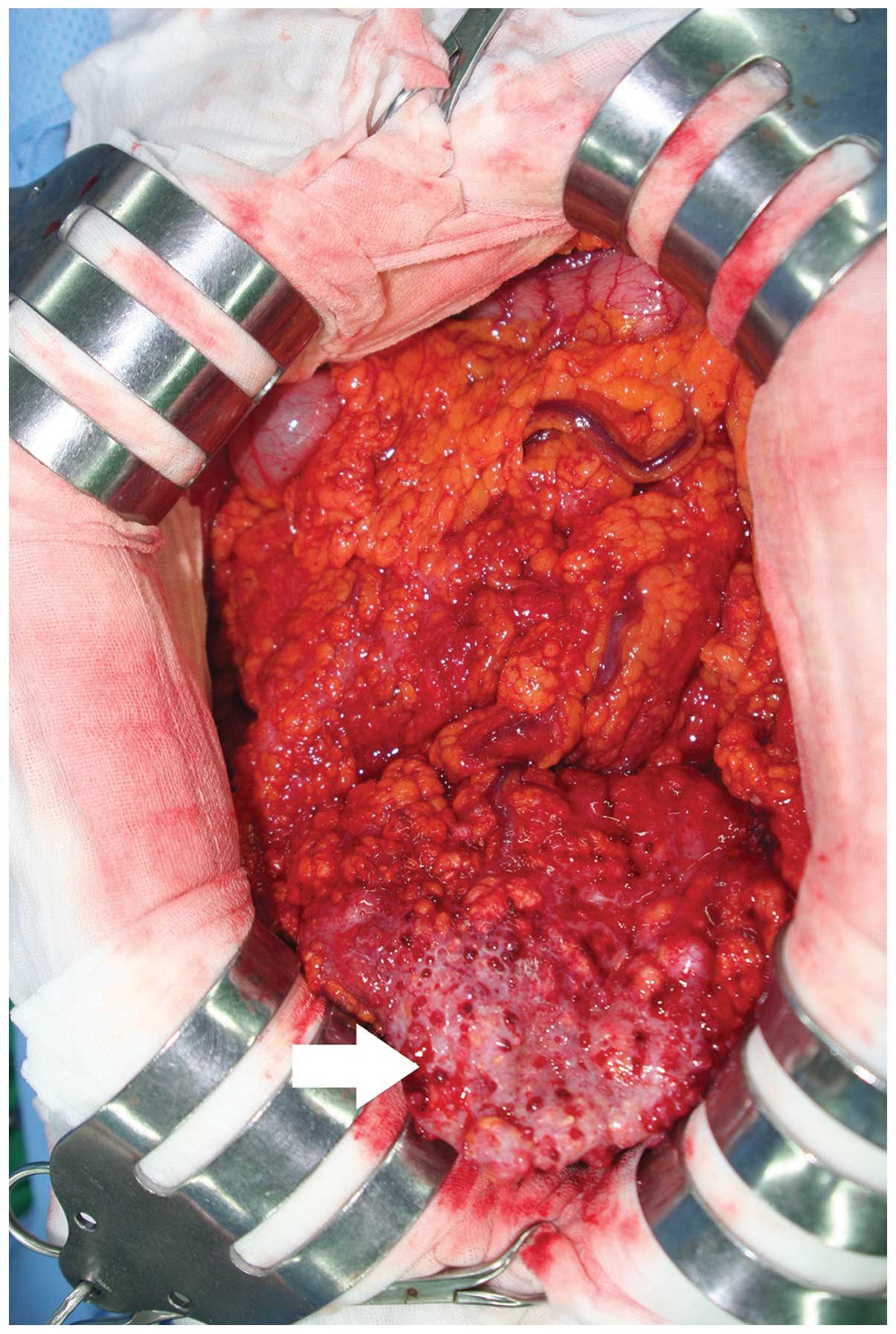
surgical exploration was performed in December 2014. Upon surgical
exploration, ~1,000 cm3 ascites, a whitish mass
(measuring 16×10×2.4 cm) and a nodule were found in the greater
omentum (Fig. 3). The uterus and both
adnexa were unremarkable without tumor involvement. The stomach,
liver, small bowel, large bowel and pancreas were also
unremarkable. Inspection of the abdominal cavity revealed a
rice-sized nodule in the mesentery, peritoneum and pelvic cavity.
Thus, omentectomy was performed. Resected tissue was fixed in 10%
buffered-formalin, paraffin-embedded and cut into 4 µm sections,
and subsequently stained with hematoxylin and eosin. For
immunohistochemical analysis, the specimens were incubated with
monoclonal mouse anti-human cytokeratin 7 (cat. no. M7018; 1:200;
Dako, Glostrup, Denmark), monoclonal mouse anti-human WT-1 (cat.
no. 348M-94; 1:100; Cell Marque™; Sigma-Aldrich, St. Louis, MO,
USA) and monoclonal mouse anti-human CA-125 (cat. no. M3519; 1:40;
Dako) antibodies. The results revealed positivity for
cytokeratin-7, WT-1 and CA-125. Pathological examination of the
resected specimen further indicated a diagnosis of PPSC. In the
current case, both ovaries were of normal size with no observed
abnormalities, and the main tumor was identified in the omentum.
Therefore, according to the Gynecology Oncology Group criteria
(3), surgical and pathological
findings, a diagnosis of PPSC was determined. The patient was
treated with regular chemotherapy [7 cycles of 175 mg/m2
paclitaxel and carboplatin (AUC, 4–7.5) every 3 weeks], which was
initiated in December 2014, and was followed up every month. The
patient had an uneventful postoperative course, and is currently
alive and well.
Discussion
Peritoneal malignancies may be classified as primary
or secondary, depending on the site of origin of the cancer.
Primary peritoneal malignancies, which include malignant
mesothelioma, serous carcinoma and sarcomas, are rare (6). Among these primary peritoneal
malignancies, PPSC, is an extremely rare subtype that was first
described in 1959 (1). In the United
States, the incidence of PPSC is 6.78 cases per 1,000,000
individuals (2). However, the
worldwide incidence rate is unknown and publications concerning
PPSC are only case reports or case series.
The common presenting symptoms of PPSC are abdominal
distension, abdominal pain and discomfort. Therefore, symptoms of
PPSC are similar to those of peritoneal carcinomatosis.
Furthermore, the majority patients described in case reports to
date were diagnosed in the advanced stages of the disease (7,8).
Traditionally, a diagnosis of PPSC is based on the Gynecology
Oncology Group criteria, as follows: i) The ovaries are either
absent or normal in size; ii) the involvement of the extraovarian
sites is greater than the involvement of the surface of either
ovary; iii) the absence of a deep-seated invasive ovarian carcinoma
or invasive disease in the ovarian cortical stroma with tumors that
measuring <5×5 mm2; and iv) histopathological and
cytological characteristics of the tumors similar to those for
epithelial ovarian cancer (3).
Preoperatively, a correct diagnosis of PPSC is difficult. The
current case was preoperatively diagnosed with omental metastasis
and peritoneal carcinomatosis from the gastrointestinal tract or
ovarian malignancy. However, PET/CT is beneficial due to its
ability to define the extent of metabolically active disease and
its ability to detect distant metastasis. Therefore, PET/CT is
beneficial for the differentiation of PPSC from ovarian cancer
(9).
In postoperative immunohistochemical examinations,
PPSC is typically positive for cytokeratin-7, CA-125, estrogen
receptor and Wilms' tumor-1 (WT-1) (5). In the current case, cytokeratin-7, WT-1
and CA-125 were positive.
The optimal treatment of PPSC is surgical resection
and chemotherapy, with platinum-based chemotherapy used most
commonly (10). Intraperitoneal
chemotherapy has recently demonstrated a survival benefit in
patients with PPSC when compared to those treated with surgery
alone or surgery in combination with systemic chemotherapy
(11).
Although it is difficult to generalize, as some
published survival data were from small size studies, the median
survival time of patients with PPSC is 11–17 months (4), which is similar to the present case with
a current survival time of 15 months.
In conclusion, the current study presented a case of
PPSC treated with debulking surgery. Although PPSC is considered
extremely rare, its recognition is important for accurate
evaluation and management. Due to its significant rarity,
multicenter studies are required to further understand prognosis
and identify an effective treatment approach.
Acknowledgements
The present study was supported by the 2015 Yeungnam
University Research Grant.
References
|
1
|
Swerdlow M: Mesothelioma of the pelvic
peritoneum resembling papillary cystadenocarcinoma of the ovary;
case report. Am J Obstet Gynecol. 77:197–200. 1959. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Goodman MT and Shvetsov YB: Incidence of
ovarian, peritoneal and fallopian tube carcinomas in the United
States, 1995–2004. Cancer Epidemiol Biomarkers Prev. 18:132–139.
2009. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Bloss JD, Liao SY, Buller RE, Manetta A,
Berman ML, McMeekin S, Bloss LP and DiSaia PJ: Extraovarian
peritoneal serous papillary carcinoma: A case-control retrospective
comparison to papillary adenocarcinoma of the ovary. Gynecol Oncol.
50:347–351. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Roh SY, Hong SH, Ko YH, Kim TH, Lee MA,
Shim BY, Byun JH, Woo IS, Kang JH, Hong YS and Lee KS: Clinical
characteristics of primary peritoneal carcinoma. Cancer Res Treat.
39:65–68. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Turnage RH and Badgwell B: Abdominal wall,
umbilicus, peritoenum, mesentery, omentum and retroperitoneum.
Townsend CM Jr, Beauchamp RD, Evers BM and Mattox KL: Sabiston
Textbook of Surgery (19th). Saunders Elsevier. (Philadelphia, PA).
11022012.
|
|
6
|
Bhanvadia VM, Parmar JK, Madan YG and
Sheikh SS: Primary peritoneal serous carcinoma: A rare case and
palliative approach. Indian J Palliat Care. 20:157–159. 2014.
View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Hou T, Liang D, He J, Chen X and Zhang Y:
Primary peritoneal serous carcinoma: A clinicopathological and
immunohistochemical study of six cases. Int J Clin Exp Pathol.
5:762–769. 2012.PubMed/NCBI
|
|
8
|
Rakheja R, Makis W and Hickeson M:
Extraovarian primary peritoneal carcinoma: Staging with 18F-FDG
PET/CT. Abdom Imaging. 37:304–308. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
von Riedenauer WB, Janjua SA, Kwon DS,
Zhang Z and Velanovich V: Immunohistochemical identification of
primary peritoneal serous cystadenocarcinoma mimicking advanced
colorectal carcinoma: A case report. J Med Case Rep. 1:1502007.
View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Unal OU, Oztop I, Yazici O, Ozatli T, Inal
A, Günaydın Y, Alici S, Demirci U, Cinkir HY, Aktas B, et al:
Treatment and prognostic factors in primary peritoneal carcinoma: A
multicenter study of the Anatolian society of medical oncology
(ASMO). Oncol Res Treat. 37:332–338. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Bakrin N, Gilly FN, Baratti D, Bereder JM,
Quenet F, Lorimier G, Mohamed F, Elias D and Glehen O: Association
Française de Chirurgie: Primary peritoneal serous carcinoma treated
by cytoreductive surgery combined with hyperthermic intraperitoneal
chemotherapy. A multi-institutional study of 36 patients. Eur J
Surg Oncol. 39:742–747. 2013. View Article : Google Scholar : PubMed/NCBI
|