Introduction
Malignant phyllodes tumor of the breast (MPTB) is a
rare but distinct clinicopathological entity. MPTB typically occurs
in middle-aged women (1), and has an
average annual age-adjusted incidence of 2.1 per million females
(2). As far as the etiology is
concerned, Li-Fraumeni syndrome (germline TP53 mutation) has been
reported to increase the risk of phyllodes tumors (3,4). Surgery
is the typical initial treatment option for MPTB and radiotherapy
is recommended for individuals with a high local recurrence risk.
Chemotherapy is used to treat patients with a high systemic
metastatic risk (3). Given its
rarity, decisions regarding treatment options are based on
small-scale retrospective clinical trials or case reports (5,6,7). A rapidly-growing breast mass is the most
typical symptoms of MPBT and postoperative pathology is the most
accurate method of diagnosis (3).
Surgery is regarded as the primary method of management of MPBT.
The clear margin achieved by surgery rather than the surgery type
(breast conserving surgery or total mastectomy) determines the
local recurrence rate (6). The
five-year disease-free survival (DFS) is 60–90% (6). A previous study observed that 14.3% of
patients died of metastatic MPTB 5 years following initial
diagnosis (6). To date, the optimal
intervention strategy has not been established. Herein, the case of
a giant MPTB (the postoperative specimen measured 14.5×10.5×4.5
cm), in which surgery, adjuvant chemotherapy and radiotherapy was
performed, is presented. Written informed consent was obtained from
the patient for the publication of her data in the present case
report. In addition, the related literature was reviewed in order
to expand our understanding of this unique breast malignancy.
Case report
A 43-year-old female was referred to The First
Hospital of Jilin University in August, 2014 with a history of a
painless lump in the right breast for 9 months. She had no other
discomfort. Her past history was unremarkable, except allergies to
starch and penicillin.
On physical examination, a large firm mass measuring
about 11×4.5 cm was palpated in the upper outer quadrant of right
breast. A skin ulcer of 1.4 cm was present on the surface of the
mass. In the bilateral supra- and subclavicular regions and
axillas, there were no palpable enlarged lymph nodes.
Laboratory investigations revealed that the complete
blood cell count and serum biochemical profile were normal.
Ultrasound (Philips iU22; Philips Medical Systems, Inc., Bothell,
WA, USA) of the breast demonstrated an 11.2×4.54-cm, heterogeneous,
hypoechoic mass in the upper outer quadrant of right breast with
blood flow. Mammography (Selenia Dimensions mammography system;
Hologic Corporation, Bedford, MA, USA) also revealed an 11.0×4.5 cm
irregular mass of high density. The BI-RADS stage (8) was determined to be 4B due to the
observations of an unclear border and irregular lesion shape
revealed by the ultrasound. The subsequent biopsy indicated
mesenchymal malignancy, as hematoxylin and eosin staining revealed
spindle neoplastic cells and immunohistochemistry demonstrated
Ki-67 (30%+) and AE1/AE3 (−). An abdominal ultrasound and bone scan
yielded unremarkable results.
The patient's performance status was evaluated as 1
based on Eastern Cooperative Oncology Group criteria (9). The patient subsequently underwent a
simple mastectomy plus sentinel lymph node biopsy. Biopsy and
postoperative specimens were fixed in formalin, embedded in
paraffin, sliced and stained by hematoxylin and eosin (10). Immunohistochemistry was performed
using the dex-tran-polymer method (EnVision+; Dako, Glostrup,
Denmark) (10) using the following
monoclonal mouse anti-human antibodies against Ki-67 (dilution,
1:200; catalog no., RMA-0542), AE1/AE3 (dilution, 1:200; catalog
no., MAB-0049), cluster of differentiation (CD)34 (dilution, 1:200;
catalog no., MAB-0034), desmin (dilution, 1:200; catalog no.,
MAB-0055), leukocyte common antigen (LCA; dilution, 1:200; catalog
no. MAB-0037), smooth muscle actin (SMA; dilution, 1:200; catalog
no., MAB-003), estrogen receptor (ER; dilution, 1:200; catalog no.,
MAB-0062), S-100 (dilution, 1:200; catalog no., RAB-0150), CD68
(dilution, 1:200; catalog no., MAB-0041) and cytokeratin (dilution,
1:200; catalog no., MAB-0049). All the antibodies were purchased
from Fuzhou Maixin Biotechnology Development Co., Ltd., Fuzhou,
China. Goat anti-mouse IgG horseradish peroxidse-conjugated
secondary antibodies (MaxVision™ kit; catalog no.,
KIT-5010/5020/5030; Fuzhou Maixin Biotechnology Development Co.,
Ltd.) were incubated with the samples according to the
manufacturer's protocol. The 3,3′-diaminobenzidine chromogenic
reagent kit was also purchased from Fuzhou Maixin Biotechnology
Development Co., Ltd., and used according to the manufacturer's
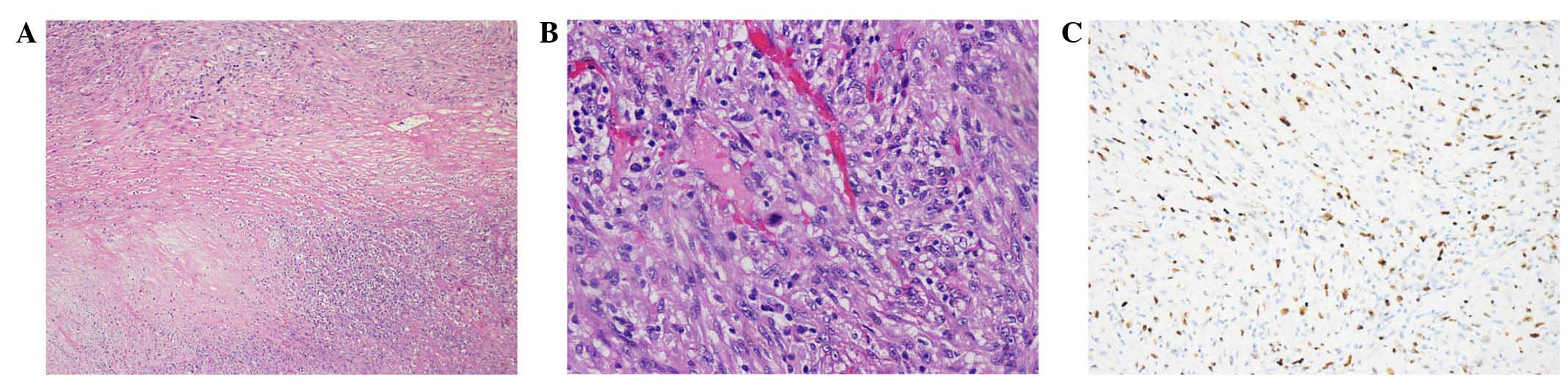
protocol. The postoperative pathology revealed a high-grade
malignant phyllodes tumor with multifocal necrosis (Fig. 1A). The primary tumor measured
14.5×10.5×4.5 cm, with involvement of the skin, tissue beneath the
nipple and superficial fascia, and a high mitotic rate (2–5 per
high power field; Fig. 1B). There was
no evidence of lymphovascular or neural invasion. The final
immunohistochemistry results demonstrated a Ki-67 index of 30%+
(Fig. 1C); negative reactivity for
cytokeratin, AE1/AE3, CD34, desmin, LCA, SMA and ER(−); and diffuse
positive reactivity for S-100 and CD68. Two sentinel lymph nodes
proved negative for metastasis.
Postoperatively, 4 cycles of chemotherapy were
administered. The first 2 cycles were as follows: Pirarubicin, 80
mg (50 mg/m2), day 1; cyclophosphamide, 800 mg (500
mg/m2), day 1; and liposomal paclitaxel, 270 mg (175
mg/m2), day 2. The 3rd and 4th cycles consisted of the
following: Pirarubicin, 70 mg, day 1; cyclophosphamide, 700 mg, day
1; liposomal paclitaxel, 270 mg, day 2. Prophylactic chest
irradiation was subsequently performed, with a dose of 60 Gy/30
fractions. To date, the patient has a good quality of life and has
demonstrated DFS for 18 months.
Discussion
Phyllodes tumors (PTs) are rather rare entities,
accounting for only 1% of all breast tumors (1). In 2003, the World Health Organization
classified PTs into three subtypes, designated benign, borderline
and malignant, according to various clinicopathological
characteristics, including the degree of stromal cell atypia and
stromal overgrowth, tumor necrosis, the status of mitosis and the
tumor margin. (11–13). An extensive literature review was
performed in the Pubmed database (www.ncbi.nlm.nih.gov/pubmed) using the following key
terms: ‘Malignant phyllodes tumor and breast’. The search was
performed on the titles of English language articles published
between 1993 and 2015. The relevant literature was studied to gain
a full-scale understanding of MPTB. In the United States, ~500 new
MPTB cases are diagnosed annually (14). A fast-growing breast mass is the most
common manifestation. Giant MPTB can lead to the development of
hypoglycemia, which results from increased insulin-like growth
factor 2 levels produced by the tumor (15,16).
Metastasis from MPTB occurs in 6.2–25% of cases (17), most frequently metastasizing to the
lung, bone and liver (18,19).
Imaging procedures, such as ultrasound and
mammography, are barely able to differentiate PT from fibroadenoma
(3,20). In a previous study, mammography
diagnosed PT in only 32% of cases (20). In addition, fine needle aspiration
cytology or even core biopsy are usually inadequate for accurate
diagnosis of PT (20). According to
the report by Salvadori et al (20), cytology was performed on 30 patients
in their study, and was suggestive of PT in only 4 cases.
Surgery is the primary option for the treatment of
MPTB. For a long time, the extension of resection, namely the
choice between breast-conserving surgery (BCS) and mastectomy, has
remained controversial. Wide resection with clear margins of ≥1 cm
has been recommended (21,22). However, research by Belkacémi et
al (23) revealed that, for
borderline and malignant PTs of the breast, total mastectomy was
superior to BCS in order to guarantee adequate safe margins. Mituś
et al (6) supported that a
tumor-free margin of ≥1 cm is critical for favorable local control
following mastectomy or BCS. MPTB has a propensity for rare
metastasis to the axillary lymph nodes, described in <10% of
cases; therefore, axillary dissection is not routinely performed
(24,25).
Positive surgical margins and large primary tumor
have been proved to be poor prognostic factors for local recurrence
(1). For patients with MPTB measuring
>2 cm after lumpectomy, or tumors >10 cm after mastectomy,
adjuvant radiotherapy is strongly recommended to control the high
local relapse rate of ≥15% (26).
Barth Jr et al (14) held the
view that, for all the borderline and malignant breast PTs after
margin-negative BCS, radiotherapy should be initiated. In their
multi-institutional study, despite a median negative margin of 0.35
cm after BCS, the local relapse rate was unexpectedly high at 21%.
Postoperative radiotherapy was effective in reducing the local
recurrence, which is considered to be a strong indicator of distant
metastases (23,26,27) and is
associated with significantly increased risk of mortality (26). Furthermore, given the fact that the
most common local relapses occurred in the site of initial
resection by BCS, partial breast irradiation may be as effective as
whole breast irradiation (14). In
the current case, the giant primary tumor (14.5×10.5×4.5 cm) and
close margin (involvement of superficial fascia) indicated a high
risk of local recurrence, making timely radiotherapy important for
local control. Radiotherapy is also an effective treatment for
symptomatic metastases of MPTB (28).
To date, the role of adjuvant chemotherapy remains
controversial; cisplatin and etoposide, and ifosfamide alone or in
combination with doxorubicin have been proven to be effective
(29,30). For large tumors (>5 cm) or
recurrent MPTB, chemotherapy is beneficial (29). The epithelial element of PT partially
expresses ER (58%) or progesterone receptor (75%); however, there
is no evidence that endocrine therapy is beneficial for treating
PTs (31).
In conclusion, MPTB is a rare entity with distinct
clinicopathological features. There is no established consensus
regarding the optimal type of surgery and indications for
radiotherapy and chemotherapy regimens. In the current case of a
giant MPTB, multidisciplinary interventions contributed to
favorable outcomes. In the future, large-scale multi-institutional
clinical trials should be launched to clarify the indication for
radiotherapy for MPTB.
Acknowledgements
The present study was supported by Traditional
Chinese Medicine Administration Bureau of Jilin Province (grant no.
2014-Q54).
Glossary
Abbreviations
Abbreviations:
|
BCS
|
breast conserving surgery
|
|
MPTB
|
malignant phyllodes tumor of the
breast
|
|
PT
|
phyllodes tumor
|
References
|
1
|
Jang JH, Choi MY, Lee SK, Kim S, Kim J,
Lee J, Jung SP, Choe JH, Kim JH, Kim JS, et al: Clinicopathologic
risk factors for the local recurrence of phyllodes tumors of the
breast. Ann Surg Oncol. 19:2612–2617. 2012. View Article : Google Scholar : PubMed/NCBI
|
|
2
|
Bernstein L, Deapen D and Ross RK: The
descriptive epidemiology of malignant cystosarcoma phyllodes tumors
of the breast. Cancer. 71:3020–3024. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Gradishar WJ, Anderson BO, Balassanian R,
Blair SL, Burstein HJ, Cyr A, Elias AD, Farrar WB, Forero A,
Giordano SH, et al: Breast Cancer, Version 1.2016. J Natl Compr
Canc Netw. 13:1475–1485. 2015.PubMed/NCBI
|
|
4
|
Birch JM, Alston RD, McNally RJ, Evans DG,
Kelsey AM, Harris M, Eden OB and Varley JM: Relative frequency and
morphology of cancers in carriers of germline TP53 mutations.
Oncogene. 20:4621–4628. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Karczmarek-Borowska B, Bukala A,
Syrek-Kaplita K, Ksiazek M, Filipowska J and Gradalska-Lampart M: A
rare case of breast malignant phyllodes tumor with metastases to
the kidney: Case report. Medicine (Baltimore). 94:e13122015.
View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Mituś J, Reinfuss M, Mituś JW, Jakubowicz
J, Blecharz P, Wysocki WM and Skotnicki P: Malignant phyllodes
tumor of the breast: Treatment and prognosis. Breast J. 20:639–644.
2014. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Reinfuss M, Mituś J, Smolak K and Stelmach
A: Malignant phyllodes tumours of the breast. A clinical and
pathological analysis of 55 cases. Eur J Cancer. 29A:1252–1256.
1993. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Sedgwick EL, Ebuoma L, Hamame A, Phalak K,
Ruiz-Flores L, Ortiz-Perez T and Sepulveda KA: BI-RADS update for
breast cancer caregivers. Breast Cancer Res Treat. 150:243–254.
2015. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Oken MM, Creech RH, Tormey DC, Horton J,
Davis TE, McFadden ET and Carbone PP: Toxicity and response
criteria of the Eastern Cooperative Oncology Group. Am J Clin
Oncol. 5:649–655. 1982. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Ma XB, Zheng Y, Yuan HP, Jiang J and Wang
YP: CD43 expression in diffuse large B-cell lymphoma, not otherwise
specified: CD43 is a marker of adverse prognosis. Hum Pathol.
46:593–599. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Lakhani SR, Ellis IO, Schnitt SJ, Tan PH
and van de Vijver MJ: WHO classification of tumours of the breast.
IARC WHO Classification of Tumours. 4:(4th). IARC Press. (Lyon).
2012.
|
|
12
|
Wu DI, Zhang H, Guo L, Yan XU and Fan Z:
Invasive ductal carcinoma within borderline phyllodes tumor with
lymph node metastases: A case report and review of the literature.
Oncol Lett. 11:2502–2506. 2016.PubMed/NCBI
|
|
13
|
Bellocq JP and Magro G: Fibroepithelial
tumours (Chapter 1 - Tumours of the Breast). Pathology and Genetics
- Tumours of the Breast and Female Genital Organs (World Health
Organization Classification of Tumours). Tavassoli FA and Devilee
P: (5th). IARC Press. (Lyon, France). 99–103. 2003.
|
|
14
|
Barth RJ Jr, Wells WA, Mitchell SE and
Cole BF: A prospective, multi-institutional study of adjuvant
radiotherapy after resection of malignant phyllodes tumors. Ann
Surg Oncol. 16:2288–2294. 2009. View Article : Google Scholar : PubMed/NCBI
|
|
15
|
Aguiar Bujanda D, Rivero Vera JC, Cabrera
Suárez MA, Aguiar Morales J, Christol R, Bohn Sarmiento U,
Domínguez Cabrera C and Le Bouc Y: Hypoglycemic coma secondary to
big insulin-like growth factor II secretion by a giant phyllodes
tumor of the breast. Breast J. 13:189–191. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
16
|
Kataoka T, Haruta R, Goto T, Sugino K,
Asahara T, Dohi K, Kaneco M, Arihiro K and Nomura S: Malignant
phyllodes tumor of the breast with hypoglycemia: Report of a case.
Jpn J Clin Oncol. 28:276–280. 1998. View Article : Google Scholar : PubMed/NCBI
|
|
17
|
Rowe JJ and Prayson RA: Metastatic
malignant phyllodes tumor involving the cerebellum. J Clin
Neurosci. 22:226–227. 2015. View Article : Google Scholar : PubMed/NCBI
|
|
18
|
Hlavin ML, Kaminski HJ, Cohen M,
Abdul-Karim FW and Ganz E: Central nervous system complications of
cystosarcoma phyllodes. Cancer. 72:126–130. 1993. View Article : Google Scholar : PubMed/NCBI
|
|
19
|
Al-Zoubaidi M, Qiu S, Bonnen M, Bonnen M,
Joyner M, Roehl K, Silva C and Chao C: Malignant phyllodes tumor of
the breast: A case report. Open Breast Cancer J. 3:45–48. 2011.
View Article : Google Scholar
|
|
20
|
Salvadori B, Cusumano F, Del Bo R,
Delledonne V, Grassi M, Rovini D, Saccozzi R, Andreola S and
Clemente C: Surgical treatment of phyllodes tumors of the breast.
Cancer. 63:2532–2536. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
21
|
Barth RJ: Histologic features predict
local recurrence after breast conserving therapy of phyllodes
tumors. Breast Cancer Res Treat. 57:291–295. 1999. View Article : Google Scholar : PubMed/NCBI
|
|
22
|
Khan SA and Badve S: Phyllodes tumors of
the breast. Curr Treat Options Oncol. 2:139–147. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
23
|
Belkacémi Y, Bousquet G, Marsiglia H,
Ray-Coquard I, Magné N, Malard Y, Lacroix M, Gutierrez C, Senkus E,
Christie D, et al: Phyllodes tumor of the breast. Int J Radiat
Oncol Biol Phys. 70:492–500. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
24
|
Khosravi-Shahi P: Management of non
metastatic phyllodes tumors of the breast: Review of the
literature. Surg Oncol. 20:e143–e148. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
25
|
Kraemer B, Hoffmann J, Roehm C, Gall C,
Wallwiener D and Krainick-Strobel U: Cystosarcoma phyllodes of the
breast: A rare diagnosis: Case studies and review of literature.
Arch Gynecol Obstet. 276:649–653. 2007. View Article : Google Scholar : PubMed/NCBI
|
|
26
|
Pezner RD, Schultheiss TE and Paz IB:
Malignant phyllodes tumor of the breast: Local control rates with
surgery alone. Int J Radiat Oncol Biol Phys. 71:710–713. 2008.
View Article : Google Scholar : PubMed/NCBI
|
|
27
|
Kapiris I, Nasir N, A'Hern R, Healy V and
Gui GP: Outcome and predictive factors of local recurrence and
distant metastases following primary surgical treatment of
high-grade malignant phyllodes tumors of the breast. Eur J Surg
Oncol. 27:723–730. 2001. View Article : Google Scholar : PubMed/NCBI
|
|
28
|
Burton GV, Hart LL, Leight GS Jr, Iglehart
JD, McCarty KS Jr and Cox EB: Cystosarcoma phyllodes: Effective
therapy with cisplatin and etoposide chemotherapy. Cancer.
63:2088–2092. 1989. View Article : Google Scholar : PubMed/NCBI
|
|
29
|
Pacioles T, Seth R, Orellana C, John I,
Panuganty V and Dhaliwal R: Malignant phyllodes tumor of the breast
presenting with hypoglycemia: A case report and literature review.
Cancer Manag Res. 6:467–473. 2014. View Article : Google Scholar : PubMed/NCBI
|
|
30
|
Hawkins RE, Schofield JB, Wiltshaw E,
Fisher C and McKinna JA: Ifosfamide is an active drug for
chemotherapy of metastatic cystosarcoma phyllodes. Cancer.
69:2271–2275. 1992. View Article : Google Scholar : PubMed/NCBI
|
|
31
|
Tse GM, Lee CS, Kung FY, Scolyer RA, Law
BK, Lau TS and Putti TC: Hormonal receptors expression in
epithelial cells of mammary phyllodes tumors correlates with
pathologic grade of the tumor: A multicenter study of 143 cases. Am
J Clin Pathol. 118:522–526. 2002. View Article : Google Scholar : PubMed/NCBI
|