Introduction
Renal oncocytoma is an uncommon tumor of the renal
parenchyma, accounting for ~4.3% of all solid renal masses
(1). It is composed of oncocytes,
which are uniform, round or polygonal neoplastic cells that exhibit
a granular eosinophilic cytoplasm (2). Despite certain manifestations of
malignancy, the majority of oncocytomas are considered to have a
benign behavior, with only a few reported cases of metastasis
(3). Based on morphological,
histochemical and pathological features, it is usually possible to
distinguish renal oncocytoma from other types of renal neoplasms;
however, in certain cases, overlapping phenotypes may pose a
challenge in the differential diagnosis of the disease (4). Renal oncocytoma usually has a benign
clinical course with excellent long-term outcomes; it has been
previously reported that disease-specific survival is 100% The
present study reports two cases of renal oncocytoma that were
successfully treated with laparoscopy. The clinical, radiographical
and pathological findings of the two cases are discussed in the
present study.
Case report
Case 1
A 60-year-old female patient presented to The First
Hospital of Jilin University (Changchun, China) in March 2012 with
a tumor in the right kidney, which was incidentally observed by
imaging modalities during a physical workup at our hospital. The
patient denied any history of hematuria, fever, weight loss or
other constitutional symptoms, but had a medical history of
hypertension and coronary heart disease. Physical examination and
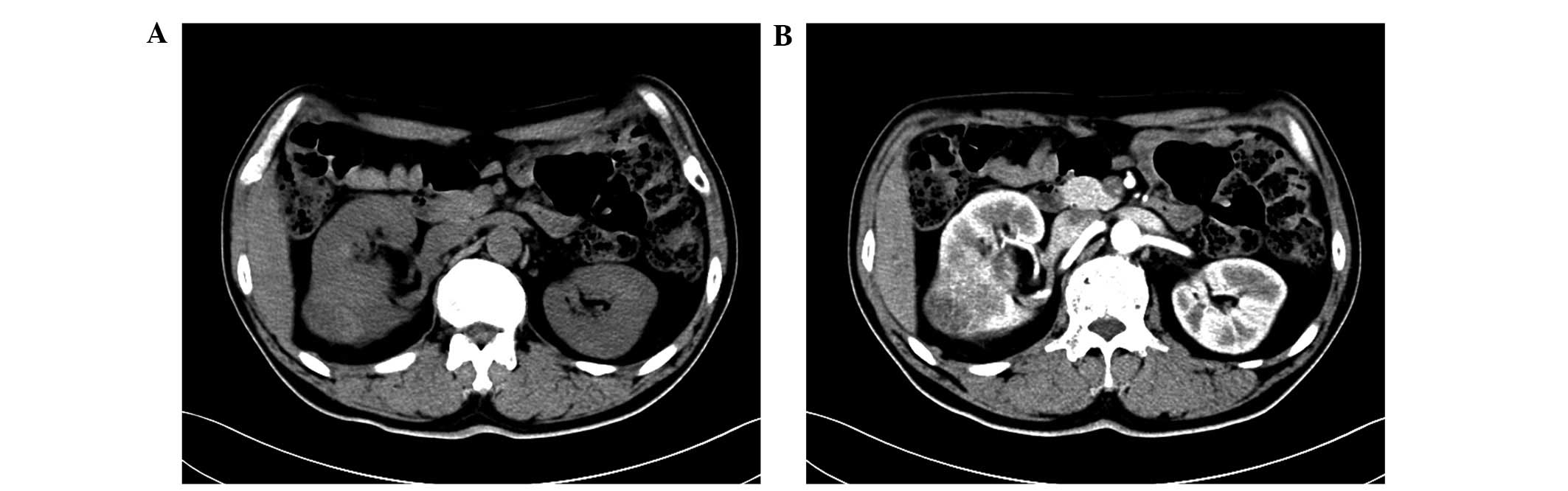
laboratory test results were unremarkable. Abdominal
ultrasonography demonstrated an ~4.5×5.3-cm solid, relatively
well-demarcated mass occupying the right kidney. Computed
tomography (CT; LightSpeed VCT; GE Healthcare Bio-Sciences,
Pittsburgh, PA, USA) revealed a 5.4×4.8 cm, heterogeneous and
markedly enhancing mass in the right kidney (Fig. 1). Chest X-ray, chest CT and bone scans
were all negative for metastasis. Based on the radiological
findings, laparoscopic radical resection of the right kidney was
performed to remove the tumor.
Macroscopic examination of the 12.0×6.0×4.5 cm
nephrectomy specimen revealed a 6.5×4.5×4.0 cm quasi-circular mass
in the middle of the right kidney adjacent to the renal hilum. The
cut section of the mass was tan-colored and light-textured.
Necrosis and hemorrhage were not observed. Tissues were sent to the
Department of Pathology, Sino-Japanese Friendship Hospital, Jilin
University (Changchun, China) to be fixed in 4% formaldehyde,
embedded in paraffin and cut into 5 µm sections. The specimens were
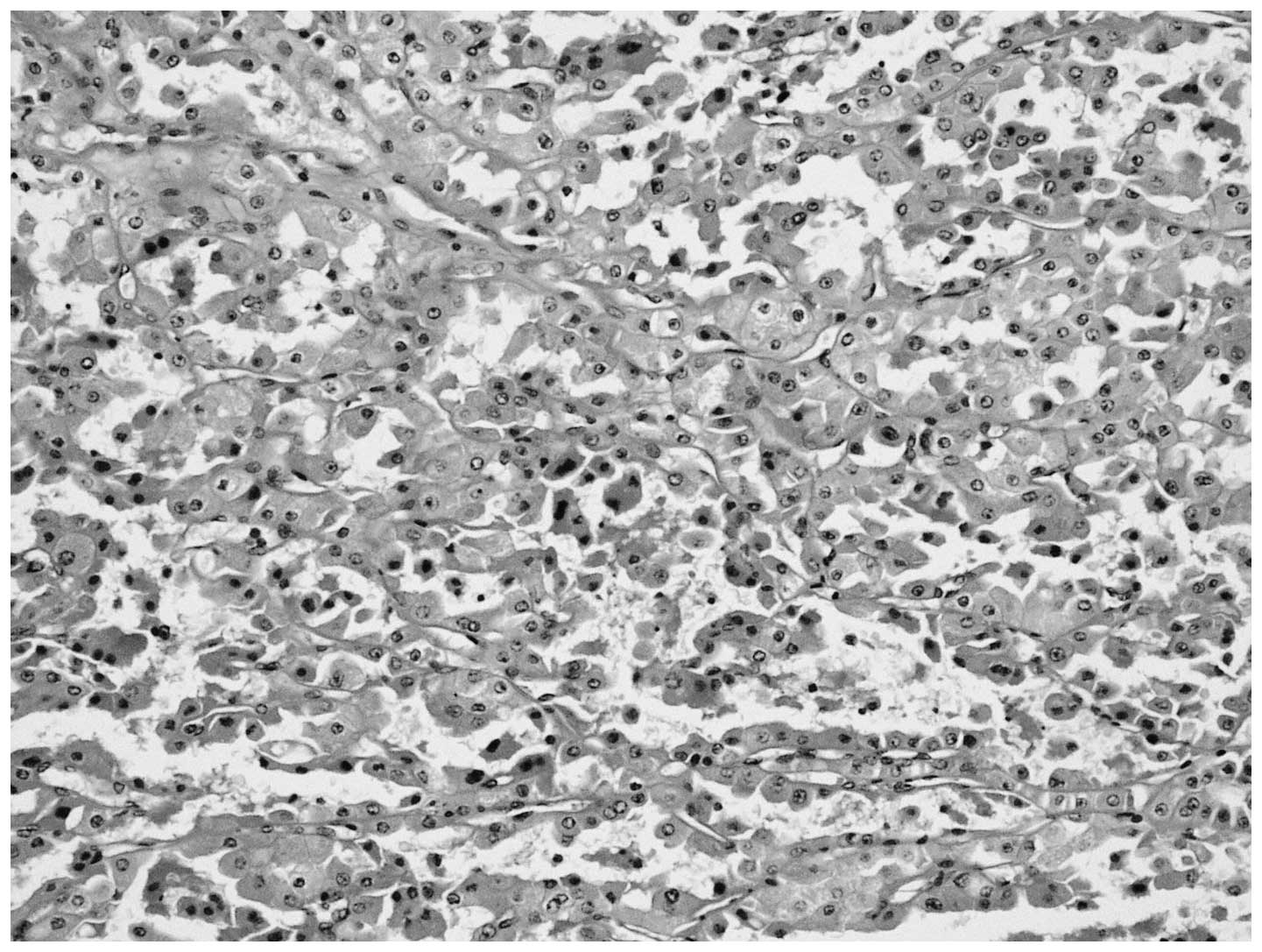
subsequently stained with hematoxylin and eosin. Histological
examination of the tumor samples revealed that the cells were round
and polygonal, which exhibited abundant granular eosinophilic
cytoplasm. Round or oval nuclei with a single centrally placed
nucleolus was noted, and focal necrosis was observed (Fig. 2). The cells did not exhibit any
cytological atypia and no mitotic figures were detected. For
immunohistochemical analysis, 4 µm sections were cut and placed on
slides coated with 3-aminopropyltriethoxysilane (Sigma-Aldrich, St.
Louis, MO, USA). The sections were then deparaffinized by routine
procedures and incubated in a microwave oven for 2X 5 min at 700 W
in citrate buffer (pH 6.0), or the specimens were predigested by
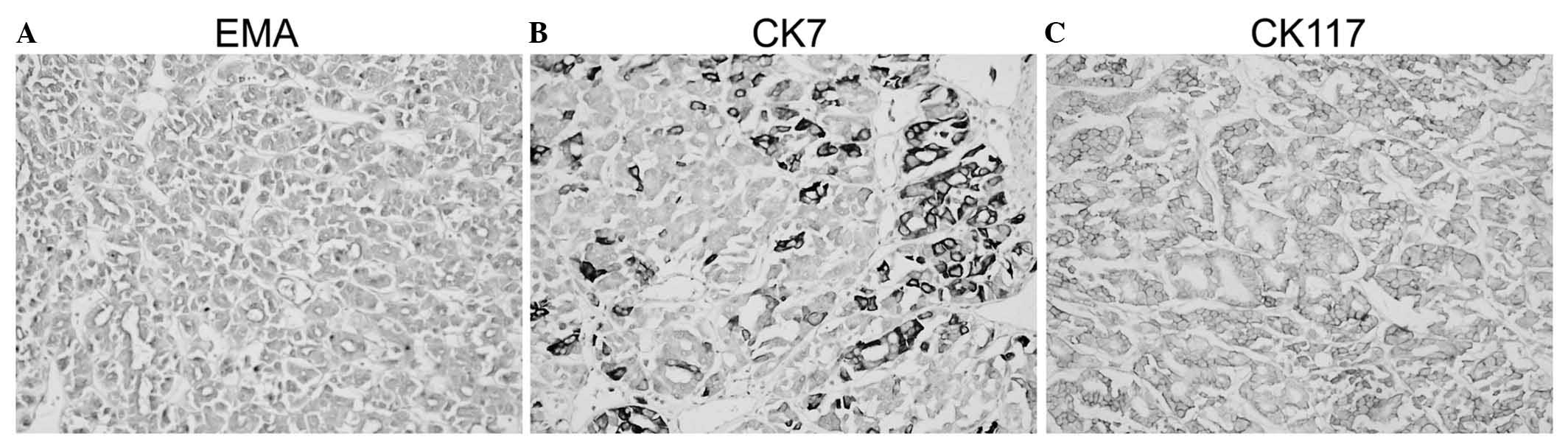
pepsin. The samples were incubated with the following primary
antibodies: Cytokeratin (CK)-7 (dilution, 1:200; Dako, Carpinteria,
CA), vimentin (dilution, 1:20; Immunotech, Marseilles, France),
epithelial membrane antigen (EMA; dilution, 1:50; Dako), CK18
(dilution, 1:50; Dako), CK117 (dilution, 1:100; Dako) and CK8
(dilution, 1:100; Dako). The primary antibodies were visualized
using the supersensitive streptavidin-biotin-peroxidase complex
(Biogenex, San Ramon, CA, USA). Immunohistochemical analysis
demonstrated that the tumor cells were positive for EMA, CK7 and
CK117, and negative for vimentin, P504S, inhibin A and cluster of
differentiation (CD) 10 (Fig. 3).
Nuclear positivity for Ki-67 was observed in <1% of tumor
cells.
Histopathological and immunohistochemical findings
confirmed the diagnosis of renal oncocytoma. The tumor was confined
to the kidney without lymphovascular invasion. Due to the final
diagnosis, neither chemotherapy nor radiation therapy were
administered postoperatively. The patient was discharged 8 days
following surgery. The patient was followed up every 3 months for 2
years, followed by semi-annual CT scans and laboratory tests. No
disease recurrence was observed at the 2-year follow-up.
Case 2
A 46-year-old male patient underwent an abdominal
ultrasound for the detection of renal function abnormalities at The
First Hospital of Jilin University (Changchun, China) in February
2012, which revealed a solid mass in the right kidney. No flank
pain or any other relevant clinical symptoms were noted. The
patient had a history of neurodermatitis and family history of
hypertension. A physical examination was normal and no renal mass
was observed. Routine laboratory tests revealed that the serum
creatinine level was 305.8 µmol/l (normal male range, 44–133
µmol/l; normal female range, 70–108 µmol/l), and there were
markedly elevated levels of blood urea nitrogen (11.76 mmol/l;
normal range, 3.2–6.0 mmol/l), uric acid (595 µmol/l; normal male
range, 149–416 µmol/l; normal female range, 89–357 µmol/l) and 24-h
urinary protein (3.39 g/24 h; normal range, <150 mg/24h). CT
revealed a heterogeneous lumpy mass that was not well-defined,
measured 4.2×3.0 cm and originated from the middle pole of the
right kidney. Due to the possibility of renal malignancy,
laparoscopic radical nephrectomy was performed.
Macroscopic examination revealed a 542 g mass
measuring 10.0×5.5×4.7 cm, brown in color, solid,
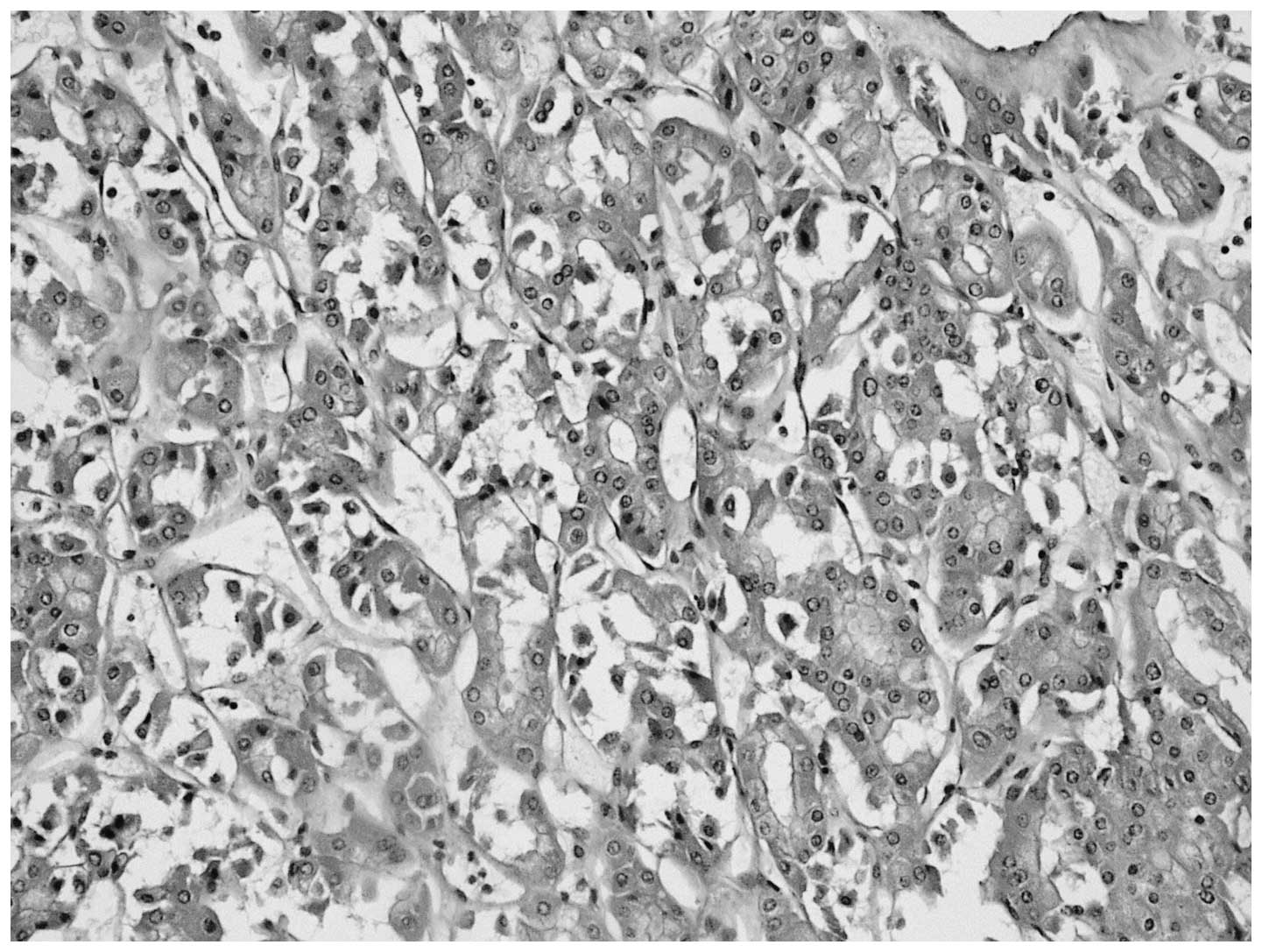
well-circumscribed and with no necrotic regions. Tumor samples were
prepared for histological and immunohistochemical analysis as
previously described in case 1. Histopathology lead to a diagnosis
of renal oncocytoma; the tumor was composed of polygonal oncocytes
exhibiting granular eosinophilic cytoplasm and round nuclei. There
was no evidence of necrosis or hemorrhage, and no vascular invasion
was observed (Fig. 4). The maximal
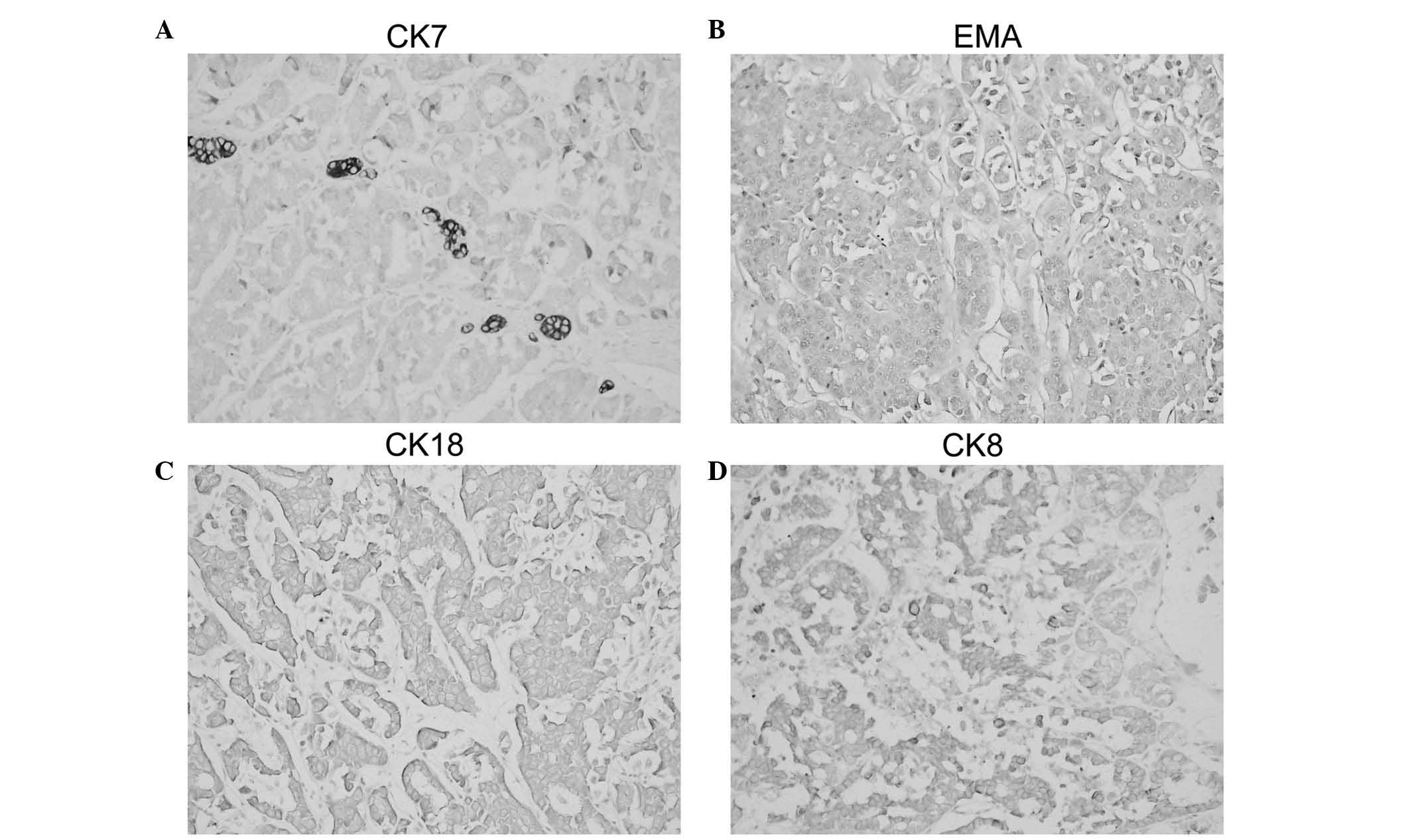
diameter of the tumor was 4 cm. Immunohistochemistry was positive
for CK7, EMA, CK18 and CK8, and negative for vimentin and CD10,
which additionally supported the initial diagnosis (Fig. 5). Nuclear positivity for Ki-67 was
observed in <1% of the tumor cells.
The postoperative course of the patient was
uneventful and the patient was discharged 7 days subsequent to
surgery. The patient was followed up every 3 months for 2 years,
followed by semi-annual CT scans and laboratory tests. There were
no signs of tumor recurrence at the 2 year follow-up.
Discussion
Renal oncocytoma is usually asymptomatic and is
observed incidentally during routine examination for non-urological
abnormalities. The peak occurrence age range is between 40 and 60
years, with a male/female ratio of 2/3:1 (5). Renal oncocytoma usually appears as a
solitary tumor measuring 4–8 cm; however, it may metastasize or
infiltrate peripheral renal tissues, causing the tumor to grow
larger (6,7). Only a few cases of metastases following
radical nephrectomy for oncocytoma have been reported (8). In the present cases, the tumors were
observed during routine examinations. No local invasion or distant
metastasis was observed in either of the two cases during 2 years
of follow-up.
Clinical and laboratory findings usually reveal no
specific characteristics, rendering a preoperative definitive
diagnosis challenging. CT may demonstrate the presence of a solid
homogeneous lesion with a centrally located scar, and arteriography
may reveal a spoke-wheel vascular pattern (5,9).
Immunohistochemical staining may aid in the differentiation of
oncocytoma from other renal tumors based on the levels of several
markers, including CD10, S100 calcium binding protein A1 and CK7
(10–12). However, these markers do not
definitively distinguish oncocytoma from other renal tumors. As a
result, numerous patients with oncocytoma are treated aggressively,
due to the possibility of renal malignancy.
Radical or partial nephrectomy is performed on the
majority of patients, based on their clinical circumstances.
Patients with tumors <4 cm in size that are located in the upper
or low pole of the kidney may be treated with a partial
nephrectomy, whilst all other patients require a radical
nephrectomy to be performed. However, considering the benign
behavior of these tumors, a that partial nephrectomy is a more
appropriate treatment option compared with radical nephrectomy
(8,13). In the present cases, laparoscopic
radical nephrectomy was performed due to the challenge in making an
accurate diagnosis.
In summary, the present study reported two cases of
renal oncocytoma, and demonstrates that renal oncocytoma should be
taken into consideration in the differential diagnosis of renal
tumors. The combination of clinical, radiological and
immunohistochemical features may assist lesion characterization,
but only histology can provide a definite diagnosis. Partial
nephrectomy is considered the most appropriate treatment for the
majority of patients with oncocytomas.
References
|
1
|
Morra MN and Das S: Renal oncocytoma: A
review of histogenesis, histopathology, diagnosis and treatment. J
Urol. 150:295–302. 1993.PubMed/NCBI
|
|
2
|
Alamara C, Karapanagiotou EM, Tourkantonis
I, Xyla V, Maurer CC, Lykourinas M, Pandha H and Syrigos KN: Renal
oncocytoma: A case report and short review of the literature. Eur J
Intern Med. 19:e67–e69. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
3
|
Perez-Ordonez B, Hamed G, Campbell S,
Erlandson RA, Russo P, Gaudin PB and Reuter VE: Renal oncocytoma: a
clinicopathologic study of 70 cases. Am J Surg Pathol. 21:871–883.
1997. View Article : Google Scholar : PubMed/NCBI
|
|
4
|
Koller A, Kain R, Haitel A, Mazal PR,
Asboth F and Susani M: Renal oncocytoma with prominent
intracytoplasmic vacuoles of mitochondrial origin. Histopathology.
37:264–268. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
5
|
Fan YH, Chang YH, Huang WJ, Chung HJ and
Chen KK: Renal oncocytoma: Clinical experience of Taipei Veterans
General Hospital. J Chin Med Assoc. 71:254–258. 2008. View Article : Google Scholar : PubMed/NCBI
|
|
6
|
Banks KL, Cherullo EE and Novick AC: Giant
renal oncocytoma. Urology. 57:3652001. View Article : Google Scholar : PubMed/NCBI
|
|
7
|
Ahmad S, Manecksha R, Hayes BD and
Grainger R: Case report of a symptomatic giant renal oncocytoma.
Int J Surg Case Rep. 2:83–85. 2011. View Article : Google Scholar : PubMed/NCBI
|
|
8
|
Romis L, Cindolo L, Patard JJ, Messina G,
Altieri V, Salomon L, Abbou CC, Chopin D, Lobel B and de La Taille
A: Frequency, clinical presentation and evolution of renal
oncocytomas: Multicentric experience from a European database. Eur
Urol. 45:53–57; discussion 57. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
9
|
Ciftci AO, Talim B, Senocak ME, Kaymaz F,
Cağlar M and Büyükpamukçu N: Renal oncocytoma: Diagnostic and
therapeutic aspects. J Pediatr Surg. 35:1396–1398. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
10
|
Avery AK, Beckstead J, Renshaw AA and
Corless CL: Use of antibodies to RCC and CD10 in the differential
diagnosis of renal neoplasms. Am J Surg Pathol. 24:203–210. 2000.
View Article : Google Scholar : PubMed/NCBI
|
|
11
|
Langner C, Ratschek M, Rehak P, Schips L
and Zigeuner R: CD10 is a diagnostic and prognostic marker in renal
malignancies. Histopathology. 45:460–467. 2004. View Article : Google Scholar : PubMed/NCBI
|
|
12
|
Leroy X, Moukassa D, Copin MC, Saint F,
Mazeman E and Gosselin B: Utility of cytokeratin 7 for
distinguishing chromophobe renal cell carcinoma from renal
oncocytoma. Eur Urol. 37:484–487. 2000. View Article : Google Scholar : PubMed/NCBI
|
|
13
|
Dechet CB, Bostwick DG, Blute ML, Bryant
SC and Zincke H: Renal oncocytoma: Multifocality, bilateralism,
metachronous tumor development and coexistent renal cell carcinoma.
J Urol. 162:40–42. 1999. View Article : Google Scholar : PubMed/NCBI
|